Chapter 63 Supracondylar Femoral Fractures: Is a Locking Plate or a Nail Better?
Supracondylar fractures of the femur have been a controversial topic over the years. As the literature indicates, the first attempt at minimally invasive surgery in this area was the intramedullary (IM) nail, first done antegrade, then later, more successfully, in a retrograde fashion.1 Although the union rate seemed improved with the IM nail, the number of malunions appeared to increase as the fracture type became more complex. Eventually, the technique for a minimally invasive dynamic condylar screw (DCS)2 and the advent of the locked plate with its minimally invasive tools and technique opened the door for biomechanical and prospective clinical studies to evaluate whether the increased cost of the new locked plate was associated with improved outcome.3–7
EVIDENCE
Are Plates Better Than Nails in Supracondylar Fractures of the Femur?
Christodoulou and colleagues11 examined the fixation methods of supracondylar fractures before the introduction of the locked plate. The objective of the study was to present the results of surgical management of supracondylar fractures of the femur (types A and C according to the Association for Osteosynthesis/Association for Research and Education Foundation [AO/ASIF] classification) in elderly patients with the use of two different methods of fixation: the mini open DCS fixation and the closed retrograde intramedullary nailing (RIN). Eighty patients with supracondylar fractures of the femur were treated from January 1994 to June 2000, and 72 of them followed up completely. The authors conclude that although the two methods appear to have the same percentage of excellent results and same time to bony union, RIN is preferable to DCS in terms of less blood loss and shorter operating time (Fig. 63-1).
Hartin and coauthors12 studied the blade plate and the IM nail used in the treatment of supracondylar femoral fractures. The condylar blade plate relies on the principles of open reduction, absolute stability, and interfragmentary compression to achieve union. The technique of retrograde nailing uses indirect reduction of the metaphyseal fracture component, offering relative stability and a less invasive approach. Twenty-two patients with 23 supracondylar femur fractures were recruited from two regional trauma centers over a 26-month period and randomized to receive either a retrograde IM nail fixation (12 fractures) or a fixed-angle blade plate fixation (11 fractures). Both distal femoral nailing and blade plating gave good outcomes. There was a trend for patients undergoing retrograde nailing to report more pain and to require revision surgery for removal of implants.
Biomechanical Data on Nails versus Plates
Koval and investigators5 performed a biomechanical cadaver study to compare the stability of three standard distal femoral fixation techniques. After initial mechanical characterization of intact femurs, a distal femoral osteotomy was created, reduced, and stabilized under compression using random assignment to one of three methods of fixation: (1) 6-hole 95-degree supracondylar plate; (2) retrograde inserted, statically locked, supracondylar IM nail; and (3) antegrade inserted, statically locked Russell–Taylor nail.
Koval and investigators4 report on the biomechanical properties of the locked plate compared with the standard condylar buttress plate. The locked buttress plate provided significantly greater fixation stability than the standard plate both before and after cycling in axial loading. The locked buttress plate also proved significantly more stable in axial loading than the blade plate both before and after cycling. The authors conclude that a condylar buttress plate with locked screws improves fixation stability.
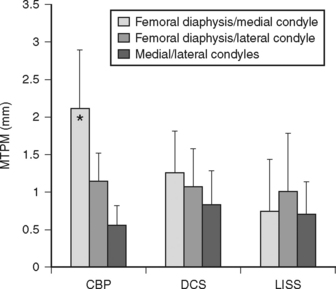
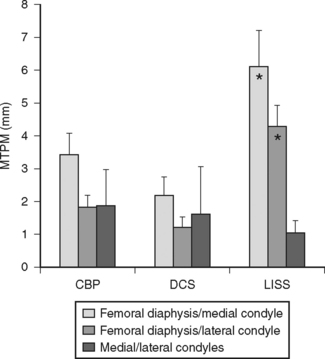
Duffy and colleagues13 also studied the biomechanical characteristics of the DCS, standard condylar buttress plate, and the limited invasive stabilization system (LISS). Both of these studies indicate the locked plate (LISS) was indeed stronger than the other two standard devices. Duffy and colleagues’13 study used radiostereometric analysis to measure micromotion between bone segments. Permanent deformation was measured after cyclic axial loading, and elastic deformation was measured during a static load. The LISS plate proved to be more flexible and allowed some motion, which may explain the clinical impression of more exuberant callous formation at the fracture site (Figs. 63-2 and 63-3).
