Strength
What is muscle strength?
Normal muscle strength is defined as the maximum force a muscle can generate in a specified movement pattern (Knuttgen and Kraemer 1987). Muscle weakness being interpreted as the inability to generate sufficient force to complete a task in a given context. In other words the muscle itself may be able to recruit sufficient force under certain circumstances but not in others when it will present as weak. As well as the context and the task itself, force production in a muscle is influenced by many factors associated with the anatomy and physiology of the muscle and the nervous system controlling it:
• Motor unit (an alpha motor neuron and the muscle fibres supplied by it)
• Number recruited. The greater the number, the greater the force
• Order of recruitment. To produce a smooth coordinated muscle contraction, small motor units are recruited before larger units. This is termed the size principle or Henneman principle
• Size of motor unit. This relates to muscle fibre type, with larger motor units comprised of type IIx (fast glycolytic) fibres and smaller units made up of type I (slow oxidative) fibres
• Frequency of the firing rate. An increased frequency of muscle action potentials to the neuromuscular junction results in summation (S2.6) of the signals.
Generally, greater force is generated with an increased number and size of motor units and at an increased rate of firing.
• Psychological factors such as motivation and mood also affect force production
• Cross-sectional area: The greater the cross-sectional area of the muscle, the greater the number of muscle fibres, motor units and ultimately sarcomeres that can be recruited in parallel and therefore the greater the force generated. Compare the force produced when pulling a car using a single rope with the force generated when 10 ropes are used (in parallel). However, the cross-sectional area includes both contractile and non-contractile tissue, the latter of which does not contribute to force production.
• Neural control: The force production of a given muscle is governed by the task requirements in terms of:
For a learned movement task these factors are integrated into the stored movement plan of the task which then provides feed forward prediction of the force requirements. However, the force production is also modified by ongoing sensory input from the periphery.
• The length tension relationship within the muscle relates to the potential for actin and myosin cross-bridge formation. Working in middle range of the muscle provides the optimum number of available cross-bridges and hence the greatest force production
• The anatomical alignment of muscle fibre within an individual muscle also influences force production (Palastanga et al. 2006)
• The type of muscle work, concentric eccentric or isometric.
Muscle weakness
Muscle weakness may occur as a result of:
• Partial or complete lesion of a peripheral nerve
• Injury to the musculoskeletal system resulting in inflammation, oedema and pain
• Pain which may cause the inhibition of muscle contraction (S3.29)
• A change in role of a muscle imposed by damage to the musculoskeletal or nervous systems may lead to a change in muscle fibre type
• Altered neural control affecting the recruitment of motor units
• Decreased use of the muscle which causes:
• A change in muscle length, becoming lengthened or shortened
• Muscle atrophy, whereby muscle proteins (actin and myosin myofilaments) are lost. Locally there is a loss of sarcomeres in the muscle fibre and globally a reduction in muscle mass (Ryan et al. 2002) and cross-sectional area.
Weakness in neurological conditions
Disorders affecting the peripheral nervous system such as Guillain–Barré syndrome and motor neuron disease often present with weakness as a primary symptom. Damage to the alpha motor neurons interferes with the nerve conduction, which ultimately means that insufficient motor units are recruited and muscle weakness presents. Secondary to this, further weakness may occur as a result of disuse, leading to a loss of sarcomeres and therefore muscle mass (atrophy) (Ryan et al. 2002). Following damage to the peripheral nervous system, motor units can be re-innervated via regeneration of the damaged neuron. However, if the nerve lesion is a long distance from a completely denervated motor unit it may be re-innervated as a result of axonal sprouting from adjacent alpha motor neurons. If this sprouting is heterotypic (not from the same muscle fibre type) the patient may present with dysfunctional incoordinated movement (Lieber 2002). This is a consequence of a disruption in the order of recruitment of motor units (the size principle). The recruitment of small units (type I) followed by the larger units (type IIx) ensures that the force of contraction is built up slowly and smoothly. However, if sprouting occurs from a neuron innervating a type I motor unit to re-innervate a type IIx motor unit the outcome will be large increases in force production too early in the sequence of recruitment and hence an incoordinated movement.
