CHAPTER 18 Superior Labrum Anterior and Posterior (SLAP) Tears
Pathology of the superior glenoid labrum and bicipital tendon insertion can present as chronic shoulder pain and yield subtle findings. In 1985, Andrews initially described this type of pathology in throwing athletes.1 Superior labrum anterior and posterior (SLAP) lesions, originally referred to by Snyder as superior labrum anterior and posterior lesions, were classified by Snyder in 1990.2 This initial classification was later expanded to include a total of 10 SLAP subtypes.3,4 Whereas this classification has enabled surgeons to approach SLAP lesions systematically and study them more thoroughly, difficulty lies in the preoperative diagnosis and differentiating symptomatic superior labral pathology from normal variants. The difficulty is compounded by the natural degenerative changes that occur in the labrum with advancing age.5 In addition, the accepted mechanisms of injury are as different as the different types of SLAP pathology.6 Included in this chapter are the current SLAP tear classifications and a systematic approach to diagnosis and treatment.
ANATOMY AND PATHOANATOMY
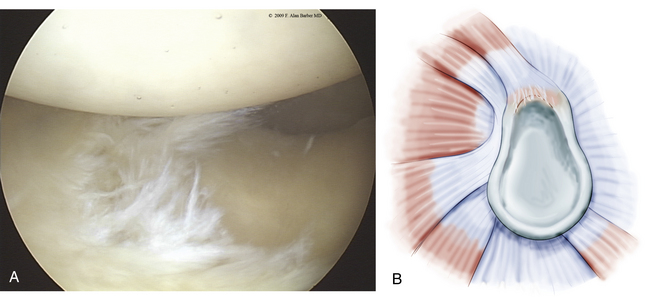
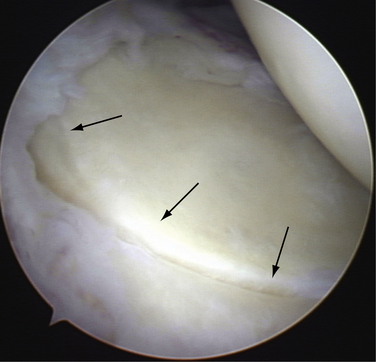
With the increased acceptance and improved techniques of shoulder arthroscopy, clinically significant SLAP lesions have become more distinguishable from normal anatomy. As noted, Snyder’s initial classification of SLAP lesions was expanded to include 10 SLAP subtypes.2–4 Type 1 SLAP lesions have fraying on the inner margin of the superior labrum (Fig. 18-1). These are likely to represent normal degenerative changes and the retreat of blood supply from the superior labrum associated with normal aging.5 Occasionally, a meniscus-like superior labrum (meniscoid labrum, a normal variant) can have similar degenerative fraying of the inner rim and can also be classified as a type 1 lesion; it is the most frequently encountered type.
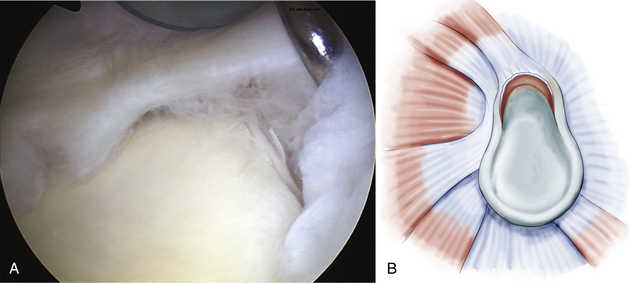
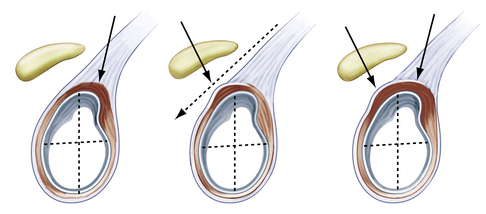
In a type 2 SLAP (Fig. 18-2), which is the most common clinically significant lesion,2,7–9 the superior labrum is pulled off the superior glenoid tubercle at the bicipital attachment. Three subtypes have been described by Morgan and colleagues,10 including anterior, posterior, and combined anterior and posterior (Fig. 18-3). The anterior variant is the most common type 2 SLAP in throwing athletes, but the posterior variant is also commonly seen in the same population. Combined avulsion from both anterosuperior and posterosuperior quadrants of the glenoid is the least common subtype encountered.
