Streptococcal Infections
At the conclusion of this chapter, the reader should be able to:
• Describe the etiology, epidemiology, signs and symptoms, and complications of streptococcal infection.
• Discuss the immunologic manifestations and diagnostic evaluation of streptococcal infection.
• Analyze and apply laboratory data to a case study.
• Correctly answer case study related multiple choice questions.
• Be prepared to participate in a discussion of critical thinking questions.
• Explain the principle and applications of the classic anti–streptolysin O (ASO) procedure.
• Briefly explain other methods of detection of group A streptococcus.
Etiology
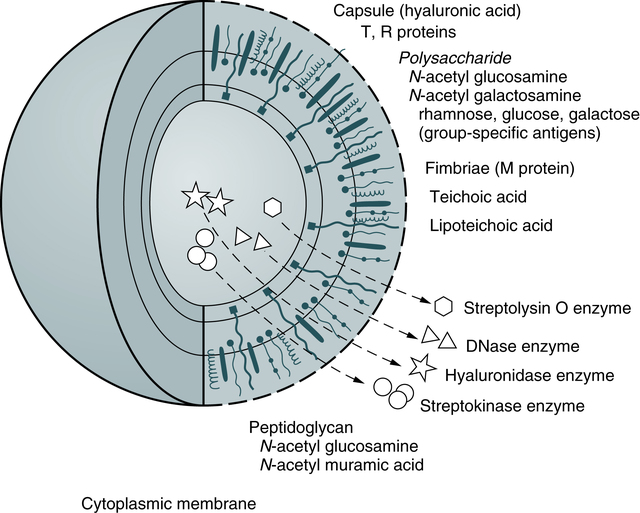
Most streptococci that contain cell wall antigens of the Lancefield group A (Table 17-1) are known as Streptococcus pyogenes. Members of this species are almost always beta-hemolytic streptococci. S. pyogenes is the most common causative agent of pharyngitis and its resultant disorder, scarlet fever, and the skin infection, impetigo. The most common type of bacteria causing necrotizing fasciitis is S. pyogenes.
Table 17-1
Lancefield Streptococcus Classifications∗
| Lancefield Group | Examples of Bacterial Species in the Group | Comments |
| A | Streptococcus pyogenes | Strains most pathogenic for human beings can cause strep throat, rheumatic fever, scarlet fever, acute glomerulonephritis, and necrotizing fasciitis. |
| B | Streptococcus mastitis Streptococcus agalactiae |
Strains from mastitis in cows and from normal milk, including strains from the human throat and vagina Can cause pneumonia and meningitis in neonates and older adults, with occasional systemic bacteremia |
| C | Streptococcus equii Streptococcus dysgalactiae |
Strains from various lower animals, including cattle, and from the human throat Can cause pharyngitis and other pyogenic infections similar to group A streptococci |
| D | Streptococcus faecalis (now Enterococcus faecalis) Other nonenterococcal group D strains include Streptococcus bovis and Streptococcus equinus. |
Strains from cheese and humans Many former group D streptococci have been reclassified and placed in the genus Enterococcus. |
| E | Strains from certified milk | |
| F | Streptococcus anginosus (Lancefield classification) or Streptococcus milleri group (European system) | Strains mainly from the human throat, associated with tonsillitis; minute hemolytic |
| G | Streptococcus canis is an example of a GBS Group B streptococcus (GBS) which is typically found in animals, but does not cause infection except in newborns at birth | Strains can cause infection in human beings (a few strains from monkeys and dogs). Note: This is not exclusively beta-hemolytic. |
| H, K, O | Nonpathogenic strains occasionally from normal human respiratory tracts |
∗This is a serologic classification of hemolytic streptococci, dividing them into groups based on antigenic serocharacteristics. It is based on precipitation tests depending on group-specific carbohydrate substances.
Extracellular Products
• Streptolysin O (SLO), an oxygen-labile enzyme, binds to sterols in the red blood cell (RBC) membrane, causing stearic rearrangement. This rearrangement produces submicroscopic holes in the RBC membrane and hemoglobin diffuses from the cells. SLO is antigenic; the antibody response to it is the most frequently used serologic indicator of recent streptococcal infection.
• Streptolysin S, an oxygen-stable enzyme, is responsible for the beta (clear-appearing) hemolysis on the surface of a blood agar culture plate. Streptolysin S disrupts the selective permeability of the RBC membrane, causing osmotic lysis. It is not antigenic.
• Other substances produced by group A streptococci presumably facilitate rapid spread through subcutaneous or deeper soft tissues and include the following:
• Hyaluronidase, also called spreading factor, breaks down hyaluronic acid found in the host’s connective tissue.
• Four immunologically distinct deoxyribonucleases (DNases A, B, C, and D) degrade deoxyribonucleic acid (DNA).
• Streptokinase, an enzyme, dissolves clots by converting plasminogen to plasmin.
• Other extracellular products that can elicit an antibody response include NADase, proteinase, esterase, and amylase.
• Erythrogenic toxin is elaborated by scarlet fever–associated strains and is responsible for the characteristic rash.
Signs and Symptoms
Impetigo and Cellulitis
Impetigo is a skin infection that begins as a papule (Fig. 17-2). The lesion may itch and will eventually crust over and heal. Cellulitis caused by subcutaneous infection with group A streptococci is associated with a warm, red, tender area that may be mildly swollen. Erysipelas, a distinct cellulitis syndrome, usually involves the face and may be associated with pharyngitis. This syndrome is characterized by toxicity and a high fever. If left untreated, erysipelas can be fatal.
Immunologic Manifestations
Most infected patients demonstrate increased concentration of antibody against SLO. The concentration of antibody (titer) begins to rise about 7 days after the onset of infection and reaches a maximum after 4 to 6 weeks. A rise in titer of 50 Todd units∗ in 1 to 2 weeks is of greater diagnostic significance than a single titer.
Diagnostic Evaluation
In addition to throat cultures in patients with pharyngitis, antibodies to bacterial toxins and other extracellular products that display measurable activity can be tested. ASO and ADN-B are the standard serologic tests. The ability of a patient’s serum to neutralize the erythrocyte-lysing capability of SLO (ASO procedure) has been used for many years as a method for detecting previous streptococcal infection. After an infection such as pharyngitis with SLO-producing strains, most patients show a high titer of the antibody ASO. The use of rapid testing (see ASO latex procedure, Chapter 12, and Chapter 14) has replaced the use of the classic ASO procedure archived on the EVOLVE website (and on www.mlturgeon.com).
Chapter Highlights
• Most streptococci that contain cell wall antigens of Lancefield group A are known as Streptococcus pyogenes. Members of this species are almost always beta-hemolytic streptococci.
• S. pyogenes is important in the development of complications such as acute rheumatic fever and poststreptococcal glomerulonephritis.
• Strains of S. pyogenes that lack M protein cannot cause infection.
• Extracellular products are important in the pathogenesis and serologic diagnosis of streptococcal disease. Antibodies produced in response to these substances indicate recent streptococcal infection.
• Substances produced by group A streptococci presumably facilitate rapid spread through subcutaneous or deeper soft tissues.