CHAPTER 21 Superolateral Pedicle Breast Reduction with Vertical and Inverted T Patterns
Key Points
Patient Selection
The superolateral dermoparenchymal pedicle has been adapted for surgery on a myriad of breast types using differing skin excisions. A simple classification system that reflects the versatility of the superolateral pedicle operation has been developed and is used to select appropriate patients for this technique.1
Type I: Superolateral dermoparenchymal pedicle using the modified Wise pattern:2
Type II: Superolateral dermoparenchymal pedicle using the vertical pattern:
Indications
The evolution of procedures designed to reduce breast volume and improve breast shape has been an ongoing process since the first reports by the Greek physician, Paulus Aegineta, probably during the seventh century ce (sixth book of the Synopsis of Medicine in Seven Books). Since that time, almost every conceivable pedicle type, both dermal and parenchymal, has been successfully employed. This flexibility in pedicle selection is afforded by the rich blood supply network to the breast, which includes the internal mammary artery, lateral thoracic artery, multiple intercostal perforators, thoracoacromial artery, and thoracodorsal artery. As Aufricht stated: ‘There is sufficient blood supply from any direction of the breast hemisphere to nourish the corresponding tissue.3
The anatomic innervation to the breast has been described by several authors. A detailed description of the anatomy was provided by Sir Astley Cooper in 1840.4 Craig and Sykes5 have elucidated the importance of the third, fourth, and fifth anterior cutaneous nerves, and the fourth and fifth lateral cutaneous nerves, in supplying sensation to the nipple–areola complex. Courtiss and Goldwyn6 identified the lateral cutaneous branch of the fourth intercostal nerve as the major source of innervation to the nipple–areola complex. Attempts at preserving maximal nipple–areola sensation during breast surgery must take these anatomic features into account.
The superolateral dermoparenchymal pedicle technique integrates elements from several other operations. Strombeck7 developed a horizontal bipedicled dermoparenchymal flap for breast reduction in 1960. Skoog8 is credited with describing the first lateral pedicle, modifying the Strombeck procedure by elevating the nipple–areola complex on a lateral dermal pedicle alone. In 1982, Nicolle9 presented his experience with the lateral dermoparenchymal pedicle for breast reduction. Cardenas-Camerana and Vergara10 described their successful use of the superolateral dermoglandular pedicle.
The superolateral dermoparenchymal pedicle has been successfully employed by the authors in over 1500 breast operations, including reduction mammaplasty and mastopexy procedures, using differing patterns of skin excisions. For many years the procedure was performed using a modified Wise pattern only, for skin excision. During the past 7 years, following the presentations of Lassus,11 Lejour and Abboud,12 and especially Hall-Findlay,13 a vertical pattern of skin and breast excision has been offered to patients. Follow-up for some patients has been for 15 years (Figs 21.13 and 21.14). Routinely, patients are followed for a minimum of 5 years.