The peel-back phenomenon initially described by Burkhart and Morgan11 occurs when the labrum detaches and slides medially or peels off the posterior superior glenoid because of the force transmission of the biceps tendon origin. This pathology may be demonstrated by placing the shoulder into abduction and external rotation while viewing arthroscopically.
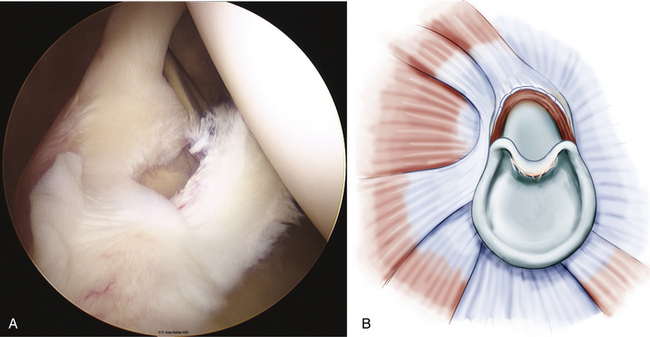
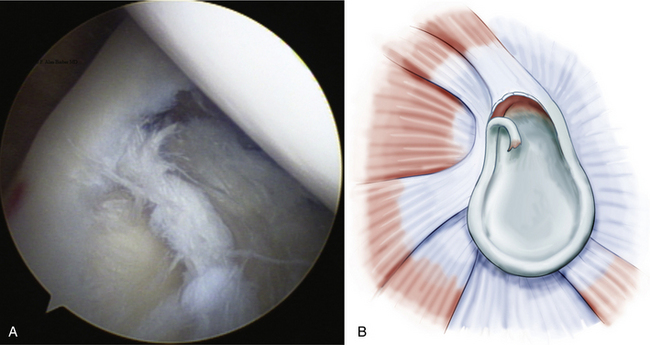
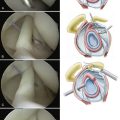
Type 3 SLAP lesions usually extend from anterior to posterior with a bucket handle tear configuration (Fig. 18-4). Type 3 differs from type 2 because there is no elevation of the biceps-labral attachment from the glenoid. The type 4 SLAP is a bucket handle labral tear that extends into the biceps tendon, resulting in a split in the tendon attachment (Fig. 18-5).
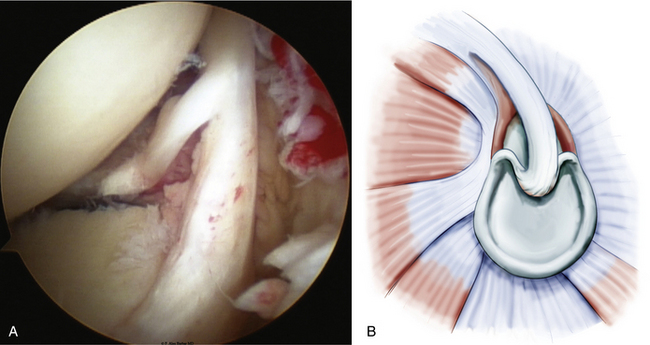
FIGURE 18-5 The type 4 SLAP lesion is a bucket handle labral tear (A) that extends into the biceps tendon, resulting in a split in the tendon attachment (B); left shoulder, posterior portal, lateral decubitus position.
(B from Powell SE, Nord KD, Ryu RK. The diagnosis, classification and treatment of SLAP lesions. Oper Tech Sports Med. 2004;12:99-110.)
Classifications of labral pathology that include shoulder instability were later added.3 Type 5 SLAP lesions are Bankart lesions that extend superiorly to the biceps attachment (Fig. 18-6). Type 6 SLAP lesions have an anterior or posterior labral flap and a type 2 separation from the superior glenoid (Fig. 18-7). Type 7 SLAP lesions include a separation of the biceps attachment that extends into the middle glenohumeral ligament (Fig. 18-8). A type 8 SLAP4 is a posterior labral extension of a type 2 SLAP lesion (Fig. 18-9). Type 9 SLAP lesions show complete circumferential labral tearing (Fig. 18-10). A type 10 SLAP lesion includes a type 2 SLAP with a posterior inferior labral separation.
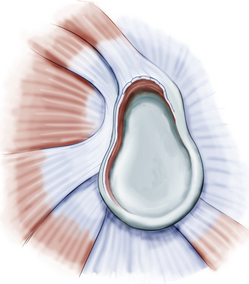
FIGURE 18-6 A type 5 SLAP is a Bankart lesion that extends to the biceps attachment.
