Chapter 55 Supracondylar Humeral Fractures: Is Open Reduction and Internal Fixation or Primary Total Elbow Arthroplasty Better in Poor Quality Bone?
In young patients, open reduction and internal fixation (ORIF) with double-plate fixation is the gold standard for displaced intra-articular fractures of the distal humerus, regardless of comminution.1 This procedure, however, can be technically challenging even when excellent bone quality is present, and elbow stiffness, malunion, nonunion, failure of fixation, and ulnar neuropathy are common sequelae.1 In elderly patients, the complication rate is increased because of osteoporotic bone, metaphyseal comminution, poor soft-tissue quality, and limited tolerance for joint immobilization; this is important because although distal humeral fractures represent only a small proportion of adult upper extremity fractures, the incidence of osteoporotic fractures of the distal humerus is increasing.1,2 According to the Finnish National Hospital Discharge Register, the current trend in the number and incidence of osteoporotic fractures of the distal humerus in Finnish women aged 60 or older is increasing rapidly.3 The annual incidence of these types of fractures has escalated from 11 per 100,000 in 1970 to 30 per 100,000 in 1995 and 2000; the increase is greatest in the oldest age group (women > 80 years) where the age-specific incidence rates showed a nine-fold increase (8 in 1970 vs. 75 in 2000). These results (which reflect trends seen in Europe and North America) reinforce the need to identify the optimal type of treatment for comminuted distal humeral fractures in the elderly to reduce the risk for reoperation and maximize functional outcome and independence. It should also be pointed out that, in most studies on this topic, women predominate in a 5:1 or 6:1 ratio.
OPTIONS
Although semiconstrained TEA has been recognized as a standard treatment for the complications or failure of primary ORIF of intra-articular distal humeral fractures,4,5 the role of primary TEA in the setting of acute supracondylar humeral fracture is more controversial. Although the advantages are obvious, including immediate stability and enhanced rehabilitation, no requirement for bone grafting or concern for delayed or nonunion, and possibly shorter operative times, the longevity of the prosthesis in the increasingly active elderly population remains a concern. In a landmark study, Cobb and Morrey6 report a series of 21 elderly patients (mean age, 72 years) who had primary TEA for comminuted fractures of the distal humerus and described a 95% good or excellent result rate at a mean follow-up of 3.3 years with a reoperation rate of 5% (one elbow).6 Several other similar single-institution reviews have described remarkably similar results in smaller series.7–11 More recently, Frankle and colleagues12 performed a retrospective comparison of ORIF with TEA, and the Canadian Orthopaedic Trauma Society (COTS)13 conducted a randomized clinical trial comparing these two treatment methods in older individuals. Although there is now an increasing amount of data to guide the clinician in decision making for elderly patients with intrinsically poor bone quality who sustain an intra-articular fracture of the distal humerus, it must be emphasized that this is a technique restricted to older patients and is contraindicated for patients younger than 65 years unless there are special circumstances (i.e., preexisting elbow arthritis).
EVIDENCE
Outcome after Open Reduction and Internal Fixation
Although there is substantial evidence for the benefits of ORIF in younger patients with fractures of the distal humerus,1,2 the evidence is less clear in older patients because only retrospective studies with small numbers have been reported (Table 55-1).14–19 Several of these studies have suggested that the majority of elderly patients achieve good or excellent functional results with ORIF; however, critical analysis of these results indicates a large variability in outcome and less predictable results than optimal.