Operative Techniques
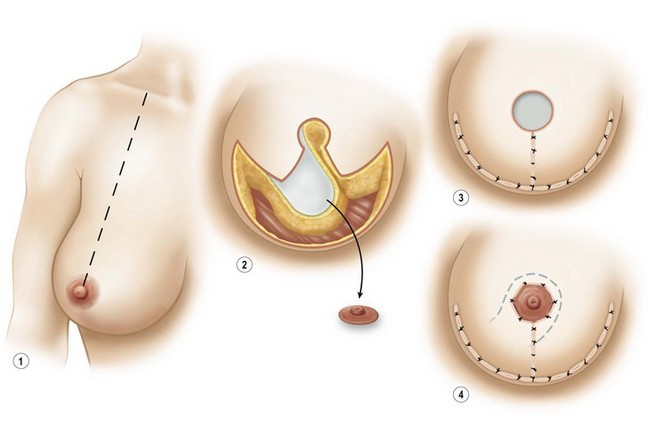
Wise pattern procedure (types Ia (Fig. 21.1), Ib (Fig. 21.2), Ic (Fig. 21.3))
Markings
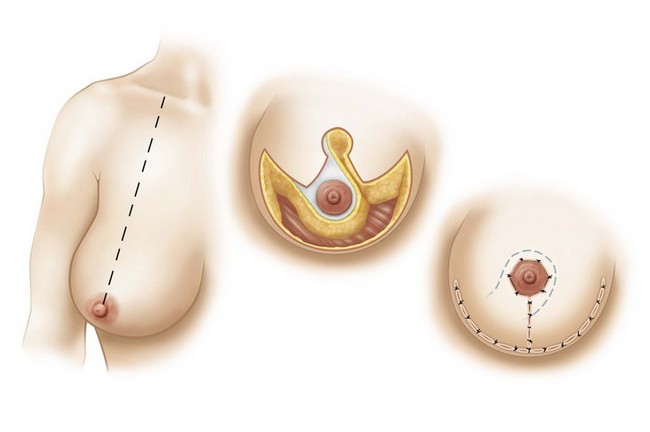
Fig. 21.1 Wise-type pattern variation (Ia).
With permission from Strauch B, Elkowitz M, Baum T, Herman C. Superolateral pedicle for breast surgery: an operation for all reasons. Plast Reconstr Surg 2005;115(5):1269–77; discussion 1278–9.
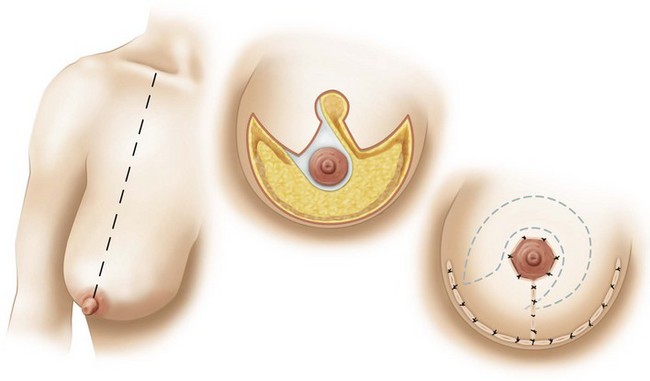
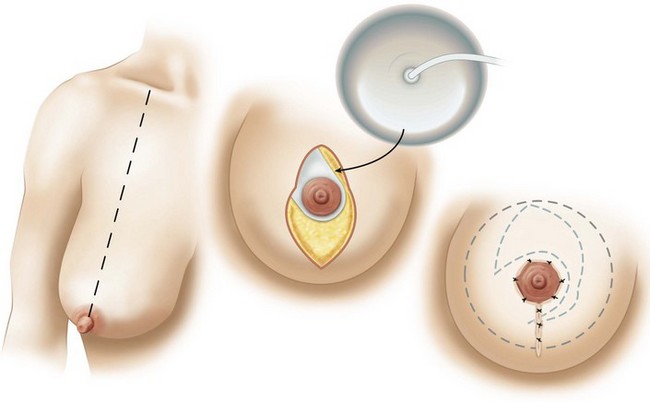
Fig. 21.2 Wise-type variation (Ib).
Wise-type pattern resection with SLDP for mastopexy for correction of ptosis.
With permission from Strauch B, Elkowitz M, Baum T, Herman C. Superolateral pedicle for breast surgery: an operation for all reasons. Plast Reconstr Surg 2005;115(5):1269–77; discussion 1278–9.
