4
Strength
1. Name the noncontractile and contractile elements of muscle tissue.
2. Give examples of concentric and eccentric contractions.
3. State two definitions of strength.
4. List methods used to measure strength.
5. Compare muscle contraction types related to tension produced and energy liberated.
6. Identify clinical features of delayed onset muscle soreness (DOMS).
7. List three clinically relevant exercise programs to enhance strength.
8. Explain opened and closed kinetic chain exercise.
9. Identify goals and applications of strength training programs for the elderly.
Strength training is physical activity intended to increase muscle strength and mass.46 Adults who engage in strength training are less likely to experience loss of muscle mass and functional decline.63
Maintaining, enhancing, and regaining strength are critical for improving body function during all phases of recovery after surgery, injury, or disease affecting the musculoskeletal system. Strength training, resistance training, and weight training are synonymous and refer to physical conditioning that uses isometric, isotonic, or isokinetic exercise to develop muscle.28 Resistance exercise is any form of active exercise in which a dynamic or static muscle contraction is resisted by an outside force, applied either manually or mechanically. Therapeutic exercise is resistance training that is applied in a systematic and individualized manner designed to improve, restore, or enhance physical function. The physical therapist assistant (PTA) must understand the basic foundations of strength development and, more importantly, how to apply principles of strength gaining during recovery after immobilization, surgery, or musculoskeletal injury. In this chapter the PTA is introduced to basic concepts and universally accepted principles that can be applied in numerous clinical situations with various orthopedic pathologies.
A muscle’s strength or tension-generating capacity is determined by a number of diverse but interrelated factors, including neural control (motor unit recruitment and rate coding; the number and rate at which the motor units are fired), cross-sectional area (muscle fiber number and size), muscle fiber arrangement (angle of pennation or how fibers are aligned in relation to a imaginary line between the muscle’s origin and insertion), muscle length (length tension ratio; muscle produces the greatest tension when it is near or at the physiologic resting position at the time of contraction), angle of pull (muscle’s tension generating capacity is increased when the tendon is perpendicular to the bone), and fiber type distribution (high percent of type I: low force production, fatigue resistant; or type IIA and IIB: high force production, rapid fatigue).6,41 One also has to consider other factors, such as energy stores of the muscle, recovery from exercise, fatigue, age, gender, and state of health of the muscle; they may effect tension generation.
GENERAL MUSCLE BIOLOGY
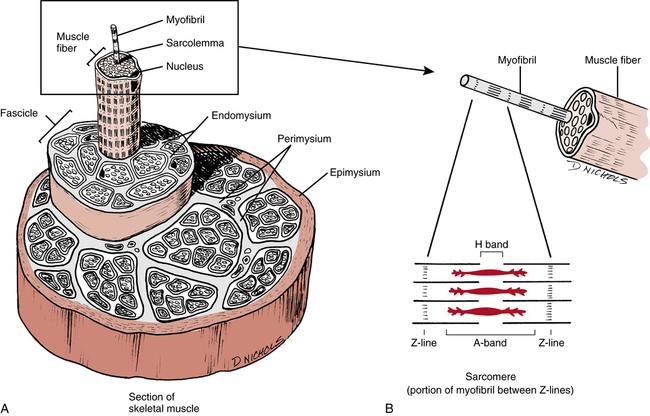
The body of an individual muscle is surrounded by noncontractile connective tissue called the epimysium. Within the muscle are bundles of fibers called fasciculi, which are surrounded by another noncontractile connective tissue called the perimysium. The endomysium is a noncontractile connective tissue that surrounds each individual muscle fiber. The individual muscle fibers are composed of myofibrils that lie parallel to each other and the muscle fiber itself (Fig. 4-1, A). The structural components of the myofibrils are called myofilaments, and they comprise two predominant proteins, actin and myosin. The functional, or contractile, unit of a muscle fiber cell is called the sarcomere (Fig. 4-1, B). Myosin (a thick protein) and actin (a thin protein) are actively involved with the mechanics of muscular contraction, which involves a complex and highly structured series of chemical and mechanical events.
Muscle Fiber Types
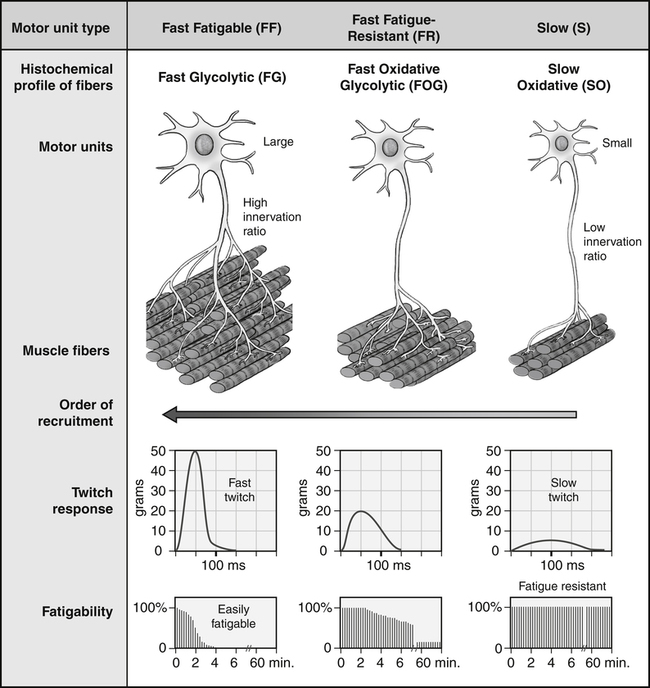
Generally two distinct types of muscle fibers have been identified in humans. These fibers are classified by their contractile and metabolic characteristics (Fig. 4-2).
Type II fibers can be further broken down into three distinct subclassifications: type IIA; type IIAB; and type IIB.49,73 These fiber types differ mainly in terms of contraction velocity and endurance and are classified as intermediate fiber types with both aerobic and anaerobic capacities.
 The type IIA (fast-oxidative-glycolytic [FOG]) fiber has a fast contraction speed and a moderate capacity for energy transfer from both aerobic and anaerobic sources.
The type IIA (fast-oxidative-glycolytic [FOG]) fiber has a fast contraction speed and a moderate capacity for energy transfer from both aerobic and anaerobic sources.
 The type IIB (fast-glycolytic [FG]) fiber possesses the greatest anaerobic capacity and the fastest shortening speed.
The type IIB (fast-glycolytic [FG]) fiber possesses the greatest anaerobic capacity and the fastest shortening speed.
 The type IIAB fiber is rare and undifferentiated and may contribute to reinnervation and motor unit transformation.
The type IIAB fiber is rare and undifferentiated and may contribute to reinnervation and motor unit transformation.
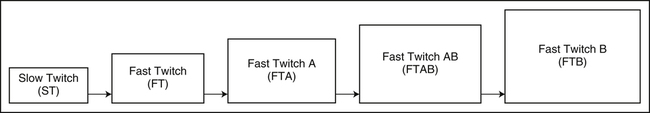
The motor unit is the basic unit of movement. It consists of the anterior motor neuron and all the muscle fibers it innervates. A motor unit contains only one specific muscle fiber type. Motor unit recruitment is the adding of motor units to increase force. The Henneman size principle proposes an orderly recruitment of motor units within a motor neuron pool during a defined movement task.36a When a low force is needed, only the slow twitch motor units (type I) are activated; and with increasing force requirements, larger and faster motor units (type IIA, type IIB) are recruited. Therefore the orderly recruitment of muscle fibers during contraction proceeds according to increased force requirements, as shown in Fig. 4-3.