(From Powell SE, Nord KD, Ryu RK. The diagnosis, classification and treatment of SLAP lesions. Oper Tech Sports Med. 2004;12:99-110.)
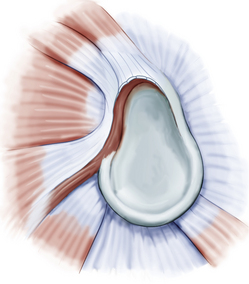
FIGURE 18-8 Type 7 SLAP lesions include a separation of the biceps attachment that extends into the middle glenohumeral ligament.
(From Powell SE, Nord KD, Ryu RK. The diagnosis, classification and treatment of SLAP lesions. Oper Tech Sports Med. 2004;12:99-110.)
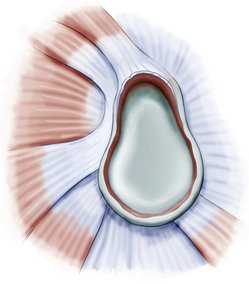
FIGURE 18-10 A type 9 SLAP lesion is a type 2 SLAP with circumferential labral tearing.
(From Powell SE, Nord KD, Ryu RK. The diagnosis, classification and treatment of SLAP lesions. Oper Tech Sports Med. 2004;12:99-110.)
Despite the extensive classification of SLAP tears, the overall incidence of superior labral pathology is low unless associated with shoulder instability. Type 2 tears are the most frequently observed clinically significant labral lesions. Excluding a type 1 tear, type 2 lesions represent 50% or more of SLAP tears, but only 4% to 6% of all intra-articular pathology detected at the time of arthroscopy.2,7 The most frequently associated pathology in patients younger than 40 years with clinically significant type 2 lesions is shoulder instability. When the patient is older than 40 years and a type 2 SLAP lesion is present, rotator cuff pathology or glenohumeral arthritis is most frequently found.9 There is no advantage to repairing a SLAP lesion in patients older than 50 years.12
CLINICAL PRESENTATION
History
The history and physical examination are very important in the identification of clinically significant SLAP lesions, which are commonly found in throwing athletes or after a specific traumatic event.2,3,7 Many patients complain about anterior shoulder pain, clicking and popping in the shoulder, and decreased function. A long history of overhead throwing activity may result in significant humeral retroversion. Athletes often will present with overhead activity pain, decreased power or velocity of their throws (sometimes termed dead arm syndrome),13,14 or slower lap time in swimmers. Each of these may manifest acutely or over time.
The primary challenge for the clinician is to distinguish symptomatic superior labral pathology from asymptomatic lesions and normal anatomic variations.8 The physical examination and mechanism of injury should correlate with a SLAP tear. The addition of imaging studies can be helpful, but should be reviewed with discernment because they can give false-positive results.15,16
Most SLAP lesions are found in the dominant arm of male patients who have been involved with overhead or throwing activities at a high level, and are younger than 40 years. The traumatic subgroup may have isolated shoulder trauma or variations of instability. The initial history should reveal patients who have a history of a shoulder dislocation, a fall on outstretched hand, or a motor vehicle accident during which the patient was wearing a shoulder lap belt over the involved shoulder.17
Patient age is an important consideration when diagnosing shoulder pain, and it is important to understand which patients are likely to develop a true SLAP injury. Patients older than 40 years often have naturally occurring degenerative changes that can mimic a SLAP lesion.9,12 Pfahler and associates5 have described the normal aging pattern of the superior labrum. Microscopic and macroscopic evaluation of normal shoulders demonstrated age-dependent variations. Three age- dependent stages were described: (1) a child up to 10 years old has a normal circumferential labral attachment without damage; (2) adults between 30 and 50 years old demonstrate fissuring and sublabral recesses at the superior and anterosuperior area of the glenoid labrum; and (3) those older than 60 years demonstrate an inconsistently attached superior labrum with tearing, fissuring, and labral detachment.5
Physical Examination
Various physical examination maneuvers have been described to aid in diagnosis of symptomatic SLAP lesions. The common element of these maneuvers is the application of either torsional or tensile loads on the biceps anchor.
A positive Speed test18 produces pain at the anterior bicipital groove by resisted forward flexion with the shoulder flexed at 90 degrees and the forearm fully supinated. A positive test suggests biceps tendinitis.
