CHAPTER 22 Subscapularis Tears
Arthroscopy has revolutionized the way we treat rotator cuff tears1 and many authors have reported excellent clinical results following all arthroscopic rotator cuff repairs. Arthroscopic repair of the subscapularis tendon, however, remains the final frontier for many arthroscopists because of its difficulty with visualization, the awkward angle of approach, and the complex releases required for mobilization and repair.
Subscapularis tears, however, are commonly missed, particularly partial-thickness articular surface tears and full-thickness upper subscapularis tendon tears. The incidence of subscapularis tears has been reported as high as 27% in a study of 165 arthroscopically evaluated shoulders with rotator cuff, labral, or ligamentous disorders.2 Although subscapularis tears do occur in isolation, they are more commonly seen in combination with other rotator cuff tears. In one study, 90% of subscapularis tears were associated with tears of the supraspinatus tendon.3
ANATOMY AND PATHOANATOMY
Recently, cadaveric studies have clarified the insertional anatomy of the subscapularis tendon.4,5 The shape of the tendinous insertion grossly resembles a human ear, with the medial border almost parallel to the longitudinal axis of the humerus, and the insertion broad proximally and tapered distally. The average footprint measures 25.8 ± 3.2 mm in superior to inferior height, and the maximum width measures 18.1 ± 1.6 mm.4 These anatomic dissections highlight the broad insertional anatomy of the footprint and are helpful when determining the percentage of subscapularis tendon torn during arthroscopic evaluation.
Traditionally, the main function of the subscapularis has been described as an internal rotator and anterior stabilizer of the glenohumeral joint. However, the subscapularis tendon is also an important dynamic stabilizer during normal glenohumeral motion. In the normal shoulder, the transverse plane force couple consists of the subscapularis anteriorly, which is balanced against the infraspinatus and teres minor posteriorly, resulting in a balanced force couple in the transverse plane. In contrast, a disruption of the subscapularis leads to loss of the transverse plane force couple and an unstable fulcrum. When rotator cuff repair restores the anterior (subscapularis) and posterior (infraspinatus, teres minor) forces so that the moments between the two are balanced, function will be restored, even in the presence of a persistent defect in the superior rotator cuff (supraspinatus).1
The precise cause of subscapularis tears has yet to be fully defined, but is likely multifactorial and includes intrinsic degeneration, microtrauma or macrotrauma, impaired vascularity, and subcoracoid impingement. Subcoracoid stenosis (narrowing of the subcoracoid space) and subcoracoid impingement (direct contact of the coracoid against the subscapularis tendon or lesser tuberosity) have been implicated in the pathogenesis of subscapularis tears.6 The coracohumeral distance, as measured by axial computed tomography (CT) and magnetic resonance imaging (MRI), has been reported to be 8.7 to 11.0 mm in normal shoulders.7,8 In one study, the average coracohumeral distance was measured by a single axial cut on a preoperative MRI scan. In 35 patients requiring subscapularis repair, the coracohumeral distance was 5.0 ± 1.7 mm; compared with a control group (N = 35) that had no rotator cuff, subscapularis, or subcoracoid pathology, the coracohumeral distance was 10.0 ± 1.3 mm.9 Whereas these and other studies have confirmed a relationship between a narrowed coracohumeral distance and subscapularis tears, the exact temporal or causal relationship between tearing and a decreased coracohumeral distance and subcoracoid impingement is still unclear.10 Cadaveric studies of subscapularis tendons have suggested that intrinsic tendon degeneration may be an important causative factor in tears of the subscapularis.11,12 These studies have demonstrated that the incidence of histologic changes in the subscapularis tendon is similar to that of the supraspinatus tendon; these are most commonly seen in the superior and deep portion of the tendon insertion. Clinically, this corresponds to the area most commonly affected by partial-thickness tears of the subscapularis.