TABLE 55-1 Results of Open Reduction and Internal Fixation for Distal Humeral Fractures in Elderly Patients
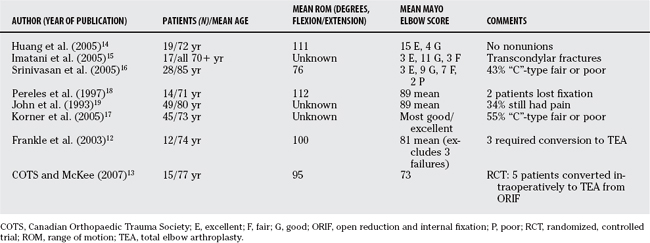
Huang and coauthors14 report on 19 patients with a mean age of 72 years who required ORIF for AO type “C” distal humeral fractures. They describe good results with no hardware failures, a mean range of flexion-extension from 17 to 128 degrees, with 15 excellent and 4 good results (according to the Mayo elbow score). Imatani and coworkers15 describe a technique in the Japanese population of using a small AO “T” plate for fixation of transcondylar fractures with good or excellent results in 14 of 17 patients older than 70 years. However, these “A”-type extra-articular fractures were not the more severe intra-articular injuries typically seen; results are usually worse in the “C”-type injuries. Srinivasan and researchers16 report their results of treatment with ORIF for “C”-type fractures in 21 patients with a mean age of 85 years (range, 75–100 years) and found 43% fair or poor outcomes. Korner and investigators17 report on the outcome of 45 patients with a median age of 73 years (range, 61–92 years) and a minimum follow-up of 2 years. Overall, 19 patients (42%) had a fair or poor outcome according to the Mayo elbow score. Fourteen of these patients (74%) had an AO/OTA type C fracture. In the subset of 29 patients with AO/OTA type C fractures, only 45% had an excellent or good outcome.17 Postoperative complications were recorded in 13 patients (29%), and revision surgery was required in 7 patients. Pereles and colleagues18 report more favorable results in 14 patients with a mean age of 71 years (mean Mayo elbow score, 89 points). John and coauthors19 reviewed the results of 49 patients with an average age of 80 years (range, 75–93 years) treated with ORIF of the distal humerus after a mean of 18 months.5 Twenty-eight fractures (57%) were classified as AO/OTA type C. Fair and poor functional results were observed in 26% of patients with an overall complication rate of 18%.19 Clearly, the results of ORIF for this type of fracture in the elderly do not match those seen for younger patients, especially for the more severe C-type fractures, and there is significant room for improvement.
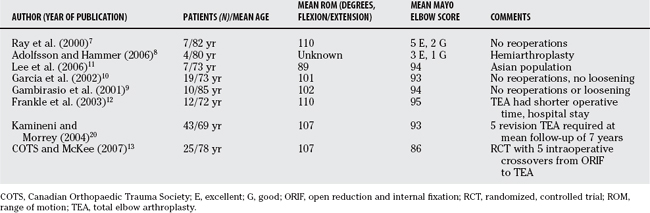
Outcome after Total Elbow Arthroplasty
Several studies suggest that semiconstrained TEA may have a role to play in the primary treatment of severe intra-articular distal humeral fractures (Table 55-2). Cobb and Morrey6 reported in 1997 their initial experience of primary TEA in 20 patients (21 elbows) with a mean age of 72 years (range, 48–92 years) and a mean follow-up of 3.3 years. A follow-up report on 43 patients was published in 2004 that revealed similar results. The mean flexion-extension arc was 24 to 131 degrees, and the mean Mayo elbow score was 93 points. Mean follow-up had increased to 7 years, although 9 elbows had required a total of 10 additional procedures, ranging from simple hematoma evacuation to revision arthroplasty for infection.20 Gambirasio and coworkers9 report the functional outcome at a minimum of 1 year for 10 women (mean age, 85 years) treated with primary TEA for a comminuted, intra-articular distal humeral fracture. Eight patients had an excellent outcome and two had a good outcome based on the Mayo elbow score.9 Garcia and colleagues10 evaluated 16 patients with a mean age of 73 years (range, 61–95 years) treated by primary TEA using the Coonrad–Morrey prosthesis at a mean follow-up period of 3 years (range, 1.5–5 years). No patients had inflammatory or degenerative arthritis of the elbow. OTA type C3 fractures were present in 11 patients. The mean DASH (a patient-based disability score) was 23 (range, 1–63), and the mean Mayo elbow score was 93 (range, 80–100).
