Chapter 35 Supraorbital Approach Variants for Intracranial Tumors
Paramount to the success of these approaches is a thorough understanding of the anatomy, as they can be difficult for novice surgeons who do not have a solid grasp of microsurgical corridors and cranial base anatomy/compartments. Anatomically relevant is the orbital bone, since it forms the roof of the orbital cavity and a strategic part of the anterior floor of the skull base. The orbital ridge intersects with the zygomatic bone laterally and the ethmoid medially; the orbit is further contiguous with the anterior fossa and sphenoid bone. Consequently, it is an anatomic structure that is intimately associated with the orbital cavity and its structures, as well as with the intracranial region.1–5
The supraorbital craniotomy and its variants essentially provide a combined subfrontal–anterolateral microsurgical approach. Anatomic structures such as the anterior clinoid, sphenoidal plane, and sellar region are keys to this corridor extending toward the region of the sylvian fissure. Therefore, these anatomic structures are critical in planning any microsurgical trajectory to the anterior fossa floor, the middle fossa, the smaller wing of the sphenoid, and the sellar/parasellar region.1,6,7
Previous anatomic studies have critically evaluated anatomic corridors in this region and their utility in treating a variety of neurologic lesions; these studies have subsequently resulted in potential surgical alternatives. Such historical and fundamental contributions have been made by Durante, Krause, Frazier, Cushing, Heuer, Dandy, Yasargil, Brock and Dietz, Al-Mefty, Zabramski, and Perneczky. Although the supraorbital approach is not a new strategy (initially described by Frazier with his epidural approach described in 19138), technological innovations have enhanced its applicability. The introduction of new tools (e.g., endoscopy) and new approaches (i.e., orbital ridge osteotomy) has improved access to and visualization of cranial base lesions. Ultimately, neurosurgical and technological innovations have aimed to reduce morbidity under the concept of minimally invasive neurosurgery.9,10
Orbital Anatomy
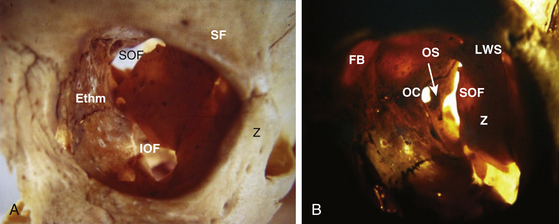
It is important to consider the orbital region as an anatomic compartment bound superiorly by the frontal bone, medially forming a close angle with the ethmoid bone, lacrimal bone, and lacrimal fossa. In addition, there are connections to the nasal region.11–14
In the inferior medial region we find the adjacent palatine bone and in the lower border the maxillary bone, where the infraorbital foramen is located. Going towards the midlateral inferior region, we find the area of the zygomatic bone which in turn extends through the zygomatic arch towards the posterolateral aspect, and going in an anterolateral location we find the facial zygomatic foramina. In the internal cavity of the orbital region the origin of the great wing of the sphenoid in its posterolateral portion is found—giving way to a virtual space between the small wing and the great wing of the sphenoid, known as the superior orbital fissure. Adjacent to the posterior medial portion are the optic canal located inferiorly and the inferior orbital fissure.2,15
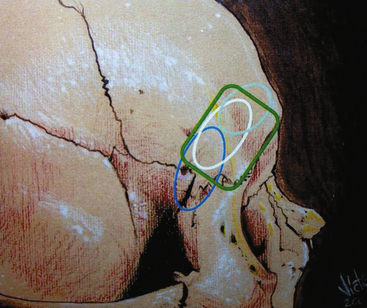
The posterosuperior orbital cone is made of the superior margin of the orbital fissure and the extension of the small wing of the sphenoid. The intracavitary foramina are the lacrimal foramen, the optic canal, the superior orbital fissure, the inferior orbital fissure, and in the extracavitary portion we find the notch or foramen for the infraorbital nerve and the orbital zygomatic foramen (Fig. 35-1).12
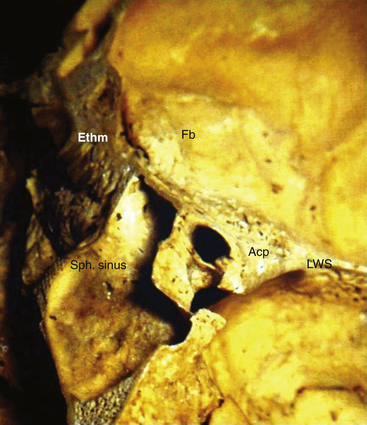