Vertical pattern procedure (types IIa (Fig. 21.4), IIb.i (Fig. 21.5), IIb.ii (Fig. 21.6))
Indications
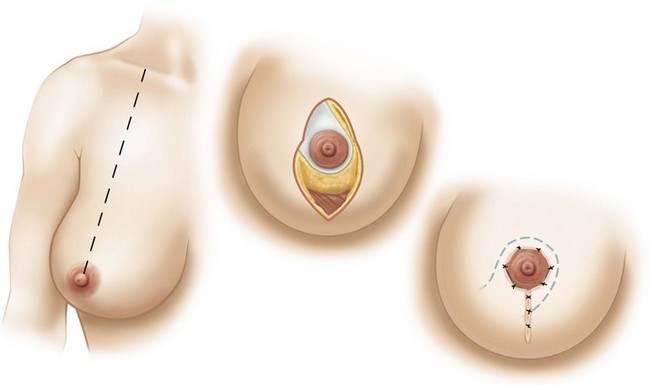
Fig. 21.4 Vertical pattern variation (IIa).
Vertical reduction using an SLDP pedicle for moderate-to-small reductions.
With permission from Strauch B, Elkowitz M, Baum T, Herman C. Superolateral pedicle for breast surgery: an operation for all reasons. Plast Reconstr Surg 2005;115(5):1269–77; discussion 1278–9.
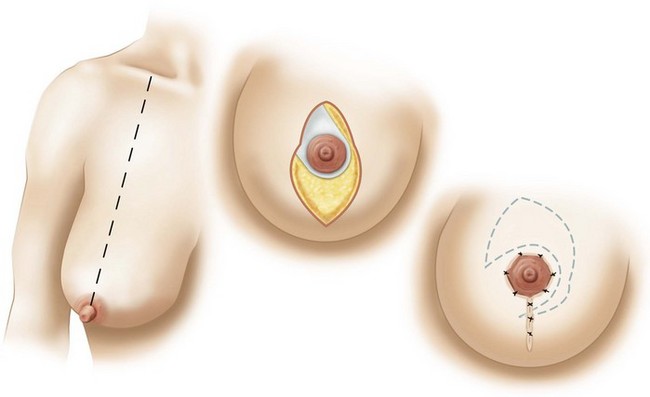
Fig. 21.5 Vertical pattern variation (IIb.i).
With permission from Strauch B, Elkowitz M, Baum T, Herman C. Superolateral pedicle for breast surgery: an operation for all reasons. Plast Reconstr Surg 2005;115(5):1269–77; discussion 1278–9.
Markings
The preoperative markings are drawn with the patient in the standing position, using the same markings as described by Lejour and Abboud.13 Nipple height placement is determined as previously described for the Wise pattern patient and is generally between 21 and 25 cm, depending on the height of the patient. The standard mosque pattern is marked with vertical limbs traced free-hand, based on the surgeon’s assessment of the patient’s skin envelope. The vertical limbs curve to automatically meet at a point 2 to 3 cm superior to the inframammary fold.
Pitfalls and How to Correct
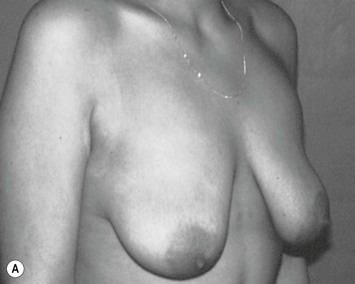
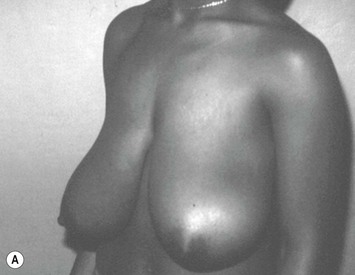
The superolateral pedicle has been used in 1500 breast surgeries. Patients have been followed up to 15 years (see Figs 21.7–21.14 for examples). Total nipple–areola necrosis was observed in four patients. Two had bilateral loss and two had unilateral loss, a total nipple–areola loss of six, or a loss of 0.2% of all nipple–areola complexes. Epidermolysis associated with partial areolar loss was seen in three cases (0.2%). In type I cases, delayed wound healing at the ‘T’ closure was observed in 126 cases (8%), but all healed without the need for operative intervention. Some loss of pigmentation with partial or complete repigmentation was seen in all patients with free nipple grafts. Twelve cases involving free nipple grafts required color tattooing (0.8%). Palpable fat necrosis occurred in 26 patients (1.7%); one patient with fat necrosis underwent excision of the area of fat necrosis by a general surgeon, because it was misinterpreted by the surgeon as being a suspicious breast mass. Three patients who had undergone type II (vertical pattern) reductions using the superolateral pedicle required reoperation for contour revision (0.4%); the revision involved adding a transverse incision at the inframammary fold. Clinically detectable postoperative infections occurred in two patients (0.1%), but did not require surgical intervention. Scar revision was required in seven patients with type I procedures (0.9%), all resulting from unfavorable scars in the lateral or medial segments of the transverse incision line. Nipple–areola sensibility was evaluated as normal or slightly reduced at 1-year follow-up in 1440 patients (96%), with only 60 patients (4%) reporting significantly decreased or absent sensibility. There were no clinically detectable cases of hematoma or seroma. No operative or perioperative mortalities have been experienced.