TYPES OF MUSCLE CONTRACTIONS
Concentric
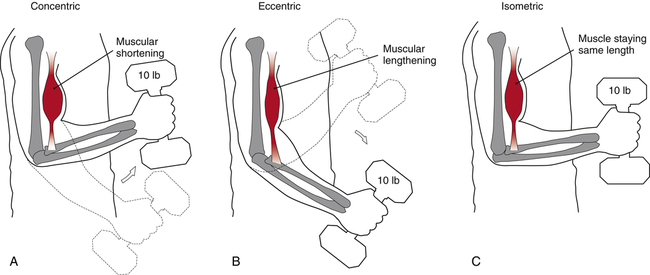
In a concentric contraction, tension is produced and shortening of the muscle takes place (Fig. 4-4, A). The action produced by a concentric contraction brings together or approximates the origin and insertion of the contracting muscle. In a concentric exercise, tension is developed and shortening of the muscle occurs to overcome an external force, such as a weight.
Eccentric
An eccentric muscle contraction is sometimes referred to as a lengthening contraction. In an eccentric contraction, tension is produced; however, lengthening of the muscle occurs so that the net action is opposite that produced by a concentric contraction (Fig. 4-4, B). The origin and insertion of the contracting muscle move farther apart during the contraction. Eccentric exercise involves loading of a muscle, causing a physical lengthening of the muscle as it attempts to control the load when lowering the weight. For example, as one slowly descends to sit in a chair and moves from a standing to a sitting position, the quadriceps muscles must eccentrically contract to control the rate of descent or one would suddenly fall into the chair.
Isometric
In an isometric contraction, tension is produced but no joint movement or action takes place (Fig. 4-4, C). Isometric exercise involves a muscle contraction against a force with no significant movement occurring. Examples include pushing or pulling against an immovable object or holding a weight in a particular position. Isometric exercises are used when joint movement is restricted or not possible. A form of isometric exercise is a muscle-setting exercise. Setting exercises are muscle contractions performed without movement or resistance. An example is a quadriceps set, or quad set. (The word “set” is used to describe an isometric contraction.) If the quadriceps contracts as a knee is held straight, tension is produced within the muscle but no change in joint angle takes place. Clinically, setting exercises are used to decrease pain, facilitate muscle contraction, increase circulation, and retard muscle atrophy.
Isotonic
An isotonic muscle contraction is not an accurate name for what happens physiologically. The name implies that the resistance, force, load, or tension remains constant, but actually the tension or force created in a muscle during this type of action must change as the joint angle changes. For example, when one lifts a barbell (constant resistance), the amount of force generated by the contracting muscle varies at different angles during the movement, even though the weight itself remains constant. This occurs because changes in the muscle length as well as the muscle tendon’s angle of pull alter the mechanical advantage of the muscle throughout the movement, resulting in variations of force developing capacity. Therefore a more precise and descriptive term, isoinertial,55 can be used in place of isotonic. The term isotonic is used in this book to describe the action of variable velocities of movement with a constant load. Examples of isotonic resistance equipment are barbells, dumbbells, and ankle weights, which are collectively referred to as free weights.
DEFINITIONS OF STRENGTH AND POWER
Strength is a broad term. Generally strength is the ability of a muscle to generate force, or more specifically the maximum force generated by a single muscle or related muscle group.50 Other definitions of strength include “The ability to exert force under a given set of conditions defined by body position, the body movement by which force is applied, movement type, and movement speed”36 and “The maximal force a muscle or muscle group can generate at a specified velocity.”45 The American Physical Therapy Association defines muscle strength as “the muscle force exerted by a muscle or group of muscles to overcome resistance under specific set of circumstances”; muscle performance as “the capacity of a muscle or group of muscles to generate forces”; muscle power as “the work produced per unit time or the product of strength and speed”; and muscle endurance as “the ability to sustain forces repeatedly or to generate forces over a period of time.”5 Functional strength has been described as the ability of the neuromuscular system to produce, reduce, or control forces, contemplated or imposed, during functional activities, in a smooth, coordinated manner.41
 Work is used to describe the result or product of a force exerted on an object and the distance the object moves.36
Work is used to describe the result or product of a force exerted on an object and the distance the object moves.36
 Force can be described as either linear or rotary.66
Force can be described as either linear or rotary.66
 Linear force is described as Force = Mass × Acceleration.
Linear force is described as Force = Mass × Acceleration.
 Rotary force is expressed as Force = Mass × Angular acceleration.
Rotary force is expressed as Force = Mass × Angular acceleration.
 Torque is the ability to cause rotational movement.
Torque is the ability to cause rotational movement.
 Power is defined as the time rate of doing work, which can be expressed in several ways.55
Power is defined as the time rate of doing work, which can be expressed in several ways.55
 Velocity is defined as a vector that describes displacement.
Velocity is defined as a vector that describes displacement.
Overall, these terms help describe resultant muscular performance as they relate to the development of strength.
MEASURING STRENGTH
Strength can be measured by six methods:
Manual muscle testing (MMT) is a isometric method of muscle testing that is designed to measure muscle strength requiring no equipment other than the examiner’s hands. This technique was introduced in the early 1900s and its use is widely accepted in the health care professions.61 It is used to generally grade a muscle’s isometric contraction capacity at a specific joint angle against a manually applied force or gravity. Performing a MMT requires extensive time, effort, and attention to detail while performing the correct technique to ensure that the results obtained are as accurate as possible.61 The tester must have a comprehensive and detailed understanding of kinesiology to accurately and consistently reproduce manual grading of muscle strength (performance). The grading scale for this test is clinically easy to use and is outlined in Table 4-1. The disadvantage of isometric strength testing is that because muscle length is held constant, isometric strength testing provides muscle strength data at only one point in the range.59 MMT is valid from grades 0 to 5; however, when MMT scores exceed grade 4, the MMT loses it ability to discriminate between gradations of strength. In cases where measurement and documentation of strength level is critical above a MMT grade 4, an alternative form of measuring strength should be used.59
Table 4-1
| Score | Description |
| Grade 5/Normal | Patient can hold the position against maximum resistance, has complete range of motion. There is a wide range of normal. |
| Grade 4/Good | Patient can hold the position against strong to moderate resistance, and has full range of motion. Grade 4/good and below represents true clinical weakness. |
| Grade 3+/Fair + | Patient can complete a full range of motion against gravity and hold end position against mild resistance. |
| Grade 3/Fair | Patient can tolerate no resistance but can perform the movement through the full range of motion. |
| Grade 2+/Poor + | Patient has full range of motion in the gravity eliminated position and can take some resistance. |
| Grade 2/Poor | Patient has full range of motion in the gravity eliminated position. |
| Grade 2−/Poor – | Patient can complete partial range of motion in the gravity eliminated position. |
| Grade 1/Trace | The examiner can detect visually or by palpation some contractile activity. |
| Grade 0/Zero | The muscle is completely quiescent on palpation or visual inspection. |
From Hislop HJ, Montgomery J: Daniels and Worthingham’s muscle testing: techniques of manual examination, ed 7, St Louis, 2002, Saunders.
Cable tensiometry is used to isometrically measure a muscle’s strength (Fig. 4-5). Essentially this tool is a mechanical form of manual muscle testing. The tensiometer provides the advantage of versatility for recording force measurements at virtually all angles of a joint’s ROM and may be more sensitive for grading muscle strength above grade 4. This method is used primarily to measure strength in normal subjects in research projects. Many tests were developed in the 1950s to describe static force or isometric strength by use of the cable tension method.15,16
Dynamometry is used extensively in physical therapy. Hand-held dynamometers (Fig. 4-6) are used to quantify grip strength, and the standing-back dynamometer is used to evaluate back extension strength. In this latter example, many factors contribute to the subject’s ability to generate tension or force during the back pull, including the patient’s motivation, degree of pain (if any), arm length, leg length, height, weight, and the obvious contribution from other muscle groups. These variables make dynamometry an unreliable, nonspecific testing tool.
