CHAPTER 19 Superomedial Pedicle Breast Reduction Using a Vertical Pattern
Summary/Key Points
Introduction
Although the technique of vertical breast reduction was pioneered by Marchac1–3 and Lassus4–6 nearly three decades ago, it was popularized by Lejour7,8 in the 1990s and to the present day most notably by Hall-Findlay.9,10 The ability to utilize the vertical reduction skin pattern with a variety of pedicle options and to deliver a reliable and aesthetically pleasing breast shape is compelling support to have this operation in any plastic surgeon’s armamentarium. Part of the resistance to adopting this technique has been wound healing problems along the vertical scar and lower incisional puckering. Complications and need for revision are minimized by avoiding excessive cinching of the skin closure and by careful patient selection taking into account skin quality and estimated resection volume.
There has been an evolution throughout the senior author’s practice which has culminated in the current technique for vertical breast reduction. Early on, the majority of reductions were performed using the inferior pedicle and Wise pattern. The boxy postoperative shape and bottoming out of the breasts, led to dissatisfaction and interest in trying other techniques. After reviewing the experiences of Madeleine Lejour7,8 the notion of not relying on the skin envelope to shape the breast became an important concept in adapting the vertical technique to clinical practice. Multiple different pedicles were tried with the vertical skin pattern. First, the superior pedicle was used, and soon after abandoned in most cases due to difficulty folding large dense breasts that often resulted in significant drag on the areola. Second, the lateral pedicle was employed; however, this presented a limited opportunity for debulking the lateral aspect of the breast, the quadrant most often in need of debulking. The superomedial pedicle was the next choice and remains the first choice of pedicles when using the vertical technique (and even the Wise skin pattern). The ability to sculpt the pedicle and vary the lateral tissue resection affords great flexibility with this approach. In addition, utilizing a superomedial pedicle leaves the cleavage undisturbed and provides an attractive breast shape. There remain some instances where due to a patient’s anatomy, the superior pedicle is a better choice. These cases occur when there is minimal ptosis and superior migration of the nipple is a short distance. We have used the rule that if nipple elevation is less than 4 cm, a superior pedicle is chosen. We like the approach of Frank Lista who advocates using the superior pedicle if the existing nipple position is at or above the 6 o’clock mark on the keyhole.11
Patient Selection
The majority of women seeking consultation for breast reduction surgery are appropriate candidates. However, some may be declined surgery, not because of anticipated lack of symptom relief, but because they are at higher than acceptable risk for complications. The two main exclusion criteria for breast reduction surgery in our practice are obesity (body mass index, BMI > 35) and current smokers.12–14 There are instances where patients with significant obesity are considered for surgery; however, these exceptions are decided on a case by case basis. We have a smoking policy for all elective surgery performed in our section. Patients are required to be smoke free for a minimum of 4 weeks preoperatively. We check a urine cotinine test on the day of surgery in patients known to be smokers to confirm compliance with our smoking policy. If the test is positive, the case is cancelled. This is communicated well in advance given the inconvenience to the patient and the operating room schedule when this occurs.
Initial Consultation
When the initial consultation is booked, women are mailed an information package to review prior to the visit. This includes a brochure and informed consent on breast reduction developed by the American Society of Plastic Surgeons. Women are provided with several website addresses to further explore breast reduction surgery. A shared medical appointment model is used for the initial consultation in the majority of our patients.15,16 This model provides ample time for women to interact with nursing staff, the surgeon, and other patients, and to watch a 12 minute video production, all of which greatly enhances the informed consent process. The video details the procedure of breast reduction and emphasis is placed on the fact that there is no guarantee of a specific requested cup size and that surgery is best done at a realistic long-term stable weight. The video also describes alternate skin incisions, pedicle versus free nipple graft techniques, and the surgical risks. Photographs of excellent, average, and poor results are presented as are complications, including nipple necrosis. The evidence of this surgery on decreasing breast cancer risk is also communicated. The outpatient nature of the surgery, drains, postoperative recovery, and time required off work is reviewed.