Fig. 21.14 A Same patient as in Figure 21.13, now 10 years postoperative. Shows continued excellent contour of the reduced breast in frontal view. B Same patient showing oblique view 10 years postoperatively.
With permission from Strauch B, Elkowitz M, Baum T, Herman C. Superolateral pedicle for breast surgery: an operation for all reasons. Plast Reconstr Surg 2005;115(5):1269–77; discussion 1278–9.
The incidence of complications using the superolateral dermoparenchymal pedicle compares favorably with those documented in studies using the inferior pedicle technique.14,15 A total of six complete nipple–areola necroses occurred in four patients out of the entire series of 1500 (0.2%). Satisfactory nipple sensation was maintained in 96% of cases, which may be attributable to preservation of the lateral cutaneous fourth intercostal nerve supply to the nipple–areolar complex. There was a very low incidence of contour deformities requiring further operation (0.4%).
1 Strauch B, Elkowitz M, Baum T, Herman C. Superolateral pedicle for breast surgery: An operation for all reasons. Plast Reconstr Surg. 2005;115(5):1269-1277.
2 Wise RJ. A preliminary report on a method of planning the mammaplasty. Plast Reconstr Surg. 1956;17:367.
3 Aufricht G. Mammaplasty for pendulous breasts. Empiric and geometric planning. Plast Reconstr Surg. 1949;4:13.
4 Cooper A. The anatomy of the breast. London: Longman; 1840.
5 Craig RDP, Sykes PA. Nipple sensitivity following reduction mammaplasty. Br J Plast Surg. 1970;23:165.
6 Courtiss EH, Goldwyn RM. Breast sensation before and after plastic surgery. Plast Reconstr Surg. 1976;58:1.
7 Strombeck JO. Mammaplasty: report of a new technique based on the two pedicle procedure. Br J Plast Surg. 1960;13:79.
8 Skoog T. A technique of breast reduction. Transposition of the nipple of a cutaneous vascular pedicle. Acta Chir Scand. 1963;126:453.
9 Nicolle F. Improved standards in reduction mammaplasty and mastopexy. Plast Reconstr Surg. 1982;69:453.
10 Cardenas-Camarena L, Vergara R. Reduction mammaplasty with superior-lateral dermoglandular pedicle: another alternative. Plast Reconstr Surg. 2001;107:693.
11 Lassus C. A technique for breast reduction. Int Surg. 1970;52:69.
12 Lejour M, Abboud M. Vertical mammaplasty without inframammary scar and with breast liposuction. Perspect Plast Surg. 1990;4:67.
13 Hall-Findlay EJ. A simplified vertical reduction mammaplasty: shortening the learning curve. Plast Reconstr Surg. 1999;104:748.
14 Maxwell Davis G, Ringler SL, Short K, et al. Reduction mammaplasty: long-term efficacy, morbidity, and patient satisfaction. Plast Reconstr Surg. 1995;96:1106.
15 Brown DM, Young VL. Reduction mammaplasty for macromastia. Aesthetic Plast Surg. 1993;17:211.