The optic canal and the anterior clinoid process are closely located and associated with the origin of the small wing of the sphenoid bone; the superior orbital fissure is divided by a bone strut (optic strut) supporting the anterior clinoid process. The most important structures involved in this region looking above (from the intracranial frontal floor perspective) are the anterolateral floor or the platform and the orbital arch. Toward the anterior medial portion, the crista galli and the cribriform plate of the ethmoid bone are found. The sphenoid plane and the wing of the sphenoid that meets the optic foramen are located in the deep plane (Fig. 35-2).16,17
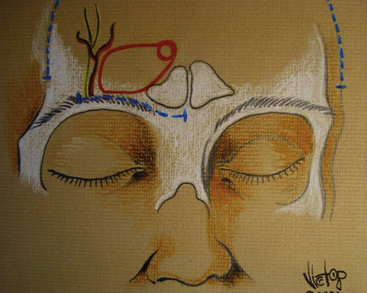
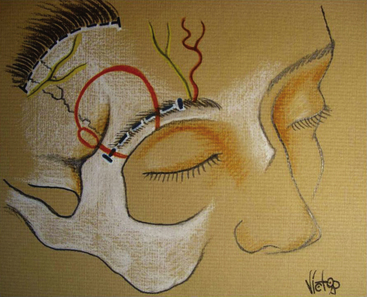
The anatomic intraorbital structures are basically represented by the extraocular muscles, predominantly the rectal and medial and lateralis muscles, such as the levator muscle for eye movement. We also find the periorbital fat or periorbit and the globe itself, the optic nerve, and other nerve structures from the ophthalmic branch of the trigeminal nerve, such as the frontal, nasociliary, and lacrimal nerves. The rest of the ocular motor nerves—III, IV, and VI—converge in a particular anatomic site after passing through the cavernous sinus (Fig 35-3).16
The most important arterial structures are the ophthalmic artery, its variants in the lacrimal artery and its connections to the ciliary artery, and the central retinal artery, whose venous return flows through the ophthalmic vein. The anterior ethmoidal artery is a significant vessel in the anteromedial region. It is closely related with the nasolacrimal region and the irrigation of the nasal mucosa, frequently managed in surgical procedures to control nose bleeds.11,14,18–22
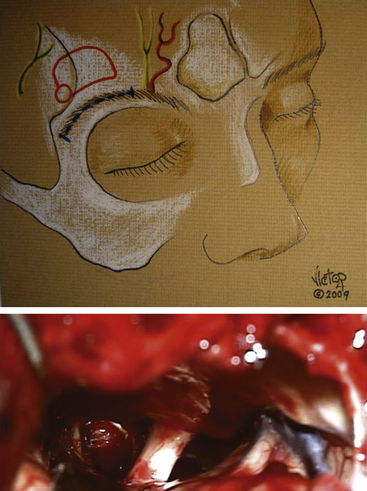
This specific anatomy gives way to the possibility of removing the orbital roof to have wide access to all the orbital area and ocular contents, nerve structures, muscles and vessels, and additionally have an intracranial access. An important anatomic structure from the surgical perspective is the lacrimal gland, located in the superior external area of the orbit. This is a region that can be compromised when using a surgical approach where the orbital roof is removed.12
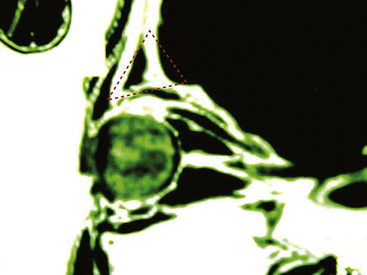
From the surgical perspective as well, it is important to emphasize the orbital surgical triangle, represented by a geometric figure that, from its lateral projection, the base is the anterior part of the frontal bone and the orbital arch, the upper part is outlined by the base of the frontal lobe, and the inferior part is outlined by the periorbit.13 This triangle, with an anterior base and a posterior vertex may offer several options for deep resection (also representing the angle of bone removal described in the trans-supraorbital approach; Fig. 35-4).5,23
Experimental Analysis of the Supraorbital Approach in Cadavers
A series of cadaver specimens were studied in order to assess the variations described for the supraorbital craniotomy in order to evaluate the extent of surgical access in identifying different anatomic landmarks. The conventional supraorbital keyhole approach was used to examine the optic nerve, ipsilateral anterior clinoid, sphenoidal plane, and the dorsum sellae. This approach, compared with the trans-supraorbital approach, showed some benefit with regard to accessibility and visualization.24–28
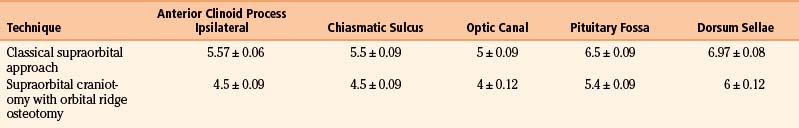
Subsequently, possible variants of this approach were analyzed in another experimental cadaveric study. In a series of 15 adult skulls, the differences between anatomic targets and the space around the sellar region were evaluated for these variants. Access to the following regions was assessed: the anterior clinoid process (ipsilateral), the chiasmatic sulcus, the optic canal, the center point of the sella turcica, and the dorsum sellae. Table 35-1 presents measurements for the classical supraorbital approach versus the supraorbital craniotomy combined with removal of the orbital arch.