Full-thickness tears of the subscapularis tendon are much less common than partial-thickness tears of the subscapularis tendon or full-thickness tears of the supraspinatus tendon. One key pathoanatomic finding of subscapularis tendon tears has been called the comma sign, which is a comma-shaped arc of soft tissue located superior to the superolateral border of the torn subscapularis tendon.13 This tissue is composed of the fibers of the medial portion of the coracohumeral ligament, as well as a portion of the superior glenohumeral ligament (the medial biceps sling), which interdigitate with the superior fibers of the subscapularis tendon at its humeral insertion. When the subscapularis tendon is torn, the medial biceps sling tears along with it and stays attached to the superolateral corner of the subscapularis tendon, forming a continuous arc of soft tissue. By identifying the comma sign, this tissue can then be followed inferiorly and medially to the superolateral border of the subscapularis tendon.
HISTORY AND PHYSICAL EXAMINATION
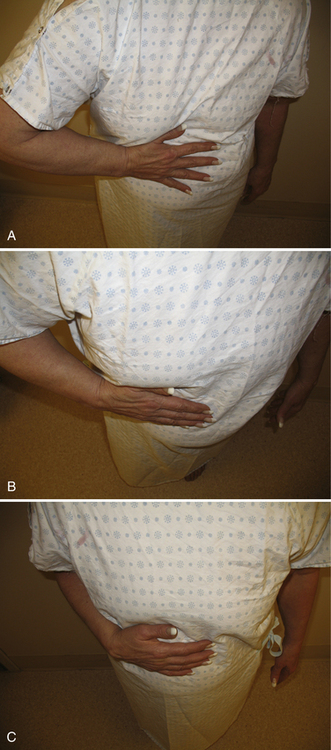
The lift-off test is performed with the affected arm of the patient placed in internal rotation and extension, with the back of the hand on the lumbar region. The test is considered positive if the patient is unable to raise the arm posteriorly off the back.14 Although this test is reliable in patients with complete subscapularis tendon tears, it may not be positive until more than 50% to 75% of the subscapularis tendon is torn. In addition, it is of limited value in patients who cannot bring the affected arm into the starting position because of pain or restricted range of motion. In this case, the belly press test may be used.
To perform the belly press test,15 the patient presses on the abdomen with the palm of the hand and attempts to keep the arm in maximum internal rotation by maintaining the elbow anterior to the midcoronal plane of the body. This test is considered positive if the elbow drops in a posterior direction behind the midcoronal plane while pressure on the abdomen is exerted by extension of the shoulder. A variation is the Napoleon test, which is similarly performed but, in addition to the elbow dropping posteriorly, the wrist commonly palmar-flexes against the abdomen. The amount of wrist flexion has been correlated with the size of subscapularis tendon tearing. Tears of less than 50% of the subscapularis tendon can have negative Napoleon signs (wrist fully extended), tears involving more than 50% but not the entire tendon have an intermediate result (wrist flexed 30 to 60 degrees), and tears involving the entire subscapularis tendon have a positive Napoleon test (wrist flexed 90 degrees; Fig. 22-1).16
Recently, the bear hug test has been described, whereby the patient places the hand of the affected side on the opposite shoulder, with the fingers extended and the shoulder in a forward-flexed position.17 The examiner then tries to pull the patient’s hand off the shoulder using an external rotational force perpendicular to the plane of the forearm as the patient resists. If the examiner is able to lift the patient’s hand off the shoulder, this is considered a positive examination and is suggestive of at least a partially torn subscapularis (Fig. 22-2). In one study, the bear hug test was more sensitive than the belly press test or the lift-off test and may be particularly helpful for partial thickness, upper subscapularis tendon lesions.