The modified O’Brien test19 is performed with the patient’s arm in 10 to15 degrees of adduction and 90 degrees of forward flexion (Fig. 18-11). With the patient’s arm fully pronated and the thumb pointing toward the floor, the patient resists the examiner’s downward pressure on the wrist of the outstretched arm. Next, the arm is fully supinated, with the palm facing up, and the examiner again places downward pressure on the wrist while the patient resists. Anterior shoulder pain with forearm pronation that is relieved with supination is considered a positive test and suggestive of a SLAP lesion. Tenderness at the acromioclavicular (AC) joint combined with local tenderness to palpation is suggestive of AC joint pathology. In both cases, a positive test consists of less pain with the palm up than with the thumb down.
Decreased glenohumeral internal rotation compared with the opposite shoulder is suggestive of a tight posterior capsule (Fig. 18-12). The most accurate way to measure internal rotation is to stabilize the scapula of the supine patient by pressure on the anterior shoulder, and measure internal and external rotation with the arm at 90 degrees abduction. Full shoulder rotation motion is measured with a goniometer and should be equal to 180 degrees. When excessive humeral retroversion is present, as with long-term throwing athletes, the throwing arm may have increased external rotation and decreased internal rotation. If the patient fails to gain full motion after a physical therapy program, the presence of a SLAP lesion should be considered.
Although these and other physical tests, including the crank test,20 anterior slide test,21 biceps load test,22 and Jobe relocation test21 have been reported to indicate the presence of superior labral pathology, they are not always consistently diagnostic.23–27 Nonetheless, they do have a role in the physical examination of the shoulder.28 There is lack of consensus for SLAP diagnosis, even among experienced shoulder surgeons. Recently, intraobserver and interobserver reliability for the diagnosis based on a review of arthroscopic videos was just over 50% among 70 experienced shoulder arthroscopic surgeons.29 Arthroscopy is still considered one of the principal diagnostic tools.
DIAGNOSTIC IMAGING
Initial radiographic imaging should consist of standard shoulder radiographs including anteroposterior (AP), Y outlet, and axillary views to determine if any associated bony pathology is present. If the history and physical examination point to superior labral pathology and a course of nonoperative treatment is unsuccessful in relieving the patient’s symptoms, magnetic resonance imaging (MRI) may be considered. MRI with the addition of gadolinium (Fig. 18-13) enhances the evaluation of the superior labrum, and interpretation by a musculoskeletal radiologist improves their accuracy.15,16 Accuracy of community read plain MRI scans are approximately 51% and slightly improved if a gadolinium arthrogram is obtained. Fellowship-trained musculoskeletal radiologists increase the accuracy by 10% to 20%.
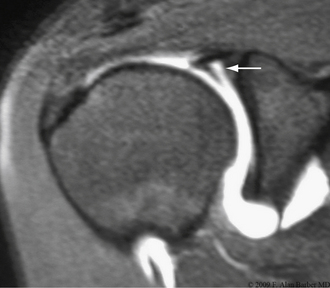
Variations within the anatomy of the superior labrum make the interpretation of imaging studies challenging. A sulcus measuring 1 to 2 mm or more identified on MRI may be a normal sublabral separation from the glenoid surface.30 Despite this normal variation, contrast may fill the sulcus and be falsely interpreted as a type II SLAP tear. The presence of a sublabral cyst is highly suggestive of a SLAP tear (Fig. 18-14) and, when it extends medially, may be contributing to suprascapular nerve compression.31–35
TREATMENT OPTIONS
Surgical Treatment
Surgery is indicated when the patient has failed 3 months of nonoperative treatment and symptoms persist. Surgical treatment of SLAP lesions is arthroscopic and dependent on the type of superior labral pathology encountered.36 Type 1 SLAP lesions are traditionally treated with débridement of the frayed labrum. Type 2 SLAPs necessitate stabilization of the biceps–superior labral anchor. Type 3 and 4 SLAPs require removal of the bucket handle portion of the superior labrum, whereas an additional suture repair or biceps tenodesis may be added for the type 4 variety. The type 4 SLAP can be further subdivided into the type 4A lesion, with a white on red bucket handle portion best treated with excision of the bucket and repair of the remaining biceps anchor to the bone and type 4B, which splits vertically into the biceps in a red on red pattern. These may be repaired with side to side suturing.37 Repair of type 4 lesions results in a successful outcome provided that no more than 30% of the biceps root is compromised. When the biceps anchor compromise is greater, a biceps tenodesis should be considered.