Ray and colleagues7 describe good results in seven elderly (mean age, 82 years) women treated with semiconstrained arthroplasty for intra-articular distal humeral fractures.7 The mean range of motion was 20 to 130 degrees, and there were five excellent and one good results according to the Mayo elbow score. Lee and researchers11 report nearly identical results in seven elderly Asian women (mean age, 73 years).11
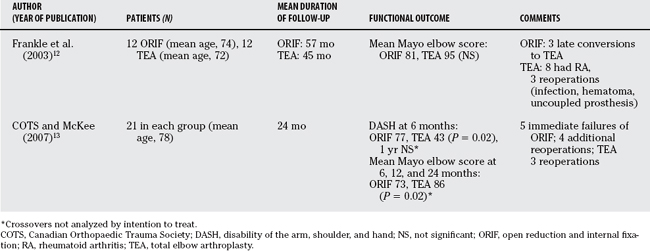
Comparative Studies
In one of the few comparative studies, Frankle and colleagues12 compared primary TEA versus ORIF for the treatment of distal humeral fractures in women older than 65 years (all comminuted type C fractures) (Table 55-3). They found that in the 12 patients in the TEA group, 11 had excellent results and 1 had good results; no fair and no poor results were reported.12 Notably, eight patients (67%) had associated rheumatoid arthritis. Three patients (25%) required subsequent operations, one to reconnect an uncoupled prosthesis, one to drain a postoperative hematoma, and one to débride a superficial infection. All of these complications resolved without subsequent sequelae, and no patient required revision implant surgery. The ORIF group had four excellent, four good, one fair and three poor results. The poor results were all salvaged by conversion to TEA (a difficult procedure with a high complication rate). The authors recommend primary TEA as a viable alternative in type C fractures of the distal humerus in elderly patients, especially in the setting of associated comorbidity such as rheumatoid arthritis, osteoporosis, and systemic steroid use.
In a study that has been presented at the 2007 Annual American Academy of Orthopedic Surgeons (AAOS) Meeting (J Shoulder Elbow Surg, accepted) the COTS randomized 42 elderly patients (mean age, 78 years) with comminuted intra-articular distal humeral fractures to either semiconstrained TEA (Coonrad–Morrey prosthesis) or conventional ORIF (two small fragment plates).13 Twenty-one patients were randomized to each group: one patient in each group died, and five patients randomized to ORIF had to be converted to TEA during surgery because of the inability to stably fix the fracture. This was anticipated and allowed as part of the study protocol. This left 25 patients in the TEA group and 15 patients in the ORIF group for evaluation. Despite the fact that the TEA group theoretically had worse injuries (by inclusion of the five most severe cases from the ORIF group), they had superior outcome, especially early. At 6 months, the mean DASH score in the TEA group was 43 versus 77 in the ORIF group (P = 0.02), although this difference was not statistically significant at 1 year (TEA vs. ORIF: 32 vs. 47; P = 0.10). The Mayo elbow scores were better in the TEA group at 6, 12, and 24 months (TEA vs. ORIF: 86 vs. 73, P = 0.015). The reoperation rate was not statistically different (TEA vs. ORIF: 3/25 [12%] vs. 4/15 [27%]; P = 0.20), although it must be remembered the TEA group included five patients who did not respond successfully to operative fixation. The authors’ conclusion was that TEA improved functional outcome compared with ORIF for these difficult fractures, and this was the treatment of choice, especially when comminuted, osteoporotic bone made fixation technically difficult. However, to date, only short-term results (2 years) are available, and these patients will require longer follow-up before establishing the ultimate superiority of replacement arthroplasty in this population.
AREAS OF CONTROVERSEY
Length of Follow-up
Prosthetic longevity is a significant concern whenever arthroplasty is used as a treatment for fracture. The mean life expectancy for a healthy North American woman aged 70 years is 15 more years. This is an important fact to remember, especially when one considers the increasingly active lifestyles (golf, tennis, etc.) of the modern retired population, and the increased demands that the prosthesis may experience. The majority of reports describing TEA for severe distal humeral fracture have follow-up that at best can be described as short term (2–5 years). The longest follow-up period in the literature is from Kamineni and Morrey’s20 2004 article, averaging 7 years.20 They describe five patients who required a revision arthroplasty; only one patient required revision in their original 1997 report that had a mean follow-up period of just more than 3 years. It is reasonable to assume that with longer follow-up more TEA patients will require revision. This emphasizes the fact that this procedure should be restricted to older (≥70 years) patients, and that a more sedentary lifestyle or at least some physical restrictions on elbow use is preferred.