An isotonic one-repetition maximum lift is used to test strength using commercially available exercise equipment or barbells and dumbbells. In this method the patient performs a single, full ROM lift, such as a bench press (Fig. 4-7), shoulder press, or arm curl, for a particular muscle group. Applying this method is difficult because the tester and patient must first establish a reasonable starting weight through trial and error, fatigue becomes a factor if many trials are needed, and precise performance or execution of the proper lift is determined subjectively by the tester. This method is best used for normal subjects, in a sports medicine environment, or with uninvolved body parts not necessary for stabilization of a disabled joint.
Perhaps the most widely used and clinically relevant method of objective, reproducible strength testing is through isokinetics. The data collected with isokinetic testing document strength (force production), torque, power, and work.60 As stated, isokinetics employs a fixed speed, or velocity, of movement that allows for maximum loading throughout the full ROM. If a patient experiences pain during any part of the test, or does not apply a maximum force throughout the entire ROM, the velocity remains constant with a variable resistance that is totally accommodating to the individual.19 To test for strength, slow speeds (30° to 60° per second) are generally used.48 Because isokinetic equipment can be interfaced with computers, a hard-copy graph of the data can be used for evaluation and exercise prescription. In addition to being a valid and reliable tool for strength testing, isokinetics also can evaluate neuromuscular endurance, speed of muscle contraction, and muscular power.40
The determination of an individual’s readiness to return to normal levels of activity is a common issue in rehabilitation. To resolve this issue, clinicians have incorporated functional testing following rehabilitation. Functional testing involves the evaluation of broad skills necessary to perform complex movements versus traditional methods that focus on isolated joint testing. This is particularly important when dealing with athletes who may be returned to activity too soon after rehabilitation because of inaccuracies in the assessment of their functional ability resulting from more traditional assessment methods.18
Examples include the following:
 One-leg hop for distance: The patient performs a single-leg hop for distance with each lower extremity.
One-leg hop for distance: The patient performs a single-leg hop for distance with each lower extremity.
 Single-leg triple hop for distance: The patient performs a single-leg triple hop for distance with each lower extremity.
Single-leg triple hop for distance: The patient performs a single-leg triple hop for distance with each lower extremity.
 Timed single-leg hop (minitrampoline): The patient hops on the trampoline a maximum number of times in 30 seconds.
Timed single-leg hop (minitrampoline): The patient hops on the trampoline a maximum number of times in 30 seconds.
 Vertical jump: The patient performs a two-legged vertical jump for height.
Vertical jump: The patient performs a two-legged vertical jump for height.
COMPARISON OF MUSCLE CONTRACTION TYPES
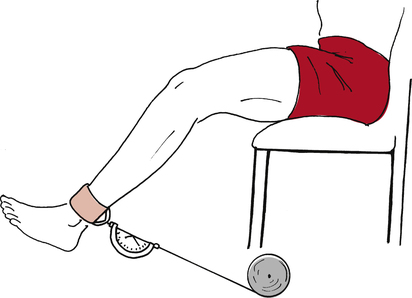
Generally, muscle contractions are characterized by the amount of tension the contraction produces and the amount of energy liberated (ATP use) by the contraction. The most common clinically applicable way to strengthen muscle is with concentric and eccentric contractions using isotonic (isoinertial)55 progressive resistive exercise (PRE). Ankle or cuff weights, hand-held weights (dumbbells), and weight machines are examples of isotonic equipment used in physical therapy practice.∗ Elftman23 has demonstrated that the production of maximal force of contraction by various methods occurs in a predictable fashion, as seen in Fig. 4-8.
The force of contraction is expressed as the amount of tension developed per unit of contractile tissue. In terms of energy liberated (ATP use), eccentric muscle contractions use the least ATP, and concentric contractions use the most (Fig. 4-9).3
Based on this information, it appears that eccentric muscle contractions are more energy efficient and produce greater tension per contractile unit than both concentric and isometric contractions. However, Davies19 points out that much of the tension produced by eccentric muscle contraction results from stress imposed on the noncontractile serial elastic components (perimysium, epimysium, and endomysium) of the muscle. Therefore eccentric muscle contractions stimulate both contractile and noncontractile elements, whereas concentric contractions and isometrics focus on the contractile elements.60
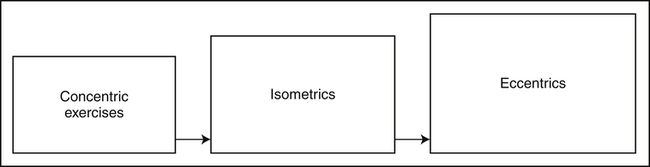
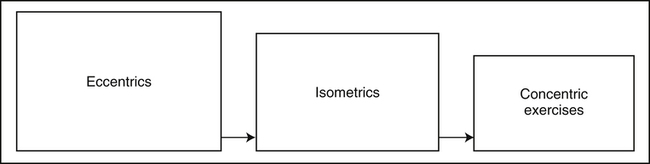
The PTA must consider the context in which each muscle contraction type is used clinically. Fundamentally implementing multiple muscle contraction types during all phases of rehabilitation is well supported.8,35,69 In comparing muscle contraction types, it is best to view the decision concerning which type to use, when to use it, and in what pathologic conditions it should be used as a progression or continuum rather than a choice of one type over another. Davies19 has described a classic model of exercise progression (Box 4-1) that can be used as a general guide. Certain criteria must be established for the progression from one type of contraction to another.
First, exercise variables and parameters must be understood so that necessary adjustments can be made in a patient’s exercise prescription (Box 4-2).The criteria established for progressing from one exercise mode to another is based on many factors and is patient specific. In general, pain usually dictates the time frame for progression, although swelling also does to a lesser degree. The sequence proceeds from the least intense to more challenging exercises with increased joint forces and metabolic demands.
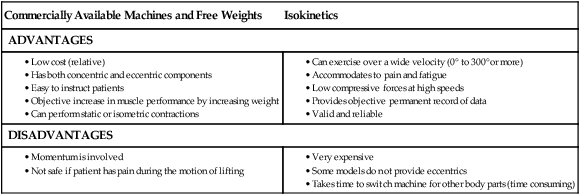
Some of the advantages and disadvantages of concentric and eccentric isotonic exercise and isokinetic exercise equipment are outlined for general comparison in Table 4-2.
Table 4-2
Comparison of Isotonics versus Isokinetics
| Commercially Available Machines and Free Weights | Isokinetics |
| ADVANTAGES | |
MUSCLE RESPONSE TO EXERCISE
Strength training must be individually tailored to meet the goals of recovery. As stated by DeLee and colleagues,21 “Function increases with use; functions we do not use, we lose. The intensity, duration, and frequency of activity are all related to the functional capacity that is developed.”
The stimuli for adaptive changes in skeletal muscle are described as frequency, intensity, and duration.12 Human skeletal muscle responds and adapts to these stimuli and is characterized by the nature, rate, magnitude, and duration of the stimulus.8 In a clinical situation, the stimulus provided to human muscle is the conditioning or training program. These programs are based on certain principles that lead to the necessary adaptive changes, which in turn affect function. The principles of overload, specificity, and reversibility25 as well as progression and transfer of training6 provide the foundation for the strength training programs used in physical therapy and are as follows.
The overload principle6 is the guiding principle of exercise prescription. If muscle performance is to improve, a load that exceeds the metabolic capacity of the muscle must be applied. A muscle must be challenged to perform at a level greater than that to which it is accustomed.