Types 5 through 7 lesions are likely to be associated with a previous glenohumeral instability.3 The instability should be repaired with the associated biceps-labral anchor. Type 6 lesions require flap débridement in addition to fixing the type II component. The labrum in subtypes 8, 9, and 10 requires repair with suture anchors and, when present, a flap débridement performed.4 Eliminating the peel-back sign and any drive-through laxity indicates that the labral injury has been adequately stabilized.
After the standard posterior viewing portal is established, an anterior instrumentation and viewing portal can be located midway between the anterior acromial margin and coracoid. Proper placement is confirmed using a needle.37a A lateral anterior superior portal has been described in the rotator cuff interval about 3 cm more laterally than the normal anterior superior portal.38 A single anterior instrumentation portal is sometimes sufficient if all that is required is a single anchor at the biceps attachment. After the initial anterior cannula is established, the superior labrum can be carefully evaluated and probed.
A second instrumentation portal may be helpful to assist with anchor insertion and suture management, especially when a posterior or combined type 2 SLAP lesion is encountered. A portal placed 1 cm lateral and 1 to 2 cm anterior to the posterior lateral corner of the acromion (Port of Wilmington portal) can provide proper anchor orientation to the posterosuperior glenoid. Posterior and lateral portals will pierce the rotator cuff. Recently, concerns have been raised about the clinical significance of the rotator cuff damage and the possibility for later sequela associated with trans–rotator cuff portals.39 The consequences of a trans–rotator cuff portal are likely to be related to its size and location. Small holes may be innocuous and asymptomatic, whereas larger portals may warrant primary suture closure. However, some believe that concerns about the trans–rotator cuff portal are not justified.40–42 The key to successful SLAP repair is the recreation of a stable biceps-labral complex while eliminating the peel-back and drive-through signs. To accomplish this, the portals should be placed to allow proper access for labral preparation and anchor insertion.
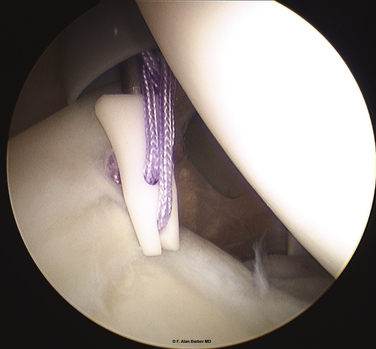
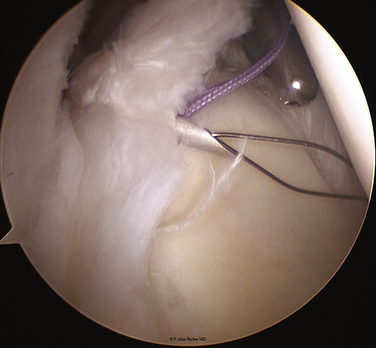
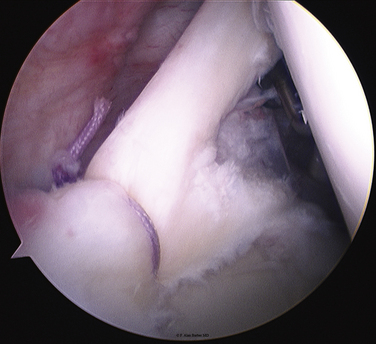
Labral anchors come with one or two sutures. Various suture configurations have been described and used. Recent studies have increased our understanding about secure biceps-labral anchor fixation and optimal suture anchor placement. Morgan and coworkers43 have demonstrated no biomechanical advantage in placement of one suture anchor anterior to the biceps attachment and one anchor posterior to the biceps attachment versus two anchors posterior to the biceps. This anterior suture anchor could, theoretically, tension the anterior capsulolabral structures via the superior and middle glenohumeral ligaments to the superior labrum and result in increased postoperative stiffness.43 Yoo and colleagues44 have evaluated three different posterior labral fixation methods: one anchor with a conventional simple stitch, one anchor through the posterior-superior labrum using a mattress stitch, and two anchors with single simple stitches. One simple stitch in one anchor was found to be sufficient to withstand the initial load without clinical failure for posterior SLAP lesions and the mattress suture was found to be inferior to a simple suture technique. These studies suggest that placing a single anchor with a simple stitch posterior to the biceps root should be sufficient for most posterior SLAPs and may be sufficient for all type 2 SLAP repairs (Fig. 18-15).