DIAGNOSTIC IMAGING
There are few studies that have specifically evaluated the usefulness of diagnostic imaging for the assessment of the subscapularis tendon. Plain radiographs are usually nonspecific but are helpful in ruling out other types of shoulder pathology. In patients with long-standing subscapularis tendon insufficiency, static anterior subluxation of the humeral head may be apparent on axillary radiographs. The use of ultrasound can provide a relatively inexpensive, noninvasive, dynamic assessment of the rotator cuff but is highly observer-dependent. Ultrasound has been reported to be 100% sensitive and 85% specific for the detection of all rotator cuff lesions.18 In this study, ultrasound correctly identified six of seven tears of the subscapularis tendon. In a larger study of 17 isolated subscapularis tendon tears, ultrasonography correctly demonstrated 86% of full-thickness tears of the subscapularis. However, ultrasonography was not as accurate in demonstrating partial-thickness tears, particularly small upper subscapularis tendon tears.19,20
MR arthrography (MRA) has been reported to be 91% sensitive and 86% specific for detecting tears of the subscapularis tendon.21 However, others have reported less promising results and subscapularis tendon tears, particularly full-thickness, upper subscapularis, or partial-thickness tears, are commonly missed by MRI.22 Failure to include T-2 weighted axial images and the experience of the reader have been suggested as contributing to missed subscapularis tendon tears on MRI.
In addition to tendon tearing, the chronicity of the tear and quality of its muscle may be assessed on sagittal oblique images medial to the glenoid. Severe atrophy and fatty degeneration on preoperative MRI or CT generally correlate with poor tendon quality and limited tendon excursion, and may be a negative prognostic sign regarding the ability to repair the subscapularis tendon.23–25 However, others have argued that the subscapularis tendon is commonly reparable, even in the presence of severe atrophy and fatty degeneration and, although not functional, may act as a tenodesis to provide a stable fulcrum of motion.26
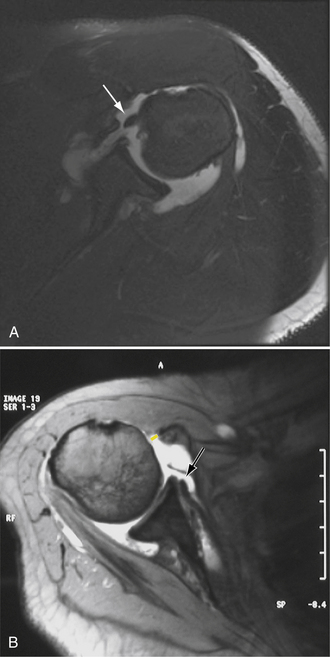
Biceps tendon and rotator interval pathology may be associated with subscapularis tears. The stabilizing reflection pulley of the long head of the biceps tendon may be lost with defects of the superior subscapularis and result in medial subluxation or dislocation of the long head of the biceps tendon (Fig. 22-3A). This may be detected as extravasation of contrast material anterior to the superior border of the subscapularis tendon on axial images. In addition to subscapularis pathology, radiographic evidence of subcoracoid stenosis should be considered. Proximal humeral migration, particularly static anterior subluxation of the humeral head, can contribute to narrowing of the subcoracoid space, especially when imaging studies are obtained with the patient in the supine position (e.g., by MRI).
The more accepted method of measurement is to use the coracohumeral distance, as described earlier (see Fig. 22-3B). A coracohumeral distance of less than 6 mm has been considered as significant evidence of narrowing,6,7,28,29 although its exact role in the pathogenesis of subscapularis tendon tearing is unclear.
INDICATIONS AND CONTRAINDICATIONS
The indications for arthroscopic subscapularis repair are essentially the same as for arthroscopic rotator cuff repair. Patients with significant pain and disability, despite conservative management for 3 to 6 months, are candidates for arthroscopic repair. Acute subscapularis tears should be treated urgently to prevent further retraction and atrophy. In patients with chronic tears, particularly those with significant tendon retraction and fatty infiltration of the subscapularis tendon, arthroscopic repair may still be attempted but the success rate is lower. Alternative treatment including allograft or tendon transfer (e.g., split pectoralis major transfer) may be considered.