The specific adaptations to imposed demands25 (SAID) principle in part defines specific adaptations and alterations in response to highly specific demands. After injury, muscle reeducation helps the patient adapt and prepare for return to function.
Specificity6 is the training of a patient in a specific manner to produce a specific adaptation or training outcome.
The progression principle6 dictates that the intensity of program must become progressively greater in order to continue to make gains.
The transfer of training6 principle describes the carryover of training effects from one variation of exercise or task to another.
The reversibility principle25 indicates that changes in a body’s systems are transient unless training induced improvements are regularly used for functional activities or a person participates in a maintenance program. This can begin within 1 to 2 weeks after cessation of exercises.
In strength training programs, a desirable and predictable morphologic adaptive change is hypertrophy, which is the compensatory increase in individual muscle fiber size as a result of increases in and synthesis of the contractile proteins actin and myosin.32 Type II muscle fibers increase more than type I fibers do. This can be observed in comparing the body types of long-distance runners with the larger, more muscular physiques of sprinters. The physiques of long-distance runners and most aerobic athletes are thinner, possess less body fat, and have smaller muscles that are more adapted to endurance activities. Highly specific, or absolute strength, programs use a high-tension (heavy loads) and low-volume protocol. This type of training program requires relatively short bouts of progressive overload to stimulate the type II muscle fibers.
Biochemical adaptations of muscle occur in specifically applied strength training programs. After intense strength training, significant increases appear in glycogen, ATP, and creatine phosphate; increased activity and quantity of enzymes involved with anaerobic glycolysis, creatine kinase, and myokinase also are seen.17
Hyperplasia (the development of new muscle fibers) or longitudinal fiber splitting may occur in response to high-intensity strength training programs. Gonyea and colleagues33 reported in animal studies that an increase of 19% of the total number of muscle fibers occurred in cat forelimb muscles after weight lifting. This phenomenon has not been proven in humans. The predominant change in response to high-intensity strength training programs is hypertrophy of existing skeletal muscle fibers. The relative contribution (if any) of hyperplasia or muscle fiber splitting has not been determined.12 Induced hypertrophy in injured or postoperative muscle tissue is important because hypertrophy relates to a potential to generate greater tension.
It is interesting to note that passive stretching of innervated muscle tissue creates tension and also results in fiber hypertrophy. The change in fiber size associated with this stretch-induced hypertrophy results from increased protein turnover.12 This feature has clinical relevance in muscle recovery during immobilization.
DELAYED ONSET MUSCLE SORENESS
The clinical features of exercise-induced muscle soreness are diffuse and general, occurring in the absence of specific, intense injury.57 Acute muscle strain can be differentiated from exercise-induced soreness primarily by the history leading to the injury. With an acute strain, the patient is able to relate a specific event or episode that caused the injury.57
Based on this distinction, the PTA can identify complaints of diffuse muscle soreness resulting from new or unaccustomed exercise.57 However, if the patient can describe a history of local, intense pain after a specific episode, an acute muscle strain must be considered.57
After a specific exercise program, muscle soreness is an anticipated by-product of intense eccentric exercise.29,30,40,52,65,68 The degree and presence of after-exercise muscle soreness appear to be greater with these eccentric programs than with concentric exercise programs.11,40,52,54,65,72
Symptoms of delayed onset muscle soreness (DOMS) include pain, swelling, tenderness, reduced ROM, and stiffness.3,40,52,65 Albert3 reports five general theories concerning the process of DOMS:
The lactic acid and tonic muscle spasms theories do not appear to be related to DOMS.1,2,62,75 Studies49,51 show evidence that the primary cause of muscle soreness after exercise is skeletal muscle damage. Greater tensions produced by eccentric exercise contribute to the initial muscle damage, although isometric and concentric contractions are not absolved of producing latent muscle soreness. In fact, isometric exercise and concentric exercise can produce DOMS even in well-trained athletes.
Conventional methods of treating DOMS are listed in Table 4-3.
Table 4-3
Suggested Treatment Techniques for Delayed Onset Muscle Soreness
| Type | Efficacy |
| Rest | None |
| Nonsteroidal antiinflammatory drugs | Highly successful |
| Steroidal antiinflammatory drugs | Moderately successful |
| Electrical stimulation | Proposed only |
| Exercise | Highly successful |
| Transcutaneous electrical nerve stimulation | Highly successful |
| Stretching | Mixed success |
| Iontophoresis | Not successful |
| Cryotherapy | Not successful |
| Calcium antagonists | Proposed only |
From Albert M: Eccentric muscle training in sports and orthopaedics, New York, 1991, Churchill Livingstone.
Treatment of DOMS remains controversial. One recent study64 found ice, a traditional treatment method, to be ineffectual, whereas other studies7,26 found vibration and compression, nontraditional treatment methods, to be effective.
A recent review67 of the current strategies for treating DOMS revealed the following:
 Pharmacologic aids, nonsteroidal antiinflammatory drugs (NSAIDs): Although there are some inconsistency in findings, NSAIDs such as ibuprofen have the potential to alleviate some of the symptoms of DOMS.
Pharmacologic aids, nonsteroidal antiinflammatory drugs (NSAIDs): Although there are some inconsistency in findings, NSAIDs such as ibuprofen have the potential to alleviate some of the symptoms of DOMS.
 Therapeutic treatments using physical modalities: Treatment using conventional therapies, such as icing, massage, or stretching, also proved inconsistent. Nonconventional treatments such as acupuncture, herbal remedies, and hyperbaric oxygen therapy were found to have limited use. However, the review did indicate that of all the therapies examined, icing the affected area appeared to be the most effective.
Therapeutic treatments using physical modalities: Treatment using conventional therapies, such as icing, massage, or stretching, also proved inconsistent. Nonconventional treatments such as acupuncture, herbal remedies, and hyperbaric oxygen therapy were found to have limited use. However, the review did indicate that of all the therapies examined, icing the affected area appeared to be the most effective.
 Dietary methods using nutritional supplements: Additional supplementation with antioxidants (vitamins C and E) and supplements such as arnica, coenzyme Q and l-carnitine appears to be of little use.
Dietary methods using nutritional supplements: Additional supplementation with antioxidants (vitamins C and E) and supplements such as arnica, coenzyme Q and l-carnitine appears to be of little use.
VELOCITY OF MUSCLE CONTRACTIONS
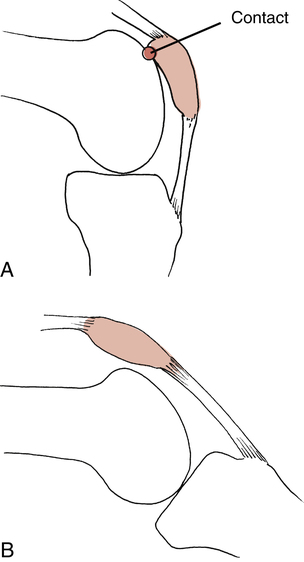
Slower speeds of muscle contraction can produce greater force and tension than the same muscle moving at a higher rate of speed. A slower contracting muscle moving a heavy resistance can produce greater tension than a faster contracting muscle lifting a lighter resistance.54 When slow speeds of full arc resistance exercise are used to generate greater tension and strength, joint compression forces and torque are increased as well. Therefore to minimize the negative or unwanted effects of joint compression (Fig. 4-10), a program of isometric exercise may be more appropriate in some instances.