A tissue-penetrating instrument through a separate portal may also be used. This device is passed through the labrum to capture the suture (a hand-off technique using a ring grasper helps here) and then retrieves that suture as the device is withdrawn. The Neviaser portal works well for this technique.45 The Neviaser portal was described by Neviaser in 198746 as the superior medial portal bordered by the clavicle, the acromioclavicular joint, and the spine of the scapula. Another option is to place a spinal or intracath needle through the Neviaser or other suitable location. The needle should be advanced through the cuff and capsule in a way that allows it to be clearly visible from the posterior viewing portal. The needle then slides under the labrum at the appropriate location. A twisted Nitinol wire device with an expandable distal basket (Chia Percpasser, DePuy Mitek, Raynham, Mass) is passed through this needle and retrieved from the anterior instrumentation cannula (Fig. 18-16). One arm of the suture in the anchor is threaded through the basket and the wire retrieved. The needle must be backed off the wire prior to retrieving it to avoid cutting the wire or the suture.
After the anchor is placed and the suture is passed through the tissue, the knot is tied arthroscopically. There are several appropriate ways to accomplish this with nonsliding and sliding knots. The recent adoption of ultra–high-molecular-weight polyethylene containing sutures has made knot tying easier. Suture breaking and fraying during knot tying with a single- lumen knot pusher is much less of a problem. However, polyethylene sutures have been shown to be much more likely to slip than braided polyester sutures, and knot selection is important. The Duncan loop and Weston knot have been shown to slip prior to ultimate failure in over 90% of tested knots47 and an alternative knot is preferred. The tied knot should use the limb that passes through the labrum as the post, keeping the knot as far from the surface as possible. It is advisable to keep the knot on the soft tissue side away from the articular surface (Fig. 18-17). As noted, a single anchor with a single simple stitch placed posterior to the biceps root is our preferred technique for most posterior type 2 SLAP tears. If the peel-back sign is dramatic and the posterior labral separation extends to the 9 o’clock position, a second anchor with a single simple stitch may be added.43,44
Intraoperative and postoperative pain control facilitates the procedure and the recovery process. Three nerves innervate the shoulder—the axillary, suprascapular (SSN), and lateral pectoral (LPN) nerve. Pain can be reduced by a percutaneous block of the SSN and LPN prior to surgery. Both blocks are administered using 0.25% bupivacaine without epinephrine. The SSN block is placed through an 18-gauge spinal needle positioned about 8 cm medial to the lateral border of the acromion, near the Neviaser portal.48,49 The needle is advanced toward the coracoid until it contacts the scapula and then walked anteriorly until if falls off the supraspinatus fossa. The needle is then moved back posteriorly until it touches bone again, an aspiration is performed, and 20 mL of bupivacaine solution are injected. The LPN block50 is performed by the infiltration of 10 mL of anesthetic solution anterior to the clavicle at the level of the deltopectoral groove, aiming for the medial border of the coracoid process.
PEARLS& PITFALLS
SUMMARY
A preoperative diagnosis of a superior labral tear can be confirmed arthroscopically by the presence of sublabral chondromalacia, associated biceps tendon injury, a sublabral sulcus more than 5 mm deep, and superior glenohumeral ligament laxity or tearing. Most type 2 SLAP repairs can be accomplished by placing a single simple stitch posterior to the biceps anchor. The most common postoperative challenge after SLAP repair is the prevention of stiffness. Postoperative immobilization should be avoided.
1. Andrews JR, Carson WGJr, McLeod WD. Glenoid labrum tears related to the long head of the biceps. Am J Sports Med. 1985;13:337-341.
2. Snyder SJ, Karzel RP, Del Pizzo W, et al. SLAP lesions of the shoulder. Arthroscopy. 1990;6:274-279.
3. Maffet MW, Gartsman GM, Moseley B. Superior labrum-biceps tendon complex lesions of the shoulder. Am J Sports Med. 1995;23:93-98.
4. Powell SE, Nord KD, Ryu RK. The diagnosis, classification and treatment of SLAP lesions. Oper Tech Sports Med. 2004;12:99-110.
5. Pfahler M, Haraida S, Schulz C, et al. Age-related changes of the glenoid labrum in normal shoulders. J Shoulder Elbow Surg. 2003;12:40-52.
6. Clavert P, Bonnomet F, Kempf JF, et al Contribution to the study of the pathogenesis of type II superior labrum anterior-posterior lesions: a cadaveric model of a fall on the outstretched hand. J Shoulder Elbow Surg, 13; 2004:45-50.
7. Snyder SJ, Banas MP, Karzel RP. An analysis of 140 injuries to the superior glenoid labrum. J Shoulder Elbow Surg. 1995;4:243-248.
