231 Superior vena caval obstruction
Salient features
History
Examination
• Tortuous, visible and dilated veins on the chest wall and neck (Fig. 231.1).
• The neck veins are non-pulsatile
• The face may be plethoric and suffused. The patient may be short of breath
• Look for signs of Horner syndrome and for radiation marks
• Tell the examiner that you would like to examine for signs of bronchogenic carcinoma, i.e. clubbing, tar staining, lymph nodes and chest signs.
Questions
How would you manage this patient?
• intravenous furosemide to relieve the oedematous component of vena caval compression
• intravenous anticancer chemotherapy, e.g. cyclophosphamide
• mediastinal irradiation within 24 h (the majority of the tumour types causing the superior vena cava syndrome are sensitive to radiotherapy, but tissue diagnosis is required prior to radiotherapy)
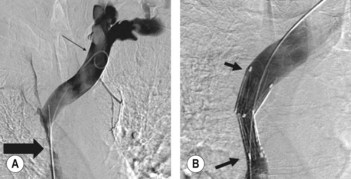
• more recently, expandable metal stents have been used to relieve the obstruction (Fig. 231.2)
• mechanical thrombectomy with an Amplatz thrombectomy device (BMJ 1994;308:1697–9).