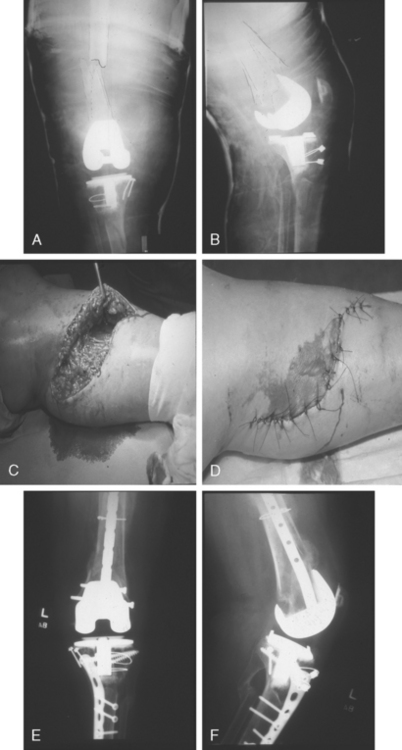
Prospective cohort studies suggest that the biomechanical properties of the locked plate seem to hold up clinically, although there are as yet no published prospective RCTs to compare implants. Fankhauser and coworkers3 used the LISS to treat 30 distal femoral fractures in 29 patients. They found the LISS to be a safe and effective treatment. Schutz and researchers6 managed 112 patients with 116 distal femoral fractures in a prospective multicenter study. All fractures were treated with the LISS plate. The study had a 93% follow-up rate with the follow-up period ranging from 7 to 33 months. The study showed that with a sound knowledge of the operative technique and careful preoperative planning, the LISS represents an excellent, safe procedure for the treatment of almost all distal femoral fracture types including periprosthetic fractures of the distal femur, generally without the need for primary cancellous bone grafting. Locked plates have also demonstrated good results in the treatment of difficult fractures such as AO33 types A and C in patients with multiple trauma injuries with soft-tissue damage7 (Fig. 63-4) and periprosthetic supracondylar femur fractures.14
Ly and coworkers15 presented data at the Orthopaedic Trauma Association (OTA) general meeting indicating that, in a review of their last 124 supracondylar fractures treated in a standard nonlocked fashion, 20 were complicated by nonunion and required further surgical intervention to achieve union.
Large and colleagues16 also presented at the OTA meeting a study of lateral locked plating versus other operative techniques. The locked plate group had six malunions (24%) and no nonunions. The other group had nine malunions (47%) and three nonunions (16%). Both approached clinical significance but remain underpowered to date.
AREAS OF CONTROVERSY
IM nails, usually retrograde, are utilized in supracondylar fractures where the fracture is extra-articular or an undisplaced intra-articular fracture is present. Given this fracture type, if a locked nail allows for axial and varus-valgus stability, the outcomes are satisfactory. If the fracture type is periarticular (within 5 cm of the joint), a fixed-angle device placed via a limited invasive approach appears to be the preferred method. This appears to reduce the risk for a malunion. If the fracture includes only one condyle or is axially stable, a standard plate without locking screws performs as well as or better than other implants tested. If the fracture involves both condyles or is axially unstable, a locked plate appears to provide the best fixation in both biomechanical and in clinical studies. Table 63-1 provides a summary of recommendations for the treatment of supracondylar femoral fractures.
TABLE 63-1 Summary of Recommendations for the Treatment of Supracondylar Femoral Fractures
| RECOMMENDATIONS | LEVEL OF EVIDENCE/GRADE OF RECOMMENDATION |
|---|---|
1 Ostrum RF, Agarwal A, Lakatos R, et al. Prospective comparison of retrograde and antegrade femoral intramedullary nailing. J Orthop Trauma. 2000;14:496-501.