8. Handelberg F, Willems S, Shahabpour M, et al SLAP lesions: a retrospective multicenter study. Arthroscopy, 14; 1998:856-862.
9. Kim TK, Queale WS, Cosgarea AJ, McFarland EG Clinical features of the different types of SLAP lesions: an analysis of one hundred and thirty-nine cases. J Bone Joint Surg Am, 85; 2003:66-71.
10. Morgan CD, Burkhart SS, Palmeri M, Gillespie M Type II SLAP lesions: three subtypes and their relationships to superior instability and rotator cuff tears. Arthroscopy, 14; 1998:553-565.
11. Burkhart SS, Morgan CD The peel-back mechanism: its role in producing and extending posterior type II SLAP lesions and its effect on SLAP repair rehabilitation. Arthroscopy, 14; 1998:637-640.
12. Franceschi F, Longo UG, Ruzzini L, et al No advantages in repairing a type II superior labrum anterior and posterior (SLAP) lesion when associated with rotator cuff repair in patients over age 50: a randomized controlled trial. Am J Sports Med, 36; 2008:247-253.
13. Burkhart SS, Morgan CD, Kibler WB The disabled throwing shoulder: spectrum of pathology. Part IIevaluation and treatment of SLAP lesions in throwers. Arthroscopy, 19; 2003:531-539.
14. Burkhart SS, Morgan CD, Kibler WB. Shoulder injuries in overhead athletes. The “dead arm” revisited. Clin Sports Med. 2000;19:125-158.
15. Reuss BL, Schwartzberg R, Zlatkin MB, et al Magnetic resonance imaging accuracy for the diagnosis of superior labrum anterior-posterior lesions in the community setting: eighty-three arthroscopically confirmed cases. J Shoulder Elbow Surg, 15; 2006:580-585.
16. Jee WH, McCauley TR, Katz LD, et al Superior labral anterior posterior (SLAP) lesions of the glenoid labrum: reliability and accuracy of MR arthrography for diagnosis. Radiology, 218; 2001:127-132.
17. Ruotolo C, Nottage WM, Flatow EL, et al. Controversial topics in shoulder. Arthroscopy. 2002;18:65-75.
18. Holtby R, Razmjou H Accuracy of the Speed’s and Yergason’s tests in detecting biceps pathology and SLAP lesions: comparison with arthroscopic findings. Arthroscopy, 20; 2004:231-236.
19. O’Brien SJ, Pagnani MJ, Fealy S, et al The active compression test: a new and effective test for diagnosing labral tears and acromioclavicular joint abnormality. Am J Sports Med, 26; 1998:610-613.
20. Liu SH, Henry MH, Nuccion SL. A prospective evaluation of a new physical examination in predicting glenoid labral tears. Am J Sports Med. 1996;24:721-725.
21. Kibler WB. Specificity and sensitivity of the anterior slide test in throwing athletes with superior glenoid labral tears. Arthroscopy. 1995;11:296-300.
22. Kim SH, Ha KI, Ahn JH, Choi HJ Biceps load test II: A clinical test for SLAP lesions of the shoulder. Arthroscopy, 17; 2001:160-164.
23. McFarland EG, Kim TK, Savino RM. Clinical assessment of three common tests for superior labral anterior-posterior lesions. Am J Sports Med. 2002;30:810-815.
24. Stetson WB, Templin K. The crank test, the O’Brien test, and routine magnetic resonance imaging scans in the diagnosis of labral tears. Am J Sports Med. 2002;30:806-809.
25. Mileski RA, Snyder SJ Superior labral lesions in the shoulder: pathoanatomy and surgical management. J Am Acad Orthop Surg, 6; 1998:121-131.
26. Walton DM, Sadi J Identifying SLAP lesions: a meta-analysis of clinical tests and exercise in clinical reasoning. Phys Ther Sport, 9; 2008:167-176.
27. Shanley KJ, Green RA, Taylor NF. An evaluation of the anatomical basis of the biceps load tests I and II for superior labral anterior and posterior (SLAP) lesions. Clin Anat. 2008;21:647-651.
28. Guanche CA, Jones DC. Clinical testing for tears of the glenoid labrum. Arthroscopy. 2003;19:517-523.
29. Gobezie R, Zurakowski D, Lavery K, et al. Analysis of interobserver and intraobserver variability in the diagnosis and treatment of SLAP tears using the Snyder classification. Am J Sports Med. 2008;36:1373-1379.