Effect of Condylar Resection
The use of semiconstrained TEA for comminuted fractures of the distal humerus typically requires resection of the fracture fragments, which include the humeral condyles. Because the condyles serve as origin for the collateral ligaments, the common extensor origin and flexor-pronator mass, their resection could have a detrimental effect on a number of functions, including elbow stability and forearm and hand strength. McKee and coworkers’21 study examined the effect of condylar resection by comparing 16 total elbow arthroplasties with intact condyles versus 16 with resected or absent condyles.21 Comparing strength to the opposite normal arm in each patient, the authors found no difference in objectively measured hand, forearm, or elbow strength. Mayo elbow scores were also similar between the two groups (intact: 79; resected: 77), suggesting that practically, condylar resection did not have a clinically relevant effect on strength. It is important to note, however, that this study did not address the question of stability and longevity of the prosthesis after condylar resection.
Hemiarthroplasty versus Total Elbow Arthroplasty
Conventional wisdom dictates that the treatment of a severe distal humeral fracture by arthroplasty requires a semiconstrained total joint prosthesis to provide immediate stability and allow early motion. However, this mandates resection of a (usually normal) ulnar articulation, which may not be necessary. Some have advocated replacement of the fractured distal humerus alone with a hemiarthroplasty, in conjunction with a ligament repair or reconstruction. Adolfsson and Hammer8 provide a preliminary report on four elderly (mean age, 80 years) female patients with an unreconstructable distal humeral fracture treated with distal humeral hemiarthroplasty. The described excellent results in three and a good result in one. Although this technique has promise and does make some sense on a theoretical level (only replacing what is broken, potentially better longevity of the prosthesis), it should be considered experimental at the present time until further data are available.
Open Fractures of the Distal Humerus
Infection is a devastating complication for patients with an implanted elbow arthroplasty, and it should be avoided at all costs. For this reason, the presence of an open wound has been considered a relative, if not absolute, contraindication to TEA after supracondylar humeral fracture. However, although there is no specific article on this topic, some information is available that suggests it may be reasonable to perform primary TEA in the presence of an open wound. It is a question of some relevance because the fractures with an open wound tend to be of the more severe variety that makes ORIF difficult or impossible. Kamineni and Morrey20 describe two patients with grade I open wounds treated with immediate debridement and arthroplasty, and neither became infected; the COTS study had three similar cases treated in the same fashion, and none suffered any infectious complications.13
Although it appears that primary TEA in the presence of a grade I wound may be safe, it is important to emphasize proper technique. First, all the above cases were treated within 12 hours of injury: It may be prudent to temporize with patients presenting late for treatment. Second, the open wound tends to be posterior and is made as the condyles break away as the elbow hits the ground and the distal humeral shaft drives through the soft tissue and skin to impact the ground. Thus, although a thorough debridement and copious irrigation of the entire wound tract is mandatory, careful attention must be given to debriding and cleaning the distal humeral shaft and associated intramedullary canal, and antibiotics should be added to the cement.
Most of the literature on this topic consists of case series and retrospective reviews that describe the experience of single centers. Although there are some recent prospective and comparative studies, more high-quality studies are required before definitive statements can be made regarding ideal treatment methods. It must be remembered that with the techniques and implants currently available, ORIF remains the treatment of choice for the majority of these fractures including anyone younger than 65 to 70 years, extra-articular or partial-articular fractures, and simple-pattern complete articular fractures. In the setting of a complex, intraarticular fracture not amenable to stable fixation in an elderly (≥70 years) patient with osteoporosis, TEA has been shown to have significant advantages in terms of quicker rehabilitation, improved function, and a lower catastrophic failure rate compared with ORIF. Table 55-4 provides a summary of recommendations.
| RECOMMENDATION | LEVEL OF EVIDENCE/GRADE OF RECOMMENDATION |
|---|---|
ORIF, open reduction and internal fixation; TEA, total elbow arthroplasty.
1 McKee MD, Jupiter JB. Fractures of the distal humerus. In: Browner B, Jupiter J, Levine A, Trafton P, editors. Skeletal Trauma. 3rd ed. Philadelphia: Lippincott; 2002:765-782.