Functionally, human limbs move at various speeds and with various degrees of motion. Velocity spectrum training allows a patient to train at speeds of motion that more closely approximate normal human limb speeds.10,58,77 For example, a training program using the velocity spectrum concept may include submaximal contractions at slow speeds (60° to 90°/s) for two sets of 8 to 12 repetitions, then contractions at incrementally increasing speeds up to 240° per second or higher for two or three sets of 15 repetitions. This may not be appropriate for athletes, because the functional speeds of movements in athletics far exceed the capability of the isokinetic dynamometer.
In a comparison of isokinetic and isotonic exercise, most isotonic exercise is performed at approximately 60° per second,19 whereas isokinetic exercise can be adjusted specifically to train the affected area at speeds more closely duplicating normal functional speeds of movement. The higher velocity contractions used with isokinetic exercise allow for the following:
 Improved functional speeds of contraction
Improved functional speeds of contraction
 Reduced joint compression forces
Reduced joint compression forces
 Accommodation of patient’s pain (the patient will not undergo more force than he or she can safely produce)
Accommodation of patient’s pain (the patient will not undergo more force than he or she can safely produce)
Using velocity spectrum training with isokinetics allows the progression from multiangle isometrics (0 deg/s) to slow speeds (60 deg/s) for greater tension and torque, to higher speeds (240 deg/s and faster) for functional activities and lower compressive forces.
CLINICALLY RELEVANT EXERCISE PROGRAMS
Although there are many strength training protocols, three broad fundamental strength protocols are used extensively in physical therapy. The DeLorme22 progressive resistance exercise (PRE) protocol is still used widely for strength training programs after injury to the musculoskeletal system. This program uses the classic and well-recognized exercise of three sets of 10 repetitions of resistance. Its protocol states that the patient must establish a maximum weight that can be lifted for 10 repetitions. This is termed the 10 RM (repetitions maximum). To initiate the program the patient performs 10 repetitions at half (50%) of the predetermined 10 RM. The next set of exercise is performed at three fourths (75%) of the 10 RM. Finally, the third set is performed for 10 repetitions at the established 10 RM (100%).
Performing three sets of 10 repetitions at the same resistance is a common clinical practice, however, it is not the DeLorme protocol and is less efficient because it does not overload the muscle in the same manner, nor does it involve built-in warm-up.
The Oxford program78 is the opposite of the DeLorme protocol. Although it begins by establishing the individual’s 10 RM, the second set is performed at three fourths (75%) of the 10 RM and the following set at half (50%) of the established 10 RM. Each set involves 10 repetitions. The method reportedly takes advantage of the muscle’s fatigue during exercise.
The Oxford regimen provides regressive loading and takes into consideration muscle fatigue:
To objectively control the progression or resistance with exercise programs, Knight44 established the daily adjustable progressive resistance exercise technique (DAPRE). Instead of using three sets of 10 repetitions as DeLorme and Oxford did, Knight’s program calls for four sets with variable repetitions. The protocol calls for establishing the patient’s 6 RM instead of 10 RM, with the number 6 based on research by Berger9 as the optimum number of repetitions for developing strength.
As the individual’s strength increases, the number of repetitions in the third set increases, which increases the weight in the fourth set. The hallmark of this program is understanding the guidelines used to adjust the working weight of the third and fourth sets.21 The DAPRE adjusted working weight guide is as follows:
| Set 1 | 10 reps | 50% of 6 RM |
| Set 2 | 6 reps | 75% of 6 RM |
| Set 3 | max reps | 100% of 6 RM |
| Set 4 | max reps | Adjust weight based on # reps performed in set 3 |
| Third Set Number of Repetitions | Fourth Set Change |
| 0 to 2 | Reduce weight 5 to 10 lb |
| 3 to 4 | Reduce weight 5 to 10 lb |
| 5 to 7 | Keep weight the same |
| 8 to 12 | Increase weight 5 to 10 lb |
| 13 or more | Increase weight 10 to 15 lb |
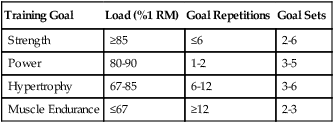
The National Strength and Conditioning Association6 makes the following recommendations:
| Training Goal | Load (%1 RM) | Goal Repetitions | Goal Sets |
| Strength | ≥85 | ≤6 | 2-6 |
| Power | 80-90 | 1-2 | 3-5 |
| Hypertrophy | 67-85 | 6-12 | 3-6 |
| Muscle Endurance | ≤67 | ≥12 | 2-3 |
Other protocols have suggested70 that by initially focusing on muscular hypertrophy, a greater potential for strength would exist. Because the cross-sectional area of muscle would be increased by a program of higher volume, the potential to develop greater amounts of tension is increased by reducing the volume of exercise and increasing the loads used.
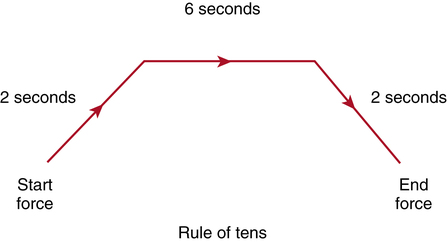
The rule of tens is followed in isometric exercise protocols that are commonly used in rehabilitation.60 This rule states that the patient must perform 10-second contractions for 10 repetitions with a 10-second rest between each repetition.19 The patient is taught to perform isometric contractions by gradually developing tension for 2 seconds, maintaining a maximal contraction for 6 seconds, then gradually decreasing tension for 2 seconds (Fig. 4-11).
While one is performing isometric exercise, an overflow of strength occurs approximately 10° above and below the angle (Fig. 4-12) at which the exercise is occurring.43 Multiple-angle isometrics are taught at 10° increments to achieve strength gains throughout a described ROM.
A circuit training program is a predetermined, organized sequence of exercise. Traditionally, this type of program is used for general body conditioning and total fitness. A general circuit program calls for the performance of one or two exercises for each body part in sequence (Table 4-4). Usually a rest period of 30 seconds to 1 minute is allowed between sets. If resistance exercise equipment is used, circuit weight-training programs also tax the aerobic metabolic pathway to a degree. The movement from one station to another does not allow for maximum recovery and high-intensity loads, but it does provide an adequate stimulus for both aerobic and anaerobic work.
Table 4-4
Sample Circuit Weight Training Program
| Exercise | Repetitions | Sets | Rest |
| Leg press | 10 | 2 | 30 s between each set |
| Leg extension | 10 | 2 | 30 s between each set |
| Leg curl | 10 | 2 | 30 s between each set |
| Bench press | 10 | 2 | 30 s between each set |
| Supine fly | 10 | 2 | 30 s between each set |
| Shoulder press | 10 | 2 | 30 s between each set |
| Lateral pull-down | 10 | 2 | 30 s between each set |
| Bent over row | 10 | 2 | 30 s between each set |
| Bicep curl | 10 | 2 | 30 s between each set |
| Triceps press-down | 10 | 2 | 30 s between each set |
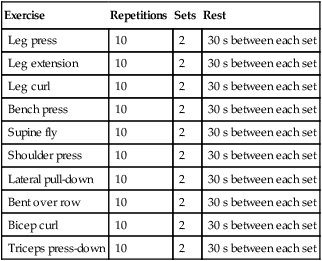
Plyometrics
Plyometric exercises are intense power-generating exercises that are traditionally confined to sport-specific functional training near the end of a rehabilitation program. Plyo comes from the Greek word plythein, meaning to increase, and metric refers to measure. Plyometrics is a system of exercising that uses the stretch reflex to develop muscle contraction speed.76
The principles behind plyometrics are based on the neurophysiologic responses from the Golgi tendon organs (GTOs) and muscle spindles.76 The most rudimentary example of plyometrics is the depth jump (Fig. 4-13). As the foot of the patient contacts the ground (amortization phase), the muscle spindles respond by causing a reflex muscular contraction. Albert3 states, “The greater and more quickly a load is applied to a muscle, the greater the firing frequency of the muscle spindle with a corresponding stronger muscle contraction.” The fundamental goal of plyometric exercise is to minimize the amortization phase of the exercise, which, in this example, is contact with the ground.
