CHAPTER 16 Supraclavicular block
Clinical anatomy
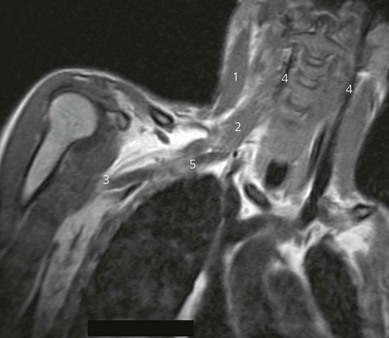
In the neck, the brachial plexus lies in the posterior triangle (Fig. 16.1), covered by the investing layer of deep cervical fascia, platysma, and skin. It is crossed by the supraclavicular nerves, the inferior belly of the omohyoid muscle, the external jugular vein, and the transverse cervical artery and vein. It emerges between the anterior scalene and middle scalene muscles; its upper part lies above the third part of the subclavian artery, while the lower trunk formed by the union of the eighth cervical and first thoracic nerve roots is placed behind the artery; the plexus next passes behind the clavicle.
Surface anatomy
Important landmarks for the supraclavicular block include the interscalene groove behind the posterior border of the sternocleidomastoid muscle, the clavicle, and the subclavian pulse (Fig. 16.2). The interscalene groove can be identified by placing a finger behind the sternocleidomastoid muscle and then rolling laterally. Maneuvers to help identify landmarks include asking the patient to flex their neck against resistance to identify the sternocleidomastoid muscle. Sniffing accentuates the scalene muscles. The groove can be followed toward the clavicle. The belly of the omohyoid muscle crosses the groove, and 1 cm above the clavicle the subclavian pulse is usually palpated. The external jugular vein crosses the interscalene groove and posterior border of the sternocleidomastoid muscle at the level of the cricoid cartilage. The needle insertion site is immediately posterior to the subclavian pulse.
Sonoanatomy
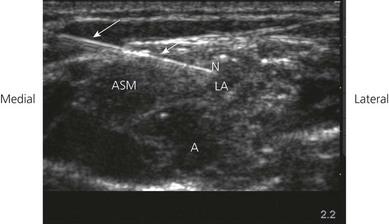
The ultrasound transducer should be held between the thumb, index and ring fingers of the non-dominant hand. Placing the little finger and ulnar aspect of the hand on the patient will stabilize the transducer. Firm even surface pressure with the ultrasound transducer usually produces the best images. Above the clavicle, the ultrasound transducer (38-mm linear array high frequency transducer) is oriented in a coronal oblique axis to the neck (Fig. 16.3). This is the transverse ultrasound transducer orientation. Such transverse imaging facilitates identification of nerves and associated relations. It also allows verification of circumferential spread of local anesthetic around nerves. A curvilinear transducer can also be used for this block. Perform a systematic anatomical survey from medial to lateral and superficial to deep.
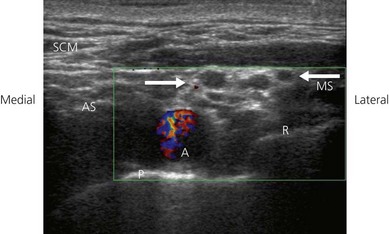
The supraclavicular ultrasound-guided technique focuses on the supraclavicular fossa, where the superior, middle, and inferior primary trunks divide into their anterior and posterior branches. The plexus runs superficially at this level, and high-frequency transducers are thus needed (10 MHz) to identify the relevant structures (Fig. 16.4). Technical difficulties are encountered in studying the supraclavicular region due to the presence of the supraclavicular depression, which complicates both manipulation of the ultrasound transducer and needle puncture. First locate the subclavian artery. Identify the hyperechoic first rib deep to the subclavian artery and its shadow beneath. Identify the pleura and air artifact beneath. This is different from the shadow beneath the first rib. The brachial plexus is found lateral and posterior to the subclavian artery. The subclavian artery and brachial plexus lie between the scalene muscles.
Technique
Landmark-based approach
A 35-mm 21-G insulated needle is used. The stimulating current is set at 1 mA, 2 Hz, and 0.1 ms. Needle orientation is caudad and parallel to the neck (Fig. 16.5). It is important to avoid any dorsomedial orientation. At a depth of 1–2 cm a fascial sheath is entered. The superior trunk of the brachial plexus is usually located first. The needle position is adjusted while decreasing the current to 0.35 mA with maintenance of the muscle response.