Recognizing that the approach can be tailored, the craniotomy can be extended in different anatomic directions specific to the target pathology/region. For example, the supraorbital nerve can be mobilized in order to create a craniotomy more towards the midline. This modified approach facilitates a more comfortable and direct route to the prechiasmatic region, as well as other structures such as the crista galli, ethmoid lamina, olfactory bulb, sphenoidal plane, and anterior clinoid.10,27–32
On the other hand, lateral extension, as with the supraorbital-pterional approach, permits greater pterional access. This modification permits greater access to the lateral targets in the frontotemporal neurosurgical corridor and their neurovascular structures.10,27,32
Finally, if the principles of minimally invasive surgery and skull base surgery are combined, using the supraciliary incision, it is possible to remove the orbital arch in a block in the medial and lateral portion which provides an average of 1.5 cm more space to work in the craniotomy site, according to the anatomic studies of the trans-supraorbital approach.22,33
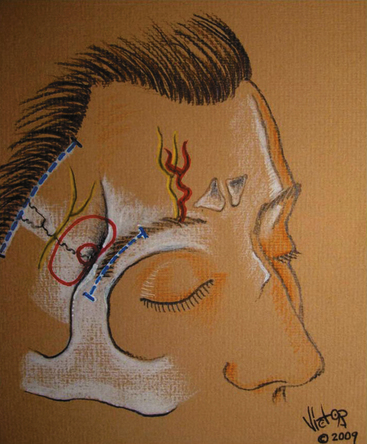
All of these variations of the supraorbital approach provide greater versatility and several possible adaptations to meet the surgical goal under the concept of supraselective craniotomy, which is the fundamental basis of the “keyhole” craniotomy. There are four basic variants of the supraorbital approach (Fig. 35-5):
Intracranial Surgical Access and its Variants
The development of finer, more accurate, and angled instruments has been critical for success of the supraorbital approach and its variants. Likewise, a major breakthrough was the use of the surgical microscope complemented with endoscopy-assisted microneurosurgery. The concept of keyhole microsurgery set forth by Perneczky was based on this new technology that contributed to providing several new options. Although seemingly contradictory, keyhole cranial base surgery advocates maximal resection through the use of current surgical technology and methodology taking into consideration the patient’s condition and pathology. Thus, variations in the orbital approach itself have led to improved extension and use in various surgical spaces granting access to the most important accessible structures.27,32–39
Synonymous with the development of keyhole surgery has been the increasing acceptance of using smaller incisions, such as the eyebrow incision. The use of smaller incisions can have cosmetic, functional, and even psychological benefits for the patient. However, this fact should not limit the final surgical plan in view of the surgical goal. For example, a displaced frontal scalp flap/craniotomy can also be chosen to apply the principle of selective craniotomy. In other words, minimally invasive surgery does not simply mean a minimal incision or minicraniotomy; instead, the goal is to spare craniofacial and neurovascular structures using a tailored approach as broad as necessary and as selective as experience allows, with every possible manipulation of a conventional procedure.36,40–48
For example, disadvantages of the brow approach can include frontalis weakness that occurs as a result of damage to the frontal branch of the facial nerve or the potential posterior alopecia of the eyebrow. Another advantage of this approach is preservation of the temporalis muscle in comparison to other antero-lateral based approaches (i.e., pterional). Even with lateral extension of this approach, the soft tissue dissection only involves minimal mobilization of the superior and anterior most aspect of the temporalis—in this process the deep neurovascular supply is preserved.40,47
Patient Positioning
One of the most significant factors in supraselective approaches is patient positioning as part of the operative plan. It is crucial to consider not only the surgical plan, but also the general and neurovascular anatomy of the patient. The effect of gravity and potential brain shift as a result of positioning may provide patient benefits by creating comfortable and wide access.11,45
Consequently, is important to consider not only elevating the head above the chest in every case to facilitate the venous return but also retroflexing and rotating the head according to the surgical plan.46,49 One of the goals is to have a three-dimensional view that gives full access to the surgical target with the least possible retraction, considering the conventional anatomic spaces promoted by cisternal drainage and subarachnoid dissection—fundamental microsurgical principles.24