As part of the shared medical appointment, individual examinations are performed. This includes recording of the following measurements: sternal notch to nipple distance (SN-N), IMF to nipple distance (IMF-N), the proposed new location of the nipple which is the IMF transposed to the anterior breast skin in line with the breast meridian, the anticipated elevation of the nipple, the distance from the superior areolar border to the proposed new nipple position, the degree of ptosis, the skin envelope quality/elasticity, the presence of shoulder grooves, palpable breast masses, scars, axillary rolls, and any rashes. Estimations are made of the volume of each breast as well as the anticipated resection given the patient’s desired final cup size. There are multiple techniques to estimate resection volume including mathematical formulas and water displacement however it is in the opinion of the senior author that the ability to predict resection volume comes with experience.17,18
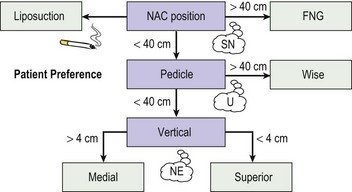
After the examinations are completed, a group discussion is held with the purpose of assisting each woman individually to decide the most optimal surgical approach. The patient is informed that with the vertical incision pattern, there is less scarring on the breast compared to the Wise pattern, but there may be a slightly greater risk for delayed healing and desire for scar revision, which is not likely covered by insurance. As a general guideline, patients with sternal notch to nipple distances less than 40 cm are candidates for one of the pedicle techniques (Fig. 19.1). In choosing the vertical pattern versus other patterns, we take into consideration the amount of resection as well as the patient’s skin envelope. Patients are informed that in resections over 1000 g, there is an increased risk of having a poor cosmetic result with the vertical technique and are thus advised to select the Wise pattern. However, should they have a strong preference for the vertical approach, they are counseled that this can be attempted with the flexibility of altering the plan intraoperatively to include a ‘J’ or a short ‘T’ conversion along the IMF. This part of the session generates many additional questions that help address the nuances of the surgical techniques and expectations for surgical outcomes.
As with all surgical decisions, they have to be customized to the patient. Our current algorithm is presented in Figure 19.1. In our practice, the vertical pattern and superomedial pedicle are used in 70% of all breast reduction cases. The following exceptions are necessary in select patients. The superior pedicle will be chosen if anticipated nipple–areola complex (NAC) elevation is small – less than 3–4 cm. In cases where there are pre-existing scars precluding the use of the superomedial pedicle, then usually an inferior pedicle is chosen with a Wise pattern. In patients with SN-N distances greater than 40 cm or with IMF-N distances greater than 20 cm, free nipple grafts are used with the Wise pattern. One caveat with using SN-N distance cutoffs: there are cases where the woman is willing to retain more volume than is typical. In this scenario, one can consider using a pedicle technique even with SN-N greater than 40 cm. If the patient requests to be as small as possible, then free nipple grafts may be necessary. In all breast reduction surgery, one must consider a woman’s expectations and her anatomy to arrive at the optimal choice.
Operative Technique
Part I: Preoperative markings
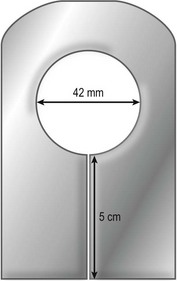
On the day of surgery, the following materials are needed to perform the markings: ruler, tape measure, keyhole pattern, and surgical skin marker (Fig. 19.2). The template we use is made from commonly available material in any operating room. It is made out of silicone sheeting (thickness 1.0 mm (0.04 inches)) or two sheets of foam tape. The areolar diameter is 42 mm and the vertical limbs are 5 cm. There are additional templated hash marks for the 3 and 9 o’clock positions along the keyhole.
There are seven key steps to focus on in the markings (Fig. 19.3): (1) breast meridian, (2) new nipple height, (3) vertical limbs, (4) keyhole pattern, (5) ghost patterns, (6) pedicle design, (7) recheck all markings, especially the pedicle for symmetry.



Fig. 19.3
The first four of the seven key steps in marking for a vertical breast reduction. A The breast meridian has been marked along the midportion of the gland (Key Step 1) and the ruler is in place along the old IMF to mark the new nipple height (Key Step 2). B The IMF has been marked on the right breast and the vertical limbs determined (Key Step 3). C The areolar outline has been marked (Key Step 4) using a silicone template depicted in Figure 19.2.