30. Rao AG, Kim TK, Chronopoulos E, McFarland EG Anatomical variants in the anterosuperior aspect of the glenoid labrum: a statistical analysis of seventy-three cases. J Bone Joint Surg Am, 85; 2003:639-653.
31. Baums MH, Seil R, Kettler M, et al. Treatment option in a SLAP-related ganglion cyst resulting in suprascapular nerve entrapment. Arch Orthop Trauma Surg. 2006;126:621-623.
32. Westerheide KJ, Dopirak RM, Karzel RP, Snyder SJ Suprascapular nerve palsy secondary to spinoglenoid cysts: results of arthroscopic treatment. Arthroscopy, 22; 2006:721-727.
33. Chen AL, Ong BC, Rose DJ. Arthroscopic management of spinoglenoid cysts associated with SLAP lesions and suprascapular neuropathy. Arthroscopy. 2003;19:E15-E21.
34. Westerheide KJ, Karzel RP Ganglion cysts of the shoulder: technique of arthroscopic decompression and fixation of associated type II superior labral anterior to posterior lesions. Orthop Clin North Am, 34; 2003:521-528.
35. Chochole MH, Senker W, Meznik C, Breitenseher MJ Glenoid-labral cyst entrapping the suprascapular nerve: dissolution after arthroscopic debridement of an extended SLAP lesion. Arthroscopy, 13; 1997:735-753.
36. Barber FA, Field LD, Ryu RK Biceps tendon and superior labrum injuries: decision making. Instr Course Lect, 57; 2008:527-538.
37. Weber SC Repair versus tenodesis of type IV SLAP lesions. Poster P418, 11 American Academy of Orthopaedic Surgeons 2009 annual meeting. 2009:25-28
37a. Daluga DJ, Daluga AT. Single-portal SLAP lesion repair. Arthroscopy. 2007;23:321.
38. Buess E, Schneider C. Simplified single-portal V-shaped SLAP repair. Arthroscopy. 2006;22:680.
39. Cohen DB, Coleman S, Drakos MC, et al. Outcomes of isolated type II SLAP lesions treated with arthroscopic fixation using a bioabsorbable tack. Arthroscopy. 2006;22:136-142.
40. Oh JH, Kim SH, Lee HK, et al Trans-rotator cuff portal is safe for arthroscopic superior labral anterior and posterior lesion repair: clinical and radiological analysis of 58 SLAP lesions. Am J Sports Med, 36; 2008:1913-1921.
41. Meyer M, Graveleau N, Hardy P, Landreau P Anatomic risks of shoulder arthroscopy portals: anatomic cadaveric study of 12 portals. Arthroscopy, 23; 2007:529-536.
42. O’Brien SJ, Allen AA, Coleman SH, Drakos MC The trans-rotator cuff approach to SLAP lesions: technical aspects for repair and a clinical follow-up of 31 patients at a minimum of 2 years. Arthroscopy, 18; 2002:372-377.
43. Morgan RJ, Kuremsky MA, Peindl RD, Fleischli JE. A biomechanical comparison of two suture anchor configurations for the repair of type II SLAP lesions subjected to a peel-back mechanism of failure. Arthroscopy. 2008;24:383-388.
44. Yoo JC, Ahn JH, Lee SH, et al. A biomechanical comparison of repair techniques in posterior type II superior labral anterior and posterior (SLAP) lesions. J Shoulder Elbow Surg. 2008;17:144-149.
45. Nord KD, Masterson JP, Mauck BM. Superior labrum anterior posterior (SLAP) repair using the Neviaser portal. Arthroscopy. 2004;20(Suppl 2):129-133.
46. Neviaser TJ. Arthroscopy of the shoulder. Orthop Clin North Am. 1987;18:361-372.
47. Barber FA, Herbert MA, Beavis RC. Cyclic load and failure behavior of arthroscopic knots and high-strength sutures. Arthroscopy. 2009;25:192-199.
48. Checcucci G, Allegra A, Bigazzi P, et al A new technique for regional anesthesia for arthroscopic shoulder surgery based on a suprascapular nerve block and an axillary nerve block: an evaluation of the first results. Arthroscopy, 24; 2008:689-696.
49. Barber FA. Suprascapular nerve block for shoulder arthroscopy. Arthroscopy. 2005;21:1015.
50. Aszmann OC, Dellon AL, Birely BT, McFarland EG Innervation of the human shoulder joint and its implications for surgery. Clin Orthop Relat Res (330); 1996:202-207.