Supraorbital Variants
Basic Access through the Eyebrow
Meticulous planning places the incision lateral to the supraorbital foramen extending to the area of the frontozygomatic suture. The skin flaps are retracted with elastic holding sutures. After exposing the muscles of the area, the frontalis muscle is sectioned sharply parallel to the orbital rim after which dissection of the orbicularis and the frontotemporal insertion of the temporalis muscle are also completed. Subsequently, the burr hole is made with high-speed drill, inferiorly to the temporal line, and use any of the variants described in the following.36,41,50
Medial Supraorbital Approach
In selected cases, this approach basically provides access to the subfrontal region, the medial gyrus rectus, the anterior interhemispheric portion, and medial bone annexa such as the cribriform region, olfactory sulcus, and nasolacrimal region.11,15,21,24 This corridor gives access to several tumors in this area, including the basal interhemispheric region, the genu and rostrum of the corpus callosum, and the proximal pericallosal space. Direct access to the cribriform basal region and the olfactory nerves is provided (crista galli, olfactory groove, planum sphenoidale, tuberculum sellae, lamina terminalis, anterior third ventricle, pituitary stalk, anterior communicating artery, and dorsum sellae).8,16,21,28,44,46,49–54
An inconvenience of this approach is the decision to plan entry into the frontal sinus (unless the frontal sinus is reduced in size) and the potential external mobilization of the supraorbital nerve to obtain a totally medial access. Infection and fistula from the frontal sinus access should be seriously considered as risk factors for this procedure. Nevertheless, when closure of the dura is meticulous and careful, the frontal sinus is cleaned thoroughly, and specific antibiotics are used, the procedure can be done without any problem (Fig. 35-6).14,24,45,53
Classic Supraorbital Approach (Laterobasal)
The classic supraorbital approach—also called the fronto-lateral-basal approach—is the classic technique described by Perneczky. From this supraorbito-lateral corner, access is obtained to the frontobasal region, sylvian fissure, and mesial temporal lobe. This approach provides such anatomic access due to the fundamental microsurgical principle of cerebrospinal fluid drainage via opening cisterns.10,35
This approach provides access to: the orbital roof, anterior clinoid process, posterior clinoid process, the roof and lateral wall of the cavernous sinus, the basal portion of the frontal lobe, gyrus rectus, sylvian fissure, temporal lobe, uncus, hippocampus, and cranial nerves of all this neurovascular corridor including CN1, CNII, CNIII, and CNIV; and extensions of the internal carotid artery, middle cerebral artery, and posterior cerebral artery in their proximal segments (ICA, Opht A, PCoA, AChA; perforators A1, A2, Mi, M2, P1, P2, SCA; and temporal vein) (Fig. 35-7). 10,12,21,51–53,55
Supraorbito-Pterional Approach
This keyhole approach was created to achieve the angle of vision and advantages of the classic pterional approach. This surgical approach is based on the anatomic location of the sphenoid ridge and its relationship with the sylvian fissure and basal cisterns. The initial incision is made over the hairline behind the external border of the eye on the selected side, because the cosmetic outcome is better compared with an eyebrow incision. A skin and muscular flap is reflected anteriorly, and a small 3 × 3–cm craniotomy is completed around the external landmarks of the sphenoid ridge. Further extradural drilling is completed down to the anterior clinoid process. The dura is opened in a semilunar manner, and the sylvian fissure is opened completely to reach the sylvian and basal cisterns. Of course, if we consider that the actual microsurgical space is 20 mm, this approach gives the same benefits as the conventional pterional approach and the benefits of the access through the trans-sylvian corridor, for a well-outlined craniotomy at the usual extension of the dural opening (Fig. 35-8).56
Trans-Supraorbital Approach