Key step #1: The breast meridian, the vertical representation of the central axis of the breast, is drawn from clavicle across the superior breast, inferior pole and across the ribcage (Fig. 19.3B). This line does not necessarily pass over the nipple. In patients with eccentric nipples, the breast meridian will not intersect with the nipple but may cross the areola.
Key step #2: Avoid using a standard SN-N length to set the new nipple position. The NAC should be placed at the level of the IMF. The IMF is transposed to the front of the breast as recommended by Gradinger,13 by positioning a flexible ruler along the IMF under the breast on one side and allowing the ruler to cross the midline on the anterior surface of the opposite breast (Fig. 19.3A). The IMF can thus be accurately translocated to the anterior breast surface. Potential pitfall: Although the senior author previously used the bimanual palpation technique to transpose the IMF, a technique that works nicely with the Wise pattern approach, this has a tendency to leave the planned position for the NAC too high on the newly created breast mound. A purposeful lowering of the NAC compared to Wise pattern markings must be made when using the vertical skin pattern approach.
To delineate the anatomic transition between the breast and axillary roll, the woman is asked to raise her arms above her head and the lateral breast boundary is marked (Fig. 19.4).
Key step #3: To delineate the vertical limbs of the keyhole pattern and thus the length of the medial and lateral flaps, the breast is rotated lateral and superior and the vertical axis of the meridian is transposed to the displaced medial breast tissue. In a similar fashion, the breast is rotated medial and superior, the meridian transposed, to delineate the lateral extent of skin resection (Fig. 19.3C). Surgeons new to this technique often find it difficult to master the tension used to rotate the breast in these maneuvers. Fahmy and Hemington-Gorse described a marking technique that some learners might find useful where the patient is marked on a level stretcher.19 In the supine position, the weight of the breast falling laterally delineates the medial vertical limb. In a partial lateral decubitus, the breast falling medially delineates the lateral vertical limb. Although we do not routinely use this technique, we offer it as a way to check the markings when learning how to design for the vertical breast reduction.
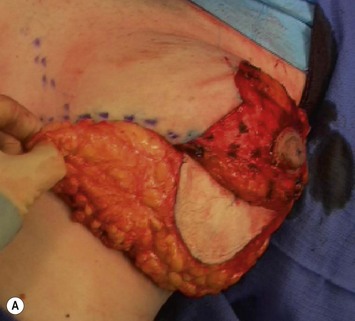
Key step #6: Finally, the superomedial pedicle is designed (Fig. 19.5). In order to teach residents this technique, we developed landmarks to help define the location of the pedicle. For the right breast the superior border of the pedicle begins at the 3 o’clock position. It curves around the areola and can be shortened by making this turn through the areola for very large areola. It then continues medially to end at the 5 cm mark on the medial vertical limb. The opposite pedicle design is performed for the left breast. A typical pedicle length measured intraoperatively from halfway along the medial vertical limb to the end of the planned pedicle ranges from 7–10 cm.
Key Step #7: Check all markings for symmetry (Fig. 19.6). We typically check the following discrete measures: sternal notch to top of areola distance, the distance between the 6 o’clock positions of the areola, the pedicle length and width, the maximum distance between the medial and lateral vertical limbs or in cases with asymmetry – the lengths of the medial and lateral flaps.
Potential challenges in designing the skin incisions are patients whose areola extends past the medial or lateral vertical limbs or patients who have a very medially located areola. In the first scenario, the pigmented areolar skin is visible past the designated marks for the medial and lateral limbs of the keyhole pattern. There are two approaches to utilize when faced with this challenge – the first is to rotate the keyhole pattern so that instead of it being perpendicular to the IMF it is rotated so that the incisions include the pigmented skin of the areola. The other approach is to curve the vertical limbs to incorporate the pigmented skin. For example, if the medial limb needs to curve towards the midline to exclude leaving areola outside of the planned incision, then the lateral limb needs to be curved to parallel the altered medial limb design. In addition to the skin pattern design challenge, a medially located NAC will frequently lead to an extremely short pedicle. In cases like this, it might make more sense to do one of the other pedicles such as inferior pedicle or lateral pedicle. In patients with particularly large areola, another way to customize the markings is to consider the circumvertical technique.20 Conceptually, rather than taking up all the excess skin in the vertical incision as the classic vertical breast reduction does, the gathering can be done around the areola as well as in the vertical incision. Hammond has also perfected his own version of this technique in the SPAIR mammoplasty by gathering the majority of the excess skin in the periareolar region.21,22
Part III: Operative technique
Preparation
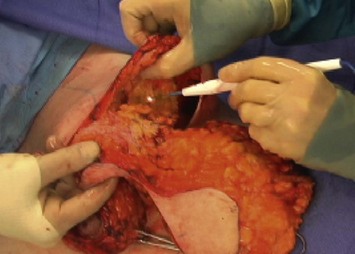
Once the glandular resection has been completed (Fig. 19.11), the specimens are weighed and compared. The residual breast tissue is checked for symmetry by cupping the remaining pedicle in each hand to estimate volume and by palpating the superior flap and the lateral flap for equivalent thickness. If there is uncertainty about symmetry while the patient is still supine, temporary skin closure with staples is performed and the head of the bed elevated to a semi-sitting position, and the breasts re-evaluated.