All forms of jumping, skipping, and hopping can be used in a plyometric exercise program.76 Upper body exercises, such as throwing and catching a weighted object, are examples of plyometrics. An isotonic supine leg press hop is an example of plyometrics used to develop rapid, eccentric loading with a corresponding rapid, concentric contraction.
Many isotonic strength training programs involve lifting a load from a seated, supine, or standing position. These exercises are meant to isolate and strengthen specific muscle groups throughout a single plane of motion. Plyometrics, on the other hand, focus on weight-bearing functional activities that duplicate high-velocity, multiplane, normal human movement.76 Therefore the PTA must recognize that the value of plyometrics is primarily to prepare the patient to return to function. Naturally not all patients recovering from an orthopedic injury require an intense plyometric exercise program. If, however, the patient desires to return to dynamic sporting activities, or his or her job requires dynamic or ballistic physical labor, then plyometrics are appropriate conditioning to enable one to withstand high levels of both eccentric and concentric loads.
Closed Kinetic Chain Exercise
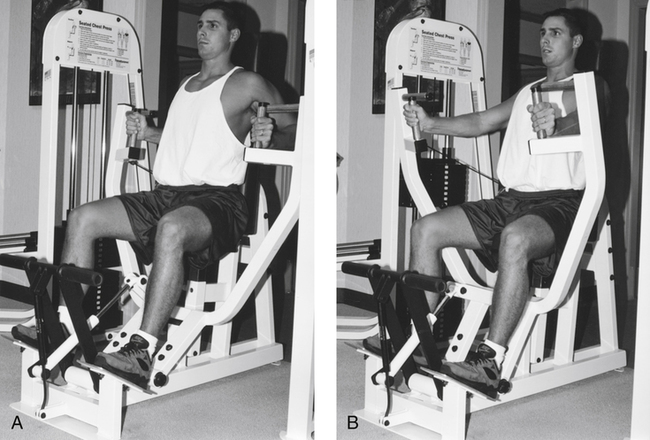
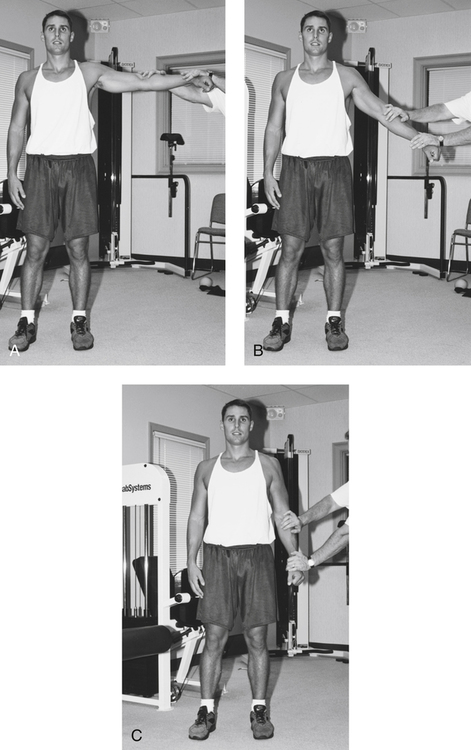
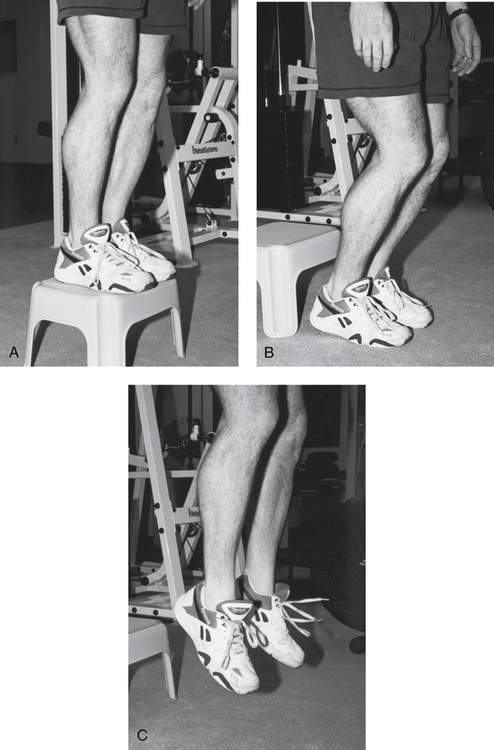
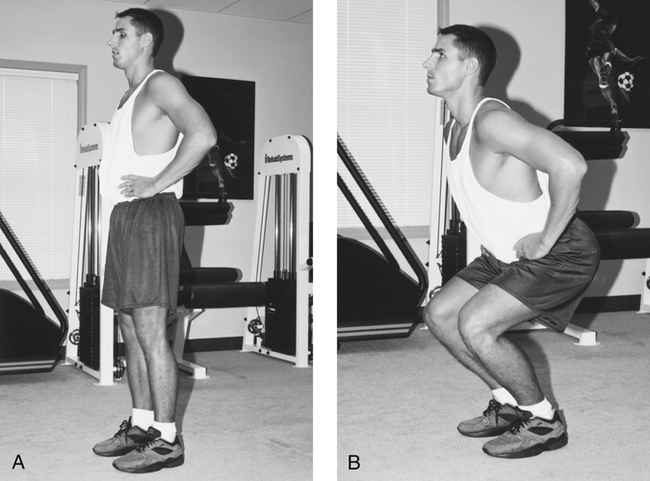
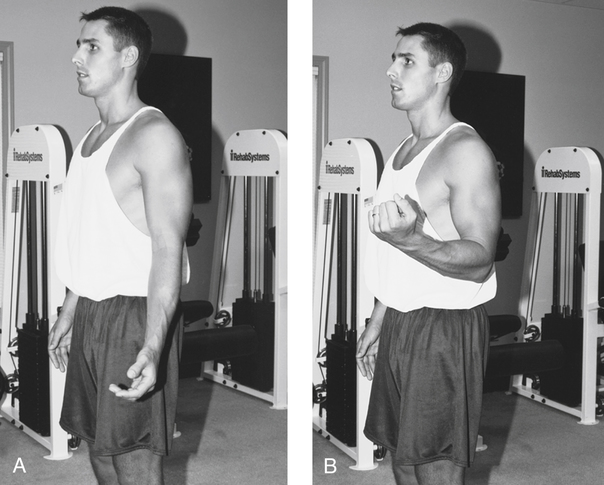
During any exercise, if the distal portion of the exercising segment is weight bearing or fixed, it is called a closed kinetic chain (CKC) exercise. An open kinetic chain (OKC) exercise involves the distal segment moving freely in space, such as a seated knee extension. A CKC is best described as a system of interdependent articulated links. For example, in a weight-bearing leg (Fig. 4-14), as the knee is flexed, the entire chain or link system joining the ankle to the knee and to the hip is affected. In an OKC system, such as the arm (Fig. 4-15), the shoulder and elbow are fixed, whereas the distal wrist segment moves freely in space. Davies20 states, “In a closed kinetic chain, motion at one joint will produce motion at all of the other joints in the system in a predictable manner.”