With the conventional technique, a 3-cm incision is made through the eyebrow between the median line of the pupil and the external rim of the zygomatic-orbital joint.25,26 In selected cases, the approach can be made through a fronto-temporal skin incision close to the hairline, to prevent scarring in the eyebrow or a cosmetic compromise from weakness in the frontal branch of the facial nerve. After incision, the orbicularis muscle is dissected. Once the tissues are mobilized with elastic retraction, an en-bloc craniotomy is performed with the following borders: median line–supraorbital foramen; external line–the zygomatic-orbital joint; and in the lower border–the orbital arch and 1-cm extension into the depth of the orbital roof until the intracranial portion is found. An en-bloc resection is made at the superior margin of the frontal 1.5-cm craniotomy, after removing the periosteum and protecting the orbital fat. The orbital bone is drilled with different boundaries and choices according to the surgical target. This procedure allows us to work in the intraorbital space, the intracranial–extradural space, and the intracranial–subarachnoid space.25,26
Once the drilling of the inner edges of the craniotomy is completed, the dura mater is opened under the microscope and the appropriate microsurgical corridor is dissected. The trans-supraorbital approach provides access to the entire sellar region and its neurovascular structures, providing enough space for surgical manipulation in cases of pituitary tumors with extrasellar extension to the optic chiasm. In selected cases, endoscopy has been used39–49 (Aesculap, Ventriculoscope, Tuttlingen, Germany, 0 and 30 degrees) to confirm patency of neighboring arteries, explore the intrasellar space and cavernous extension of the tumor, and finally, evaluate the pituitary stalk and sellar diaphragm (Fig. 35-9).3,4,25,26,33,39,57
Benefits and Limitations
One of the main advantages of the minimally invasive concept used in neurosurgery is that it involves a strategy that preserves the anatomic integrity of all structures, insofar as is possible, using a supraselective tailored approach. The latter should correlate specifically with the surgical target.3,4,25–28,33,50 Therefore, the approach does not entail a reductionist or minimalist vision, but rather one based on experience to find the proper balance in the design and size of the craniotomy aimed at achieving the surgical goal without subjecting the patient to unnecessary risk from tissue manipulation.
A practical example is shown by the historical progression from initially using large craniotomies to clip elective aneurysms to current use of tailored approaches. This progression is based on two basic principles. First, considering that microsurgery involves a 20-mm work space, it was concluded that resorting to greater exposure with the craniotomy was not strictly necessary (the evolution of a wide frontotemporal craniotomy to the pterional craniotomy). Second is inclusion anatomic integrity in the surgical plan, not only of cerebral structures with less retraction and manipulation, but also to preserve the craniofacial structures as well (avoiding atrophy of the temporal muscle, temporomandibular dysfunction, bone defects, fistula, flap necrosis, etc.).5,10,36,47,48,58
Thus, minimally invasive neurosurgery is not a discipline but a neurosurgical concept that may result in less morbidity due to the rational use and support of technology as part of the armamentarium and current multidisciplinary options used for the patient’s benefit.38 That is the reason why serious complications can result with a limited understanding of the principles of minimally invasive approaches and an overuse of technological support. Critical analysis of surgical experience accumulated thus far has demonstrated that major complications with minimally invasive approaches can occur if microsurgical principles are not properly followed. The key is to maintain a proper balance between overexposure and limited/reduced exposure. A crucial principle to obtain optimal outcome is that the selected approach must always allow performance of possible and necessary procedures, with conventional technology as support to facilitate the desired surgical goal with comfort and safety. Therefore, it is about correct planning—taking into account the patient’s specific anatomy and disease as well as variables related to the availability and pertinent use of certain technologies, and finally the skills and ability of the neurosurgical team.
Brock M., Dietz H. The small frontolateral approach for the microsurgical treatment of intracranial aneurysms. Neurochirurgia (Stuttg). 1978;21:185-191.
Cohen A.R., Perneczky A., Rodziewicz G.S., Gingold S.I. Endoscope-assisted craniotomy: approach to the rostral brain stem. Neurosurgery. 1995;36:1128-1129. discussion 1129-1130
Davies H.T., Neil-Dwyer G., Evans B.T., Lees P.D. The zygomatico-temporal approach to the skull base: a critical review of 11 patients. Br J Neurosurg. 1992;6:305-312.