TREATMENT OPTIONS
Arthroscopic Technique
Arthroscopic Subscapularis Repair
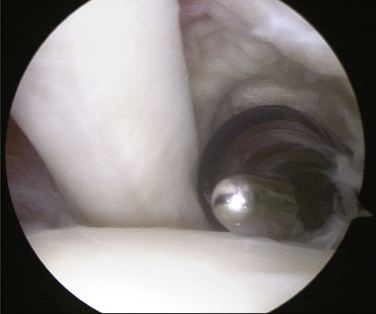
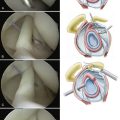
We use a standard posterior portal created 2 to 3 cm inferior and medial to the posterolateral corner of the acromion and a standard anterior portal created 1 cm lateral and 1 cm above the tip of the coracoid. However, the key portal is the anterosuperolateral portal. This portal is created 1 to 2 cm off the anterolateral corner of the acromion, anterior to the supraspinatus tendon and just adjacent to the long head of the biceps tendon. The portal is created tangential to the lesser tuberosity and is the workhorse portal for traction sutures, subscapularis tendon releases, bone bed débridement, suture passage, and knot tying (Fig. 22-4).
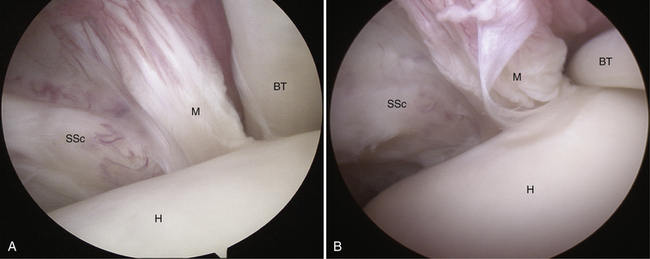
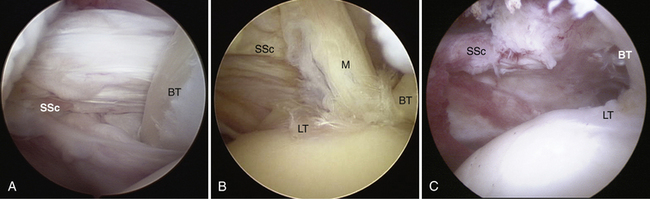
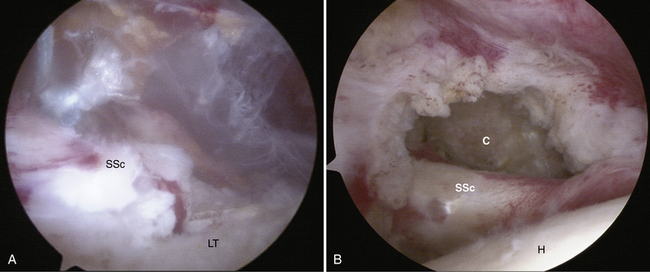
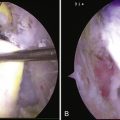
Excellent visualization during arthroscopic subscapularis repair is essential, and is almost exclusively done through a posterior glenohumeral portal. However, to maximize visualization of the subscapularis tendon and its footprint on the lesser tuberosity, the arm is manipulated into abduction, internal rotation, and posterior translation. This draws the fibers of the subscapularis away from the humeral head and increases the anterior working space, revealing the tendon insertion (Fig. 22-5A). A 70-degree arthroscope is used routinely in conjunction with arm positioning to maximize visualization (see Fig. 22-5B). By using a combination of arm positioning and a 70-degree arthroscope, a top-down view of the subscapularis tendon and the entire footprint may be obtained with careful evaluation of the relationship among the subscapularis tendon insertion, medial sling, and biceps tendon (Fig. 22-6). Occasionally, viewing through the anterosuperolateral portal can be beneficial.