2 Krettek C, Schandelmaier P, Miclau T, et al. Minimally invasive percutaneous plate osteosynthesis (MIPPO) using the DCS in proximal and distal femoral fractures. Injury. 1997;28(suppl 1):A20-A30.
3 Fankhauser F, Gruber G, Schippinger G, et al. Minimal-invasive treatment of distal femoral fractures with the LISS (Less Invasive Stabilization System): A prospective study of 30 fractures with a follow up of 20 months. Acta Orthop Scand. 2004;75:56-60.
4 Koval KJ, Hoehl JJ, Kummer FJ, et al. Distal femoral fixation: A biomechanical comparison of the standard condylar buttress plate, a locked buttress plate, and the 95-degree blade plate. J Orthop Trauma. 1997;11:521-524.
5 Koval KJ, Kummer FJ, Bharam S, et al. Distal femoral fixation: A laboratory comparison of the 95 degrees plate, antegrade and retrograde inserted reamed intramedullary nails. J Orthop Trauma. 1996;10:378-382.
6 Schutz M, Muller M, Krettek C, et al. Minimally invasive fracture stabilization of distal femoral fractures with the LISS: A prospective multicenter study. Results of a clinical study with special emphasis on difficult cases. Injury. 2001;32(suppl 3):SC48-SC54.
7 Schutz M, Muller M, Regazzoni P, et al. Use of the less invasive stabilization system (LISS) in patients with distal femoral (AO33) fractures: A prospective multicenter study. Arch Orthop Trauma Surg. 2005;125:102-108.
8 Anwar IA, Battistella FD, Neiman R, et al. Femur fractures and lung complications: A prospective randomized study of reaming. Clin Orthop Relat Res. 2004:71-76.
9 Pape H-C, Grimme K, Van Griensven M, et al. Impact of intramedullary instrumentation versus damage control for femoral fractures on immunoinflammatory parameters: Prospective randomized analysis by the EPOFF Study Group. J Trauma. 2003;55:7-13.
10 Tornetta P3rd, Tiburzi D. Antegrade or retrograde reamed femoral nailing. A prospective, randomised trial. J Bone Joint Surg Br. 2000;82:652-654.
11 Christodoulou A, Terzidis I, Ploumis A, et al. Supracondylar femoral fractures in elderly patients treated with the dynamic condylar screw and the retrograde intramedullary nail: A comparative study of the two methods. Arch Orthop Trauma Surg. 2005;125:73-79.
12 Hartin NL, Harris I, Hazratwala K. Retrograde nailing versus fixed-angle blade plating for supracondylar femoral fractures: A randomized controlled trial. ANZ J Surg. 2006;76:290-294.
13 Duffy P, Trask K, Hennigar A, et al. Assessment of fragment micromotion in distal femur fracture fixation with RSA. Clin Orthop Relat Res. 2006;448:105-113.
14 Ricci WM, Loftus T, Cox C, et al. Locked plates combined with minimally invasive insertion technique for the treatment of periprosthetic supracondylar femur fractures above a total knee arthroplasty. J Orthop Trauma. 2006;20:190-196.
15 Ly TV, Bong MR, Hamid N, et al. Results of operative intervention of supracondylar femur fractures. Available at: http://www.hwbf.org/ota/am/ota06/otapo/OTP06020.htm. Accessed May 2008.
16 Large TM, Norton J, Bosse MJ, et al. Locked plating of supracondylar periprosthetic femur fractures. Available at: http://www.hwbf.org/ota/am/ota06/otapa/OTA060212.htm. Accessed.
17 Canadian Orthopaedic Trauma Society. Nonunion following intramedullary nailing of the femur with and without reaming. Results of a multicenter randomized clinical trial. J Bone Joint Surg Am. 2003;85-A:2093-2096.