Delashaw J.B.Jr., Tedeschi H., Rhoton A.L. Modified supraorbital craniotomy: technical note. Neurosurgery. 1992;30:954-956.
Delfini R., Raco A., Artico M., et al. A two-step supraorbital approach to lesions of the orbital apex. Technical note. J Neurosurg. 1992;77:959-961.
Jane J.A., Park T.S., Pobereskin L.H., et al. The supraorbital approach: technical note. Neurosurgery. 1982;11:537-542.
Jho H.D. Orbital roof craniotomy via an eyebrow incision: a simplified anterior skull base approach. Minim Invasive Neurosurg. 1997;40:91-97.
Noguchi A., Balasingam V., McMenomey S.O., Delashaw J.B.Jr. Supraorbital craniotomy for parasellar lesions. Technical note. J Neurosurg. 2005;102:951-955.
Ramos-Zuniga R. The trans-supraorbital approach. Minim Invasive Neurosurg. 1999;42:133-136.
Ramos-Zuniga R., Velazquez H., Barajas M.A., et al. Trans-supraorbital approach to supratentorial aneurysms. Neurosurgery. 2002;51:125-130. discussion 130-131
Raza S.M., Boahene K.D., Quinones-Hinojosa A. The transpalpebral incision: its use in keyhole approaches to cranial base brain tumors. Expert Rev Neurother. 2010;10:1629-1632.
Raza S.M., Garzon-Muvdi T., Boaehene K., et al. The supraorbital craniotomy for access to the skull base and intraaxial lesions: a technique in evolution. Minim Invasive Neurosurg. 2010;53:1-8.
Reisch R., Perneczky A. Ten-year experience with the supraorbital subfrontal approach through an eyebrow skin incision. Neurosurgery. 2005;57:242-255. discussion 242-255
1. Hendryk S., Czecior E., Misiolek M., et al. Surgical strategies in the removal of malignant tumors and benign lesions of the anterior skull base. Neurosurg Rev. 2004;27:205-213.
2. Jho H.D., Ha H.G. Endoscopic endonasal skull base surgery: part 1—the midline anterior fossa skull base. Minim Invasive Neurosurg. 2004;47:1-8.
3. Raza S.M., Boahene K.D., Quinones-Hinojosa A. The transpalpebral incision: its use in keyhole approaches to cranial base brain tumors. Expert Rev Neurother. 2010;10:1629-1632.
4. Raza S.M., Garzon-Muvdi T., Boaehene K., et al. The supraorbital craniotomy for access to the skull base and intraaxial lesions: a technique in evolution. Minim Invasive Neurosurg. 2010;53:1-8.
5. Steiger H.J., Schmid-Elsaesser R., Stummer W., Uhl E. Transorbital keyhole approach to anterior communicating artery aneurysms. Neurosurgery. 2001;48:347-351. discussion 351-352
6. Cappabianca P., Alfieri A., de Divitiis E. Endoscopic endonasal transsphenoidal approach to the sella: towards functional endoscopic pituitary surgery (FEPS). Minim Invasive Neurosurg. 1998;41:66-73.
7. Couldwell W.T., Weiss M.H., Rabb C., et al. Variations on the standard transsphenoidal approach to the sellar region, with emphasis on the extended approaches and parasellar approaches: surgical experience in 105 cases. Neurosurgery. 2004;55:539-547. discussion 547-550
8. Frazier C. An approach to the hypophysis through the anterior cranial fossa. Ann Surg. 1913;1:145-150.
9. Cushing H. Technical methods of performing certain cranial operations. Surg Gynecol Obstert. 1908;6:227-246.
10. Perneczky A., Fries G. Endoscope-assisted brain surgery: part 1—evolution, basic concept, and current technique. Neurosurgery. 1998;42:219-224. discussion 224-225
11. Jane J.A., Park T.S., Pobereskin L.H., et al. The supraorbital approach: technical note. Neurosurgery. 1982;11:537-542.
12. Jho H.D. Orbital roof craniotomy via an eyebrow incision: a simplified anterior skull base approach. Minim Invasive Neurosurg. 1997;40:91-97.