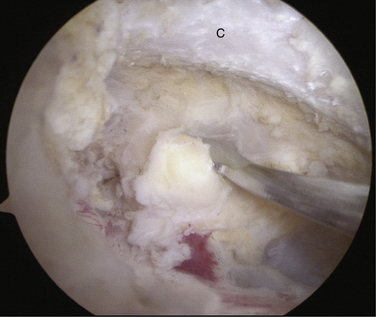
Once a subscapularis tendon tear has been identified, delineating the margins of the subscapularis tendon follows. Identification of the subscapularis tendon in partial-thickness or full-thickness partial width tears is relatively uncomplicated. However, in chronic complete disruptions, the tendon stump is commonly retracted medially and scarred to the deltoid fascia. This obscures both the lateral and superior borders of the subscapularis stump and can make the tendon difficult to locate.13
The key to finding the subscapularis and differentiating it from the deltoid, conjoined tendon, and coracoacromial ligament is to locate the comma sign. By identifying this comma-shaped arc of tissue, this tissue can then be followed inferiorly and medially to the superolateral border of the subscapularis tendon (Fig. 22-7). Applying traction along the crook of the comma draws out the subscapularis tendon from behind the glenoid, and the superior and lateral borders of the subscapularis tendon may be identified.
Concomitant pathologic involvement of the long head of the biceps tendon occurs in 31% to 56% of cases and may include subluxation, dislocation, or rupture.15,31 Subluxation of the biceps caused by disruption of the medial sling can stress the subscapularis repair and cause eventual failure. Even in cases in which the biceps tendon is not subluxated, some have recommended routine tenotomy or tenodesis, which is associated with improved subjective and objective results, independent of the preoperative condition of the biceps tendon.32 In general, a biceps tenodesis may be performed except in older, lower demand patients, for whom a simple biceps tenotomy will usually suffice. The primary feature is to tag and release the biceps tendon early in the procedure to maximize visualization for subsequent anterior shoulder work (e.g., subscapularis tendon releases, bone bed preparation). Tenodesis should be performed low in the bicipital groove, after subscapularis tendon releases but prior to definitive tendon fixation to bone.
The next step is to mobilize the subscapularis tendon.16,26 Releases start superiorly and proceed anteriorly and posteriorly. Occasionally, a lateral release is also required in chronic tears that are adherent to the subdeltoid fascia. Inferior dissection is rarely required and avoids violation of the axillary nerve.
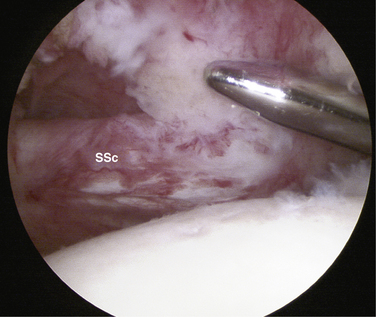
A window is created through the rotator interval to expose the coracoid (an interval slide in continuity).33 Instruments (e.g., cautery, shaver) are introduced through the anterosuperolateral portal and traction on the subscapularis tendon by the traction stitch draws the superior border of the subscapularis tendon into view. Soft tissue resection proceeds superior to the subscapularis border, keeping the lateral rotator interval tissue (the comma sign) intact. The firm coracoid can be palpated through the soft interval tissue, which is then resected. Viewing with a 70-degree arthroscope can assist in visualizing the medial aspect of the superior border of subscapularis tendon behind the glenoid while the superior adhesions are released (Fig. 22-8A). Dissection must remain lateral to the coracoid. Preservation of the subscapularis and medial sling arc is important because it helps maintain the integrity of the subscapularis tendon and can greatly facilitate posterosuperior rotator cuff repair following subscapularis tendon repair (see Fig. 22-8B).28,33
The anterior release is begun next by introducing the 70-degree arthroscope through the window, which provides a top-down view of the structures anterior to the subscapularis tendon. The coracoid tip, neck, and base are identified. Instruments (e.g., shaver, cautery) are now introduced through the anterosuperolateral portal but are directed anterior to the subscapularis tendon (Fig. 22-9). Fibrofatty tissue is removed from the subcoracoid space and the posterolateral aspect of the coracoid is skeletonized, releasing the coracohumeral ligament (Fig. 22-10).