The response that results in the greatest block success is muscle contraction below the shoulder. Responses indicating incorrect needle locations include diaphragmatic contraction (the phrenic nerve lies on the anterior scalene – too anterior a position) and contraction of the posterior compartment muscles of the shoulder (suprascapular nerve stimulation – too posterior a needle position). Contact with the first rib may occur on deep needle insertion (Fig. 16.6). The subclavian artery lies within the brachial plexus fascial sheath and injection in its proximity will produce successful block. If the artery is entered initially, the needle is withdrawn and oriented dorsolaterally.

Figure 16.6 Supraclavicular block technique: deep insertion. The first rib may be contacted on deep insertion.
Incremental injection of local anesthetic is made with repeated aspiration. For this block, 40 mL of local anesthetic is adequate (Fig. 16.7).
Ultrasound-guided approach
Intravenous access, ECG, pulse oximetry and blood pressure monitoring are established. Maximized comfort for the operator and patient is an important step in pre-procedure preparation. For the ultrasound-guided supraclavicular block, the patient is placed in the supine position with the head turned to the side opposite that to be blocked. The operator stands or sits at the patient’s head, adjacent to the side to be blocked. The ultrasound screen, transducer, needle, and plane of imaging should all be placed in one view for the operator. For the supraclavicular block, the ultrasound screen is placed below the shoulder on the side to be blocked (Fig. 16.8). Room lights may be turned down to enhance image viewing. The operating lights can be used to maintain some working lighting in the background. The patient is asked to raise their head to identify the interscalene groove. The pulsation of the subclavian artery is palpated above the clavicle.
The skin is disinfected with antiseptic solution and draped. A sterile sheath (CIVCO Medical Instruments, Kalona, IA, USA) is applied over the ultrasound transducer with sterile ultrasound gel (Aquasonic, Parker Laboratories, Fairfield, NJ, USA). Another layer of sterile gel is placed between the sterile sheath and the skin. A skin wheal of local anesthetic is raised at a distance from the lateral aspect of the transducer to facilitate sterility and allow a shallow angle of approach to improve needle visualization. An alternate method of needle insertion for the supraclavicular block can be from the medial aspect of the ultrasound transducer. The needle bevel should face the active face of the transducer to improve visibility of the needle tip. A free-hand technique rather than the use of a needle guide is preferred. A 21-GA × 50-mm insulated needle (B. Braun, Bethlehem PA) is inserted parallel to the axis of the beam of the ultrasound transducer (Fig 16.9). For this approach, the operator can slide and tilt the transducer to maintain the needle tip within the plane of imaging as much as possible. The needle tip is slowly advanced under ‘real-time’ imaging until the needle reaches the side of the target neural structures (Fig 16.10). Manipulation of the transducer or redirection of the block needle may be necessary to bring the needle tip into the plane of imaging. Patients tolerate transducer manipulation better than needle redirection. The placement of the needle tip should be very superficial.
Once the needle tip has been confirmed by ultrasonography to lie in close proximity to the brachial plexus, this can be further confirmed by using a nerve stimulator (Stimuplex; B. Braun, Bethlehem PA). Characteristic motor activity in the forearm and hand is seen. Test injections for assessment of local anesthetic spread should be small (0.5 to 2 mL). If the local anesthetic spread is not seen on the ultrasound screen, the injection should be stopped. The needle is readjusted to allow complete encirclement of the brachial plexus with local anesthetic (Fig 16.10). Local anesthetic solution appears as a hypoechoic image. Typically, a decreased volume of local anesthetic is required compared to non-ultrasound-guided supraclavicular blocks.
Adverse effects
Clinical pearls
Chan VW, Perlas A, Rawson R, Odukoya O. Ultrasound-guided supraclavicular brachial plexus block. Anesth Analg. 2003;97(5):1514-1517.
Kapral S, Krafft P, Eibenberger K, et al. Ultrasound-guided supraclavicular approach for regional anesthesia of the brachial plexus. Anesth Analg. 1994;78(3):507-513.
Klaastad O, Smedby O. The supraclavicular lateral para vascular approach for brachial plexus regional anesthesia: a simulation study using magnetic resonance imaging. Anesth Analg. 2001;93:442-446.
Winnie AP. Plexus anesthesia, Vol. 1. Perivascular techniques of brachial plexus block. Copenhagen: Schultz; 1983.