2 Sodergard J, Sandelin J, Bostman O. Postoperative complications of distal humeral fractures. 27/96 adults followed up for 6 (2-10) years. Acta Orthop Scand. 1992;63:85-89.
3 Palvanen M, Kannus P, Niemi S, Parkkari J. Secular trends in the osteoporotic fractures of the distal humerus in elderly women. Eur J Epidemiol. 1998;14:159-164.
4 Morrey BF, Adams RA. Semiconstrained elbow replacement for distal humeral nonunion. J Bone Joint Surg Br. 1995;77:67-72.
5 Morrey BF, Adams RA, Bryan RS. Total replacement for post-traumatic arthritis of the elbow. J Bone Joint Surg Br. 1991;73:607-612.
6 Cobb TK, Morrey BF. Total elbow arthroplasty as primary treatment for distal humeral fractures in elderly patients. J Bone Joint Surg Am. 1997;79:826-832.
7 Ray PS, Kakarlapudi K, Rajsejhar C, Bhamra MS. Total elbow arthroplasty as primary treatment for distal humeral fractures in elderly patients. Injury. 2000;31:687-692.
8 Adolfsson L, Hammer R. Elbow hemiarthroplasty for acute reconstruction of intra-articular distal humerus fractures. Acta Orthop. 2006;77:785-787.
9 Gambirasio R, Riand N, Stern R, Hoffmeyer P. Total elbow replacement for complex fractures of the distal humerus. An option for the elderly patient. J Bone Joint Surg Br. 2001;83:974-978.
10 Garcia JA, Mykula R, Stanley D. Complex fractures of the distal humerus in the elderly. The role of total elbow replacement as primary treatment. J Bone Joint Surg Br. 2002;84:812-816.
11 Lee KT, Lai CH, Singh S. Results of total elbow arthroplasty in the treatment of distal humeral fractures in elderly Asian patients. J Trauma. 2006;61:889-892.
12 Frankle MA, Herscovici DJr, DiPasquale TG, et al. A comparison of open reduction and internal fixation and primary total elbow arthroplasty in the treatment of intraarticular distal humerus fractures in women older than age 65. J Orthop Trauma. 2003;17:473-480.
13 Canadian Orthopaedic Trauma Society, McKee MD: A multicenter prospective randomized controlled trial of ORIF versus TEA for displaced intra-articular distal humeral fractures in elderly patients. Proceedings of the 2007 AAOS.
14 Huang TL, Chiu FY, Chuang TY, Chen TH. The results of open reduction and internal fixation in elderly patients with severe fractures of the distal humerus: A critical analysis of the results. J Trauma. 2005;58:62-69.
15 Imatani J, Ogura T, Morito Y, et al. Custom AO small T plate for transcondylar fractures of the distal humerus in the elderly. J Shoulder Elbow Surg. 2005;14:611-615.
16 Srinivasan K, Agarwal M, Matthews SJ, Giannoudis PV. Fractures of the distal humerus in the elderly: Is internal fixation the treatment of choice?. Clin Orthop Relat Res.; 434; 2005; 222-230.
17 Korner J, Lill H, Muller LP, et al. Distal humerus fractures in elderly patients: Results after open reduction and internal fixation. Osteoporos Int. 2005;16(suppl 2):S73-S79.
18 Pereles TR, Koval KJ, Gallagher M, Rosen H. Open reduction and internal fixation of the distal humerus: Functional outcome in the elderly. J Trauma. 1997;43:578-584.
19 John H, Rosso R, Neff U, et al. Distal humerus fractures in patients over 75 years of age. Long-term results of osteosynthesis. Helv Chir Acta. 1993;60(1-2):219-224.
20 Kamineni S, Morrey BF. Distal humeral fractures treated with noncustom total elbow replacement. J Bone Joint Surg Am. 2004;86A:940-947.
21 McKee MD, Pugh DM, Richards RR, et al. Effect of humeral condylar resection on strength and functional outcome after semiconstrained total elbow arthroplasty. J Bone Joint Surg Am. 2003;85-A(5):802-807.
22 Korner J, Diederichs G, Arzdorf M, et al. A biomechanical evaluation of methods of distal humerus fracture fixation using locking compression plates versus conventional reconstruction plates. J Orthop Trauma. 2004;18:286-293.