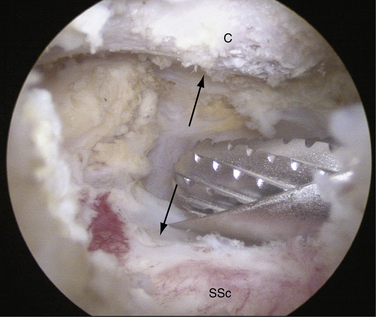
A minimal coracoplasty may be performed in the plane of the subscapularis tendon using a burr through the anterosuperolateral portal.34 Care is taken to protect the inferior conjoined tendon and superolateral coracoacromial ligament. The goal of the coracoplasty is to create a 7- to 10-mm space between the posterolateral tip of the coracoid and anterior plane of the subscapularis tendon. Subcoracoid decompression increases the anterior working space available during arthroscopic repair and may protect the repaired subscapularis from abrasion (Fig. 22-11).
The posterior release is performed next and the arthroscope is withdrawn posteriorly out the rotator interval window. Using a combination of cautery and an elevator, the subscapularis tendon is released from the middle glenohumeral ligament and anterior capsule (Fig. 22-12). With a three-sided release (i.e., superior, anterior, posterior), sufficient mobility is usually obtained for tendon repair to bone.
However, in some cases, a lateral release may also be necessary (Fig. 22-13); this is easiest to perform prior to the other releases described earlier. This is particularly relevant in chronic adhesed cases in which the lateral margin of the subscapularis tendon is scarred to the inner deltoid fascia, coracoid, and conjoint tendon. In such cases, the lateral margin must be delineated (using the comma sign as a guide) and the soft tissue bursal leader lateral to the tendon is resected. The dissection continues inferior until the subscapularis tendon is released from the anterior structures and the subcoracoid space is reconstituted.
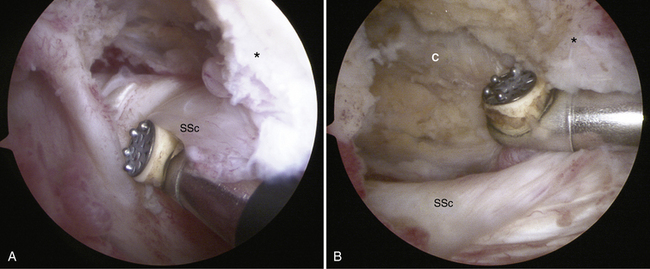
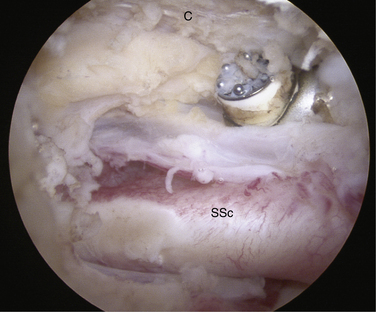
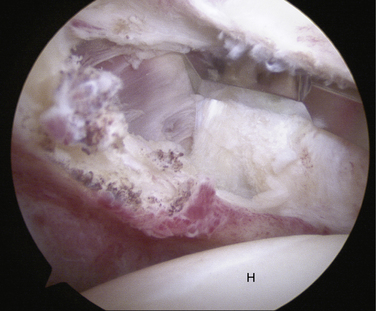
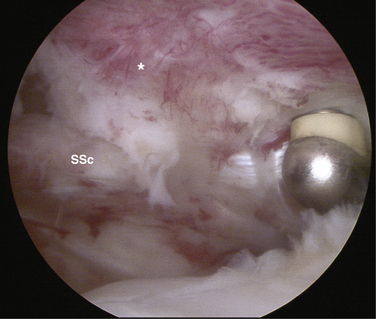
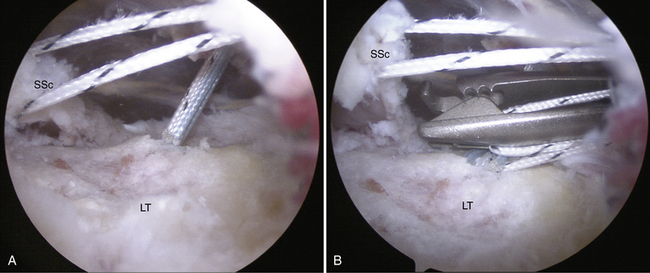
Following preparation of the bone bed, standard suture anchor insertion, suture passage, and knot-tying are carried out. Beginning inferiorly, anchors (BioCorkscrew FT, Arthrex) are percutaneously inserted in the lesser tuberosity using needle localization at a dead man’s angle (less than45 degrees to the bone bed; Fig. 22-14A). Percutaneous anchor portal placement is usually 1 to 2 cm inferior and medial to the position of the anterosuperolateral portal but can change according to the position of the arm. Although retrograde suture passage is possible, this generally is more complex and requires a hand-off technique. Antegrade suture passage through the anterosuperolateral portal is usually easier (see Fig. 22-14B) using the percutaneous anchor portal for suture management. To facilitate suture management and maximize visualization, tying as you go is a reasonable technique. The repair proceeds from inferior to superior with subsequent anchor insertion, suture passage, and knot tying. Usually, two or three double-loaded anchors are required for a complete subscapularis tendon tear (Fig. 22-15).
