Chapter 31 Superficial fungal infections
Table 31-1. Clinical Presentations of Dermatophyte Infections
| INFECTION | LOCATION |
|---|---|
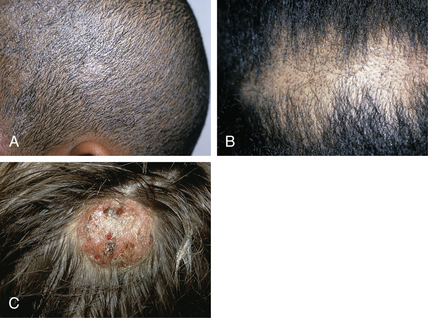
| Tinea capitis | Scalp |
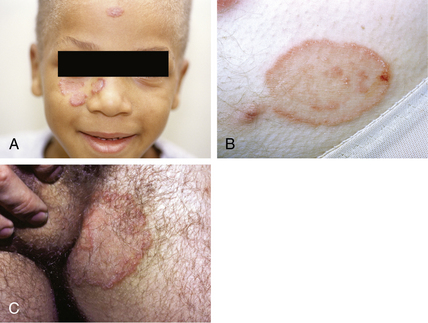
| Tinea faciei (see Fig. 31-1A) | Face |
| Tinea barbae | Beard |
| Tinea corporis (see Fig. 31-1B) | Trunk, extremities |
| Tinea cruris (see Fig. 31-1C) | Groin |
| Tinea manuum (manus) | Hands |
| Tinea pedis | Feet |
| Tinea unguium | Nails |
Foster KW, Ghannoum MA, Elewski BE: Epidemiologic surveillance of cutaneous fungal infections in the United States from 1999 to 2002, J Am Acad Dermatol 50:748–752, 2004.

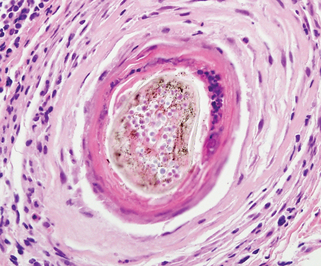
Figure 31-5. Distal subungual onychomycosis demonstrating a spikelike pattern of infection.
(Courtesy of the Fitzsimons Army Medical Center teaching files.)
Erchiga VC, Florencio VD: Malassezia species in skin diseases, Curr Opin Infect Dis 15:133–142, 2002.
Gupta KA, Batra R, Bluhm R, Faergemann J: Pityriasis versicolor, Dermatol Clin 21: 413–429, 2003.
| DISEASE | CLINICAL DESCRIPTION |
|---|---|
| Intertrigo | Superficial pustules, erythema, edema, creamy exudates within skin folds |
| Thrush | White, adherent, cottage cheeselike plaques on oral mucosa |
| Perlèche | Erythema, fissuring, creamy exudate at the angles of the mouth |
| Paronychia | Tender, erythematous, indurated proximal nail fold, with or without a purulent discharge |
| Erosio interdigitalis blastomycetica | Erythema, fissuring, maceration of the webspaces between the fingers |
Table 31-3. Oral Antifungal Agents
| CLASS | EXAMPLES | MECHANISMS OF ACTION |
|---|---|---|
| Antibiotic | Griseofulvin | Arrest of cellular division, dysfunction of spindle microtubules |
| Polyenes | Nyastatin | Binds irreversibly with ergosterol, altering membrane permeability |
| Azoles | Fluconazole Itraconazole Ketoconazole |
Inhibits ergosterol production by inhibiting the cytochrome P-450 lanosterol 14-demethylase |
| Allyamines | Terbinafine | Blocks ergosterol production by inhibiting squalene epoxidase |
Data from Gupta A, Sauder D, Shear N: Antifungal agents: part II, J Am Acad Dermatol 30:911–933, 1993.
Gupta A, Sauder D, Shear N: Antifungal agents: part II, J Am Acad Dermatol 30:911–933, 1993.
Gupta AK, Ryder JE: The use of oral antifungal agents to treat onychomycosis, Dermatol Clin 21:469–479, 2003.
Key Points: Superficial Fungal Infections