A variation of the box stitch described by Frank Lista is performed in the deep dermal layer.11 This stitch is composed of a figure of 8 placed along the vertical closure to aid in skin eversion and to avoid splitting knots. 4-0 PDS is used for deep dermal stitches along with the subcuticular closure around the areola and vertical incisions. Care is taken to start the vertical closure 1 cm below the junction with the areola to minimize the risk for a tear-drop deformity. The subcuticular closure of the vertical incision is a slight modification of the usual approach (see section on delayed wound healing below for further details).
Mindful control of the resulting inferior dog ear can be achieved in numerous ways. Our preferred technique involves two steps. First, after skin closure, closed suction is applied while compressing the inferior loose skin to the chest wall. Second, a Xeroform bolster is placed over the lower end of the vertical incision and taped into place. The first piece of tape is applied tension free to secure the Xeroform to the skin. Two more pieces of tape are placed mimicking the position of an underwire medially and laterally (Fig. 19.12). Gauze fluffs are then placed over the breasts followed by a surgical bra. Illustrative cases are shown in Figures 19.14 and 19.15.
Potential Pitfalls
Roll along the IMF
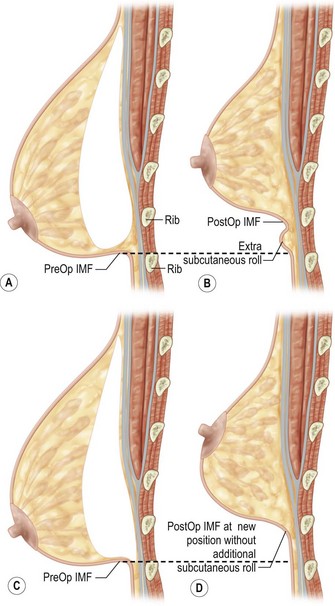
Unlike other techniques for breast reduction, the vertical approach elevates the IMF. It is therefore imperative to perform an adequate resection between the new IMF and the old IMF. There is a tendency for the learner to scoop out the tissue towards the IMF failing to keep an even thickness of the inferior flap and failing to carry the resection to and slightly past the IMF. Some surgeons target this area with liposuction and may not have any issues with a residual roll. If the glandular tissue below the new IMF is under-resected, the residual tissue produces a palpable and visible roll between the new and old IMF. This can be prevented by defatting the inferior pole skin down to chest wall with a slight rim of subcutaneous tissue on the chest wall at the IMF (Fig. 19.13).
Need for surgical revision
As for any surgery, if problems arise, surgical revision may become necessary.23 We have found that the majority of surgical revisions when appropriate and desired, can be performed in the minor surgery suite in our office under local anesthetic. The typical problem is residual skin excess along the IMF. The usual approach is to excise the excess tissue using a horizontal ellipse. We have become more adept at detecting intraoperatively which patients may need this ‘conversion’ and are more liberal with intraoperative ‘J’ extensions or ‘T’ extensions. If there is volume asymmetry, our preferred approach is liposuction. This can be somewhat challenging in a previously operated breast and the use of a power assisted liposuction device is helpful.