Arthroscopic Débridement
Débridement alone may be performed in carefully selected patients in whom tears are thought to be irreparable, or in older patients who are unwilling to participate in the rehabilitation program required after a repair. Acceptable results may be obtained with arthroscopic débridement, particularly in conjunction with biceps tenotomy.30
PEARLS& PITFALLS
CONCLUSIONS
Arthroscopic repair of the subscapularis tendon is a relatively difficult procedure and is best performed by arthroscopists already familiar with arthroscopic rotator cuff repair. However, by adherence to the principles of maximizing visualization, delineating the margins of the subscapularis, and releasing and mobilizing the subscapularis, standard suture anchor-based techniques may be used for successful arthroscopic tendon repair to bone.
1. Burkhart SS, Lo IK. Arthroscopic rotator cuff repair. J Am Acad Orthop Surg. 2006;14:333-346.
2. Bennett WF. Subscapularis, medial and lateral head coracohumeral ligament insertion anatomy. Arthroscopic appearance and incidence of “hidden” rotator interval lesions. Arthroscopy. 2001;17:173-180.
3. Kim TK, Rauh PB, McFarland EG. Partial tears of the subscapularis tendon found during arthroscopic procedures on the shoulder. A statistical analysis of sixty cases. Am J Sports Med. 2003;31:744-750.
4. D’Addesi LL, Anbari A, Reish MW, et al The subscapularis footprint: an anatomic study of the subscapularis tendon insertion. Arthroscopy, 22; 2006:937-940.
5. Curtis AS, Burbank KM, Tierney JJ, et al The insertional footprint of the rotator cuff: an anatomic study. Arthroscopy, 22; 2006:603-609.
6. Lo IK, Burkhart SS The etiology and assessment of subscapularis tendon tears: a case for subcoracoid impingement, the roller-wringer effect, and TUFF lesions of the subscapularis. Arthroscopy, 19; 2003:1142-1150.
7. Gerber C, Terrier F, Sehnder R, Ganz R. The subcoracoid space. An anatomic study. Clin Orthop. 1987;215:132-138.
8. Friedman RJ, Bonutti PM, Genez B. Cine magnetic resonance imaging of the subcoracoid region. Orthopedics. 1998;21:545-548.
9. Richards DP, Burkhart SS, Campbell Scot E. Relation between narrowed coracohumeral distance and subscapularis tears. Arthroscopy. 2005;21:1223-1228.
10. Nove-Josserand L, Boulahia A, Levigne C, et al. Coracohumeral space and rotator cuff tears. Rev Chir Orthop Reparatrice Appar Mot. 1999;85:677-683.
11. Sakurai G, Ozaki J, Tomita Y, et al Incomplete tears of the subscapularis tendon associated with tears of the supraspinatus tendon: cadaver and clinical studies. J Shoulder Elbow Surg, 8; 1999:574-579.
12. Sano H, Ishii H, Trudel G, Uhthoff HK Histologic evidence of degeneration at the insertion of 3 rotator cuff tendons: a comparative study with human cadaveric shoulder. J Shoulder Elbow Surg, 8; 1999:574-579.