13. Losken H.W., Pollack I.F., Singhal V.K. Vascularized fronto-orbital advancement. J Craniofac Surg. 1996;7:107-110.
14. McCutcheon I.E., Blacklock J.B., Weber R.S., et al. Anterior transcranial (craniofacial) resection of tumors of the paranasal sinuses: surgical technique and results. Neurosurgery. 1996;38:471-479. discussion 479-480
15. Davies H.T., Neil-Dwyer G., Evans B.T., Lees P.D. The zygomatico-temporal approach to the skull base: a critical review of 11 patients. Br J Neurosurg. 1992;6:305-312.
16. Durante F. Esterpazione di un tumore endocranio (form morbosa prima e dopo l’operazione). Boll Accad Med Roma. 1885;11:247-252.
17. Evans J.J., Hwang Y.S., Lee J.H. Pre- versus post-anterior clinoidectomy measurements of the optic nerve, internal carotid artery, and opticocarotid triangle: a cadaveric morphometric study. Neurosurgery. 2000;46:1018-1021. discussion 1021-1023
18. Jho H.D., Alfieri A. Endoscopic endonasal pituitary surgery: evolution of surgical technique and equipment in 150 operations. Minim Invasive Neurosurg. 2001;44:1-12.
19. Kabil M.S., Eby J.B., Shahinian H.K. Fully endoscopic endonasal vs. transseptal transsphenoidal pituitary surgery. Minim Invasive Neurosurg. 2005;48:348-354.
20. Kabil M.S., Shahinian H.K. Application of the supraorbital endoscopic approach to tumors of the anterior cranial base. J Craniofac Surg. 2005;16:1070-1074. discussion 1075
21. Kabil M.S., Shahinian H.K. The endoscopic supraorbital approach to tumors of the middle cranial base. Surg Neurol. 2006;66:396-401. discussion 401
22. Kawamata T., Iseki H., Ishizaki R., Hori T. Minimally invasive endoscope-assisted endonasal trans-sphenoidal microsurgery for pituitary tumors: experience with 215 cases comparing with sublabial trans-sphenoidal approach. Neurol Res. 2002;24:259-265.
23. Shanno G., Maus M., Bilyk J., et al. Image-guided transorbital roof craniotomy via a suprabrow approach: a surgical series of 72 patients. Neurosurgery. 2001;48:559-567. discussion 567-568
24. Delashaw J.B.Jr., Tedeschi H., Rhoton A.L. Modified supraorbital craniotomy: technical note. Neurosurgery. 1992;30:954-956.
25. Ramos-Zuniga R. The trans-supraorbital approach. Minim Invasive Neurosurg. 1999;42:133-136.
26. Ramos-Zuniga R., Velazquez H., Barajas M.A., et al. Trans-supraorbital approach to supratentorial aneurysms. Neurosurgery. 2002;51:125-130. discussion 130-131
27. van Lindert E., Perneczky A., Fries G., Pierangeli E. The supraorbital keyhole approach to supratentorial aneurysms: concept and technique. Surg Neurol. 1998;49:481-489. discussion 489-490
28. Zheng X., Liu W., Yang X., et al. Endoscope-assisted supraorbital keyhole approach for the resection of benign tumors of the sellar region. Minim Invasive Ther Allied Technol. 2007;16:363-366.
29. Adant J.P., Bluth F. Endoscopic supraorbital nerve neurolysis. Acta Chir Belg. 1999;99:182-184.
30. Heuer G. Surgical experiences with an intracranial approach to chiasmal lesions. Arch Surg. 1920:368-381.
31. Tzortzidis F., Bejjani G., Papadas T., et al. Craniofacial osteotomies to facilitate resection of large tumours of the anterior skull base. J Craniomaxillofac Surg. 1996;24:224-229.
32. Wang H.S., Kuo M.F. Supraorbital approach of the anterior cerebral artery: a new window for transcranial Doppler sonography. J Ultrasound Med. 1995;14:259-261.
33. Raveh J., Turk J.B., Ladrach K., et al. Extended anterior subcranial approach for skull base tumors: long-term results. J Neurosurg. 1995;82:1002-1010.