Conclusion
Vertical breast reduction is an excellent option for moderate reductions in patients with good skin quality. The flexibility of resection volumes and pedicle options make this a versatile procedure. The technique is readily learned by our residents each year. Optimal breast shape is achieved with less scarring than traditional methods. Patient satisfaction is high and with attention to patient selection and technical details, complication rates are low.23,24
1 Marchac D, Sagher U. Mammaplasty with a short horizontal scar. Evaluation and results after 9 years. Clin Plast Surg. 1988;15(4):627-639.
2 Marchac D, de Olarte G. Reduction mammaplasty and correction of ptosis with a short inframammary scar. Plast Reconstr Surg. 1982;69(1):45-55.
3 Marchac D. Reduction mammaplasty with short inframammary scar. Plast Reconstr Surg. 1986;77(5):859-860.
4 Lassus C. A 30-year experience with vertical mammaplasty. Plast Reconstr Surg. 1996;97(2):373-380.
5 Lassus C. Breast reduction: evolution of a technique – a single vertical scar. Aesth Plast Surg. 1987;11(2):107-112.
6 Lassus C. Reduction mammaplasty with short inframammary scars. Plast Reconstr Surg. 1986;77(4):680-681.
7 Lejour M, Abboud M, Declety A, et al. Reduction des cicatrices de plastie mammaire: de l’ancre courte a la verticale. Ann Chir Plast Esth. 1990;35(5):369-379.
8 Lejour M. Vertical mammaplasty and liposuction of the breast. Plast Reconstr Surg. 1994;94(1):100-114.
9 Hall-Findlay EJ. Pedicles in vertical breast reduction and mastopexy. Clin Plast Surg. 2002;29(3):379-391.
10 Hall-Findlay EJ. A simplified vertical reduction mammaplasty: shortening the learning curve. Plast Reconstr Surg. 1999;104(3):748-759.
11 Lista F, Ahmad J. Vertical scar reduction mammaplasty: a 15-year experience including a review of 250 consecutive cases. Plast Reconstr Surg. 2006;117(7):2152-2165.
12 Schumacher HH. Breast reduction and smoking. Ann Plast Surg. 2005;54(2):117-119.
13 Gradinger GP. Reduction mammoplasty utilizing nipple-areola transplantation. Clin Plast Surg. 1988;15(4):641-654.
14 Gamboa-Bobadilla GM, Killingsworth C. Large-volume reduction mammaplasty: the effect of body mass index on postoperative complications. Ann Plast Surg. 2007;58(3):246-249.
15 Kerrigan CL. PSMA’S for Women Seeking Consultation for Breast Reduction Surgery – The BRITE Visit. In: Noffsinger EB, editor. Running Group Visits in Your Practice. Berlin: Springer, 2008.
16 Kuiken S, Seiffert D. Thinking outside the box! Enhance patient education by using shared medical appointments. Plast Surg Nurs. 2005;25(4):191-195.
17 Descamps MJ, Landau AG, Lazarus D, et al. A formula determining resection weights for reduction mammaplasty. Plast Reconstr Surg. 2008;121(2):397-400.
18 Sigurdson LJ, Kirkland SA. Breast volume determination in breast hypertrophy: an accurate method using two anthropomorphic measurements [see comment]. Plast Reconstr Surg. 2006;118(2):313-320.
19 Fahmy FS, Hemington-Gorse SJ. The sitting, oblique, and supine marking technique for reduction mammaplasty and mastopexy [see comment]. Plast Reconstr Surg. 2006;117(7):2145-2151.
20 Mottura AA. Circumvertical reduction mammaplasty. Clin Plast Surg. 2002;29(3):393-399.
21 Hammond DC. The SPAIR mammaplasty. Clin Plast Surg. 2002;29(3):411-421.
22 Hammond DC. Short scar periareolar inferior pedicle reduction (SPAIR) mammaplasty. Plast Reconstr Surg. 1999;103(3):890-901.
23 Spector JA, Kleinerman R, Culliford AT, et al. The vertical reduction mammaplasty: a prospective analysis of patient outcomes. Plast Reconstr Surg. 2006;117(2):374-381.
24 Collins ED, Kerrigan CL, Kim M, et al. The effectiveness of surgical and nonsurgical interventions in relieving the symptoms of macromastia. Plast Reconstr Surg. 2002;109(5):1556-1566.