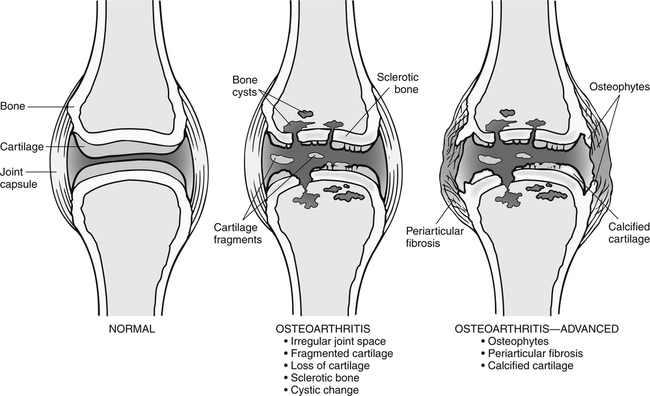
In knee rehabilitation programs,14,56 for example, quadriceps strengthening can be achieved through knee extension exercises (which are open chain), or leg press exercises or squats (which are closed chain). In many cases, patients are introduced to therapeutic exercises by way of submaximal isometric muscle contractions. More intense and demanding exercises are added as pain, strength, and function allow. OKC resistance exercises can be employed to further stimulate growth in strength. In some cases, the PT institutes CKC exercises early in the recovery phase of rehabilitation. For example, CKC exercises are frequently used within the first few weeks after anterior cruciate ligament reconstructive surgery. In addition, select open-chain exercises (those that do not place unwanted forces on the newly repaired tissues) are used. CKC exercises may not be appropriate for some patients with osteoarthritis or other conditions where vertical, compressive loads would exacerbate the condition.
The general rationales for using closed-chain exercises in rehabilitation programs are as follows:
 In theory, CKC exercises are more functional than OKC exercises (this can be refuted)
In theory, CKC exercises are more functional than OKC exercises (this can be refuted)
 Loading of the affected joint(s) produces an increase in kinesthetic awareness
Loading of the affected joint(s) produces an increase in kinesthetic awareness
 Improved neuromuscular coordination is achieved
Improved neuromuscular coordination is achieved
 CKC exercises are nonisolation exercises that produce muscular co-contractions
CKC exercises are nonisolation exercises that produce muscular co-contractions
Caution must be used when prescribing CKC activities during rehabilitation when pain, swelling, dysfunction, or muscle weakness is present.20 Because an articulated joint system is being exercised under these conditions (limited ROM, pain, swelling, etc.), unpredictable compensation may occur in the joint(s) superior and inferior to the affected joint.20 Therefore OKC exercise must be used to isolate and strengthen the weakened area before progressing to CKC exercises.
Periodization of Strength Training Programs
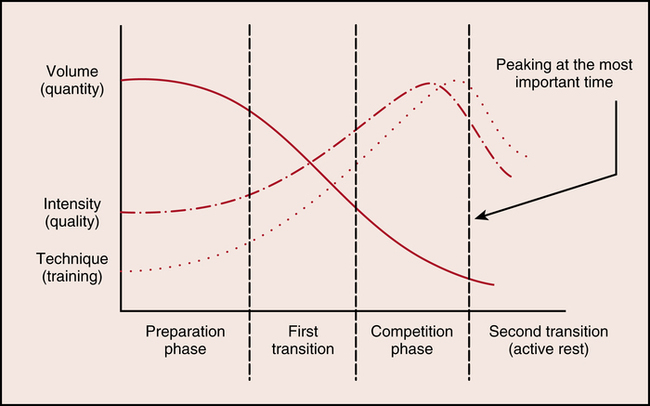
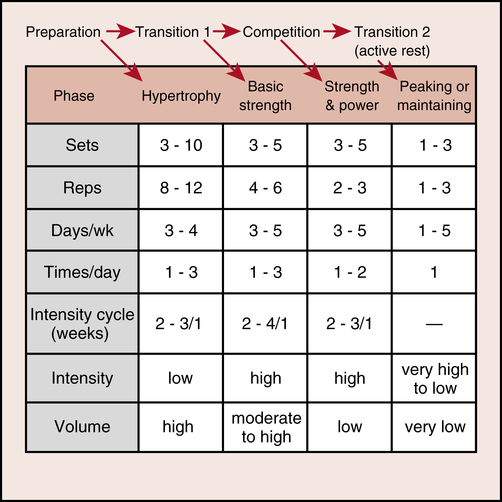
Periodization involves a predictable pattern of exercise volume, intensity, and rest periods that enhance strength-developing capabilities.71 Its main components are cycles, or periods, of strength training. Many fundamental strength programs call for a progressive resistance exercise system without consideration for variations in frequency, intensity, duration, and recovery. The periodization model takes into consideration progressive cycles of various training loads and degrees of intensity during strength programs.71
The fundamental goals and objectives of a classic periodization program are outlined in Figure 4-16. This is only a basic example, which must be modified to meet the specific rehabilitation goals for recovering patients. It can be adapted for many patients who require strength as part of their rehabilitation program.
The traditional athletic model for this modified periodization program is described in Figure 4-17. The strength protocol should be modified to fit the specific needs of each individual.
Strength Training for Older Populations
Strength training programs for the geriatric population include special considerations. In an elderly population, declines in muscle performance, force-generating capabilities, and concomitant muscle mass are well documented.39,47 Therefore strength training programs for the elderly are focused on delaying muscle atrophy, improving function, and increasing force-generating capabilities by stimulating muscle hypertrophy. Note that resistance exercise programs for healthy, older populations show significant improvements in muscle strength, muscle volume (hypertrophy), and other parameters of muscle structure and function.74 Thompson74 reports that studies show that “Given an adequate training stimulus, older men and women show similar gains compared to young individuals after resistive training.” In addition, McCartney and colleagues51 report that “Long term resistance training in older people is feasible and results in increases in dynamic muscle strength, muscle size, and functional capacity.”
A study by Evans24 concludes that “exercise may minimize or reverse the syndrome of physical frailty, which is so prevalent among the most elderly. Because of their low functional status and high incidence of chronic disease, there is no segment of the population that can benefit more from exercise than the elderly.”
Another study by Henwood and Taaffe37 found that cessation of training resulted in only a modest loss of muscle power and strength which was recouped with retraining. This is important, considering that the elderly tend to take extended vacations and have family commitments that require breaks from training.
One must consider multiple morbidities and degenerative joint disease when developing strength training programs for the elderly. Unstable, chronic, and complex medical problems may preclude certain types of strength training programs. For example, in cardiovascular disease, chronic obstructive pulmonary disease, and other conditions, a protocol of general, very low-intensity gross body movement may be more beneficial and safer than isometric or isotonic resistance exercise. In advanced cases of osteoarthritis of the knee and hip, it is prudent to avoid vertical compression loads and full ROM-heavy isotonic exercise. Pain and swelling from osteoarthritic lesions, bone spurs, and osteophytes (Fig. 4-18) can be exacerbated by the tibiofemoral vertical compressive loads involved in leg press or squatting exercises.
In general, studies support the fact that high-intensity resistance training promotes force-generating capabilities in aged muscle42 and that resistance training enhances muscle hypertrophy in elderly people.13,31 In one study,27 a very small population of very old (89- to 90-year-old) men and women showed the beneficial effects of isotonic resistance exercise for this age group. When they trained for 8 weeks, three times per week, the force-generating capacity of the trained muscles increased 174% ± 31%. The muscle mass of this group increased 9% ± 4.5%. In addition, two subjects improved in ambulation, no longer requiring the use of a cane. A hypothesis drawn from these findings suggests that increased force-generating capacity can be correlated with increased function.38
The previously outlined resistance exercise protocols (DeLorme, Oxford, and Knights DAPRE protocols) may be inappropriate for disabled elderly persons. However, modifications of these programs have provided some guidance in developing strength programs for elderly persons.38 Frontera31 states, “The isotonic resistance protocol that produced the greatest increases in force-generation capacity and attenuated atrophy to the greatest extent in older human muscle was three sets of eight repetitions of exercise performed at an intensity of 80% of a muscle’s 1 RM, 3 days a week for 12 weeks.” Studies also support the need to closely monitor heart rate, blood pressure, respirations, and subtle signs of distress during any exercise program for elderly persons.38
As with any resistance program to elicit strength, intensity of effort is the key element in the magnitude of functional or morphologic change in muscle tissue.13,31 In the elderly population, intensity of effort must take into account age, history of cardiovascular or pulmonary disease, history of orthopedic pathologic conditions, present disease states, osteoarthritis, and multiple medical conditions present.