34. Casler J.D., Doolittle A.M., Mair E.A. Endoscopic surgery of the anterior skull base. Laryngoscope. 2005;115:16-24.
35. Cohen A.R., Perneczky A., Rodziewicz G.S., Gingold S.I. Endoscope-assisted craniotomy: approach to the rostral brain stem. Neurosurgery. 1995;36:1128-1129. discussion 1129-1130
36. Czirjak S., Nyary I., Futo J., Szeifert G.T. Bilateral supraorbital keyhole approach for multiple aneurysms via superciliary skin incisions. Surg Neurol. 2002;57:314-323. discussion 323-324
37. Fries G., Perneczky A. Endoscope-assisted brain surgery: part 2—analysis of 380 procedures. Neurosurgery. 1998;42:226-231. discussion 231-232
38. Matula C., Tschabitscher M., Day J.D., et al. Endoscopically assisted microneurosurgery. Acta Neurochir (Wien). 1995;134:190-195.
39. Schroeder H.W., Gaab M.R. Intracranial endoscopy. Neurosurg Focus. 1999;6:e1.
40. Knize D.M. Limited-incision forehead lift for eyebrow elevation to enhance upper blepharoplasty. Plast Reconstr Surg. 1996;97:1334-1342.
41. Kung D.S., Kaban L.B. Supratarsal fold incision for approach to the superior lateral orbit. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81:522-525.
42. Liu J.K., Decker D., Schaefer S.D., et al. Zones of approach for craniofacial resection: minimizing facial incisions for resection of anterior cranial base and paranasal sinus tumors. Neurosurgery. 2003;53:1126-1135. discussion 1135-1137
43. Liu J.K., O’Neill B., Orlandi R.R., et al. Endoscopic-assisted craniofacial resection of esthesioneuroblastoma: minimizing facial incisions—technical note and report of 3 cases. Minim Invasive Neurosurg. 2003;46:310-315.
44. Melamed I., Merkin V., Korn A., Nash M. The supraorbital approach: an alternative to traditional exposure for the surgical management of anterior fossa and parasellar pathology. Minim Invasive Neurosurg. 2005;48:259-263.
45. Menovsky T., Grotenhuis J.A., de Vries J., Bartels R.H. Endoscope-assisted supraorbital craniotomy for lesions of the interpeduncular fossa. Neurosurgery. 1999;44:106-110. discussion 110-112
46. Noguchi A., Balasingam V., McMenomey S.O., Delashaw J.B.Jr. Supraorbital craniotomy for parasellar lesions. Technical note. J Neurosurg. 2005;102:951-955.
47. Paladino J., Pirker N., Stimac D., Stern-Padovan R. Eyebrow keyhole approach in vascular neurosurgery. Minim Invasive Neurosurg. 1998;41:200-203.
48. Papay F.A., Stein J.M., Dietz J.R., et al. Endoscopic approach for benign tumor ablation of the forehead and brow. J Craniofac Surg. 1997;8:176-180.
49. Kaplan M.J., Jane J.A., Park T.S., Cantrell R.W. Supraorbital rim approach to the anterior skull base. Laryngoscope. 1984;94:1137-1139.
50. Wiedemayer H., Sandalcioglu I.E., Stolke D. The supraorbital keyhole approach via an eyebrow incision for resection of tumors around the sella and the anterior skull base. Minim Invasive Neurosurg. 2004;47:221-225.
51. Chandler J.P., Pelzer H.J., Bendok B.B. et al. Advances in surgical management of malignancies of the cranial base: the extended transbasal approach. J Neurooncol. 2005;73:145-152.
52. Chandler J.P., Silva F.E. Extended transbasal approach to skull base tumors. Technical nuances and review of the literature. Oncology (Williston Park). 2005;19:913-919. discussion 920, 923-925, 929
53. Delfini R., Raco A., Artico M., et al. A two-step supraorbital approach to lesions of the orbital apex. Technical note. J Neurosurg. 1992;77:959-961.
54. Feiz-Erfan I., Han P.P., Spetzler R.F., et al. The radical transbasal approach for resection of anterior and midline skull base lesions. J Neurosurg. 2005;103:485-490.
55. Reisch R., Perneczky A. Ten-year experience with the supraorbital subfrontal approach through an eyebrow skin incision. Neurosurgery. 2005;57:242-255. discussion 242-255
56. Fujitsu K., Kuwabara T. Zygomatic approach for lesions in the interpeduncular cistern. J Neurosurg. 1985;62:340-343.
57. Senior B.A., Ebert C.S., Bednarski K.K., et al. Minimally invasive pituitary surgery. Laryngoscope. 2008;118:1842-1855.
58. Brock M., Dietz H. The small frontolateral approach for the microsurgical treatment of intracranial aneurysms. Neurochirurgia (Stuttg). 1978;21:185-191.