13. Lo IK, Burkhart SS The comma sign: arthroscopic guide to the torn subscapularis tendon. Arthroscopy, 19; 2003:334-337.
14. Gerber C, Krushell RJ. Isolated rupture of the tendon of the subscapularis muscle. Clinical features in 16 cases. J Bone Joint Surg Br. 1991;73:389-394.
15. Gerber C, Hersche O, Farron A. Isolated rupture of the subscapularis tendon. J Bone Joint Surgery Am. 1996;78:1015-1023.
16. Burkhart SS, Tehrany AM Arthroscopic subscapularis tendon repair: technique and preliminary results. Arthroscopy, 18; 2002:454-463.
17. Barth JRH, Burkhart SS, de Beer JF The bear-hug test: a new and sensitive test for diagnosing a subscapularis tear. Arthroscopy, 22; 2006:1076-1084.
18. Teefey SA, Hasan SA, Middleton WD, et al Ultrasonography of the rotator cuff: a comparison of ultrasonographic and arthroscopic findings in one hundred consecutive cases. J Bone Joint Surg Am, 82; 2000:498-504.
19. Teefey SA, Middleton WD, Payne WT, Yamaguchi K Detection and measurement of rotator cuff tears with sonography: analysis of diagnostic errors. Am J Radiol, 184; 2005:1768-1773.
20. Farin P, Jaroma H. Sonographic detection of tears of the anterior portion of the rotator cuff (subscapularis tendon tears). J Ultrasound Med. 1996;16:221-225.
21. Pfirrmann CW, Zanette M, Weishaupt D, et al Subscapularis tendon tears: detection and grading at MR arthrography. Radiology, 213; 1999:709-714.
22. Tung GA, Yoo DC, Levine SM, Green A Subscapularis tendon tear: primary and associated signs on MRI. J Comput Assist Tomogr, 25; 2001:417-424.
23. Goutallier D, Postel JM, Bernageau J, et al. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78-83.
24. Goutallier D, Postel MN, Bernageau J, et al. Fatty infiltration of disrupted rotator cuff muscles. Rev Rhum Engl Ed. 1995;63:415-422.
25. Ticker JB, Warner JJ Single-tendon teas of the rotator cuff: evaluation and treatment of suscapularis tears and principles of treatment for supraspinatus tears. Orthop Clin North Am, 28; 1997:99-116.
26. Burkhart SS, Brady PC Arthroscopic subscapularis repair: surgical tips and pearls from A to Z. Arthroscopy, 22; 2006:1014-1027.
27. Dines DM, Warren RF, Inglis AE, Pavlov H. The coracoid impingement syndrome. J Bone Joint Surg Br. 1990;72:314-316.
28. Lo IK, Parten PM, Burkhart SS Combined subcoracoid and subacromial impingement in association with anterosuperior rotator cuff tears: an arthroscopic approach. Arthroscopy, 19; 2003:1068-1078.
29. Nove-Josserand L, Edwards TB, O’Connor DP, Walch G. The acromiohumeral and coracohumeral intervals are abnormal in rotator cuff tears with muscular fatty degeneration. Clin Orthop Relat Res. 2005;433:90-96.
30. Edwards TB, Walch G, Nove-Josserand L, et al. Arthroscopic debridement in the treatment of patients with isolated tears of the subscapularis. Arthroscopy. 2006;22:942-946.
31. Deutsch A, Altchek DW, Veltri DM, et al Traumatic tears of the subscapularis tendon: Clinical diagnosis, magnetic resonance imaging findings and operative treatment. Am J Sports Med, 25; 1997:13-22.
32. Edwards TB, Walch G, Sirveaux F, et al. Repair of tears of the subscapularis. J Bone Joint Surg Am. 2005;87:725-730.
33. Lo IK, Burkhart SS The interval slide in continuity: a method of mobilizing the anterosuperior rotator cuff without disrupting the tear margins. Arthroscopy, 20; 2004:435-441.
34. Lo IK, Burkhart SS. Arthroscopic coracoplasty through the rotator interval. Arthroscopy. 2003;19:667-671.