General recommendations for strength training in the older adult are as follows4,50:
Strength Training for Younger Populations
A clear definition of the age range of this special population must be made at the outset to clarify and define the application of resistance exercise and the physiologic adaptation to the precise mode of training. Prepubescent and child are synonymous terms used to describe both boys and girls before the onset of secondary sex characteristics.34 The general range of prepubescence is 11 years for girls and 13 years for boys.34 The terms pubescent and adolescent are synonymous descriptive terms related to girls 12 to 18 years old and for boys 14 to 18 years old.34
In general, these definitions correspond to the classic Tanner stage classification system. Tanner stage I represents preadolescence or ages before the onset of secondary sex characteristics. Tanner stages II through IV describe various levels of development of secondary sex characteristics within adolescence. Tanner stage V is defined as adulthood.34 Other definitions that must be clarified are strength, weight training, resistance training, and weight lifting. The use of the terms strength training, weight training, and resistance training are used to describe submaximal progressive resistance exercise to improve strength, whereas weight lifting describes an attempt to lift maximum weight for a single repetition as a competitive sporting event. Examples are Olympic weight lifting (e.g., clean and jerk, snatch lift) and power lifting (e.g., bench press, squat, dead lift). The appropriate terminology must be specific to denote the precise intent of the mode of exercise.
Physiologic Adaptations
Preadolescent children (Tanner stage I) do not possess circulating androgenic-anabolic hormones (testosterone) that act to stimulate hypertrophy, muscular strength, and secondary sex characteristics. Historically this single irrefutable fact has led many researchers to state, “prepubertal boys do not significantly improve strength or increase muscle mass in a weight training program because of insufficient circulating androgens.”34 However, the complexity of strength acquisition is dependent on many factors, including hypertrophy, increases in muscle cross-sectional area, motor activation, central nervous system stimulation, genetic control, and psychological drive, as well as circulation levels of endogenous hormones.34
Several leading researchers and scientists have identified that preadolescent children can significantly increase strength with appropriately applied resistance exercise protocols.34 However, current evidence strongly suggests that neuromuscular activation, motor coordination, and intrinsic muscular adaptations contribute to preadolescent strength gains.34 In fact, when investigating the effectiveness of nine studies supporting strength gains in children younger than 13 years, researchers found a 71.6% increase in strength versus control group.35
Injury Risk
In nonpathologic conditions, PRE for preadolescent and adolescent children is both safe and effective, providing a few conditions are strictly followed. Also the nature of the specific type of training is directly related to the risk of injury. Namely, unsupervised weight training poses no greater risk for injury when compared with other sports or recreational activities common to this age group.34
Specific sites of injury occurring from nonsupervised weight lifting include the wrist, shoulder, elbows, lumbar spine, and knee. Estimates are more than 17,000 injuries occur annually to adolescents participating in nonsupervised weight lifting or power lifting.34
Other researchers have found no evidence of subclinical or clinical manifestations of musculoskeletal injury in prepubertal boys participating in 20 weeks of resistance training on the basis of bone scans and serum extraction of creatine phosphokinase (a marker of muscle damage).34
Therefore well-supervised, submaximal resistance exercise with use of nonballistic, slow, controlled motions is both effective and safe for preadolescent and adolescent children. The mechanism of physiologic adaptations of resistance exercise for this population is primarily a result of motor unit recruitment, motor control, and neuromuscular activation. Morphologic changes via hypertrophy do not play a role in strength development in preadolescent children.34
Relevant Clinical Applications
The specific therapeutic intervention of strength development in children follows a parallel progression of bone and soft-tissue healing. Each contraction type (isometric, concentric, eccentric) is appropriately used during the defined stages of tissue healing (acute inflammatory, stage I; fibroplasia, stage II; and maturation, stage III), depending on radiographic confirmation of osseous union and stability, as well as soft-tissue healing constraints. In concert with specifically applied flexibility techniques (autogenic and reciprocal inhibition, covered in Chapter 3), strength acquisition in children using the foundation of therapeutic exercise parameters—frequency, intensity, duration, muscle contraction type, degree of resistance, number of repetitions, number sets, length of rest between sets, speed of contraction, and order of exercise—as well as a clearly defined model of exercise progression (see Davies model of exercise progression), the preadolescent can be expected to develop strength primarily by neurogenic activation.
Though the American Academy of Pediatrics (AAP) is against weight lifting, power lifting, and body building, it does approve of strength training programs for children and teens. The training may use free weights, the individual’s own body weight, machines, and/or other resistance devices to attain this goal (Box 4-3).
THERAPEUTIC EXERCISE EQUIPMENT USED IN STRENGTH TRAINING
There are many commercially available isotonic exercise systems.∗ Generally, isotonic exercise machines are fairly adaptable, provide a wide range of resistance (5 to 500 lb for some leg machines), and are mechanically adjustable to accommodate different body types. Individual pieces can be expensive ($3000 or more for a single leg press machine), and a full system may cost $30,000 or more. Various types of muscle contractions can be used with isotonic exercise machines, including concentric and eccentric contractions, isometric static holds, and unilateral or bilateral movements; these exercises can be done using a wide degree of contraction velocities. As discussed, 1 RM testing can be performed on isotonic systems.
Isokinetic exercise systems are used extensively in physical therapy practices for testing, documentation, medicolegal presentations, rehabilitation, and velocity spectrum training. These systems generally are very expensive, with a single multi-joint system costing $40,000 or more.†
Isokinetic systems typically function from 0 degrees per second to 350 to 400 degrees per second. These systems are designed to isolate, test, and rehabilitate single joints. Unfortunately, it is very time consuming to change from one leg to another or from one joint (knee) to another (ankle). The versatility of these systems is presented in Box 4-4.
The impulse inertial exercise apparatus is a system used for submaximal plyometric training. The impulse system provides limited ROM (by design), high-velocity, low-intensity, concentric, and eccentric loading. The application of inertial exercise involves rapid, coordinated, cyclic, and dynamic motions with reduced loads or resistance. The impulse system can be used for upper and lower extremity exercise. Extremely adaptive components with various handles allow for the duplication of sports such as tennis, racquetball, and golf. Clinically, this system is used mainly for neuromuscular coordination and strength in limited degrees of motion. The clinical delivery of inertial exercise is shown in Box 4-5.3
GLOSSARY
Contractile tissue Myofibril—two basic proteins, myosin and actin.
Contraction types Concentric, eccentric, and isometric.
General adaptation syndrome Alarm stage, resistance stage, exhaustion stage, and adaptation.
Noncontractile tissue Epimysium, perimysium, and endomysium.
∗Cybex, Nautilus, Rehab Systems, Body Masters, Universal, and Paramount are all examples of companies that produce lines of exercise equipment for strength training used in both fitness and physical therapy facilities. This equipment is typically available in single- and multi-station units.
∗Some of the more common systems are the Universal, Paramount, Nautilus, Body Masters, and Cybex systems.
†Some common multi-joint systems are the Cybex, Lido, Kin-Com, Biodex, Isotechnologies, and Ariel systems.