In disorders of the central nervous system (CNS) such as cerebrovascular accident (CVA), Parkinson’s disease and multiple sclerosis, the mechanism underlying muscle weakness is a consequence of damage to higher centres or the pathways involved in motor control. This results in altered signalling down the descending tracts to the alpha motor neuron pool in the spinal cord, the outcome of which is a dysfunction in the timing or pattern of motor unit recruitment or the number of units being recruited. However, ultimately these factors may lead to insufficient or inappropriate recruitment of motor units in a given context and consequently insufficient force to overcome the resistance of the task, or weakness (paresis). Over time, the reduced force production will also be contributed to by a loss of sarcomeres and therefore muscle mass (atrophy) as a consequence of disuse (Ryan et al. 2002). This secondary onset muscle weakness is a common symptom in neurologically impaired patients and may present in any circumstance which leads to movement dysfunction and disuse, e.g. motor impairments but also sensory impairment (S3.23) and cognitive/perceptual deficits (S3.33).
In CNS lesions, muscle weakness is evident in association with both hypotonia (reduced muscle tone) and hypertonia (increased muscle tone; S3.21). The relationship between these concepts is complex but it appears likely that both altered tone states are contributory factors that negatively influence force production (weakness). The pathophysiology which defines alterations in muscle tone also leads to a dysfunction in the timing or pattern of motor unit recruitment or the number of units able to be recruited. Therefore, muscle weakness during movement may be apparent. In terms of assessment a comparison of the conceptual definitions of tone and weakness gives the therapist a simplified tool by which to differentiate. Muscle tone is defined as the resistance to passive movement, representing the background level of tension or stiffness in a muscle (Moore and Kowalske 2000). Therefore it should be assessed in a muscle at rest. Muscle weakness on the other hand is defined as the inability to generate sufficient force to overcome the resistance of a task and therefore by definition should be assessed during movement activities.
Why do I need to assess muscle strength?
Normal muscle strength is required to function in our activities of daily living. Any weakness may lead to ineffective unsuccessful movement with the potential for creating excessive stresses on soft tissue structures which may lead to pain and movement avoidance. By assessing general and/or individual muscle strength, the therapist will be able to focus a strengthening regime to assist the patient in achieving their full potential. However, while focusing upon specific weakened muscles it is also vital to simultaneously re-educate and integrate the strengthened muscles back into functional activities.
In CVA, muscle weakness has been shown to be the major contributor to limits in functional ability (Chae et al. 2002; Kim and Eng 2003; Mercier and Bourbonnais 2004). However, it is still widely believed that resistance strength training increases muscle tone and is therefore avoided in patients with central nervous disorders. However, this belief appears unwarranted when considering the evidence to the contrary. Several studies have now reported significant gains in strength without detrimental increases in spasticity in CVA (Sharp and Brouwer 1997; Brown and Kautz 1998; Badics et al. 2002; Sterr and Freivogel 2004; Morris et al. 2004; Ada et al. 2006) and multiple sclerosis (Taylor et al. 2006). The research also indicates that the increases in strength through resistance training are transferred into some functional improvement in CVA (Yang et al. 2006; Ada et al. 2006; Bale and Strand 2008) and multiple sclerosis (Taylor et al. 2006).
How do I assess muscle strength?
Strength measures utilized by the therapist may involve isometric (static), isokinetic/isotonic (dynamic – concentric and eccentric) testing, functional activities or lifting weights (1 repetition maximum). The choice of assessment will be dependent upon the test requirements.
Muscle cross-sectional area (limb girth measurement)
As a muscle’s size is proportional to its strength, a simple measure of muscle bulk gives the therapist a clue about muscle strength in terms of hypertrophy or atrophy when compared with the other side of the body. However, hand dominance will need to be taken into account. The limitation of this measure is that it also includes the non-contractile elements of the muscle and does not tell the therapist about the level of force production.
Patient
The measurement should be carried out on a relaxed muscle and therefore the patient should be well supported in either supine or long sitting during the assessment.
Therapist
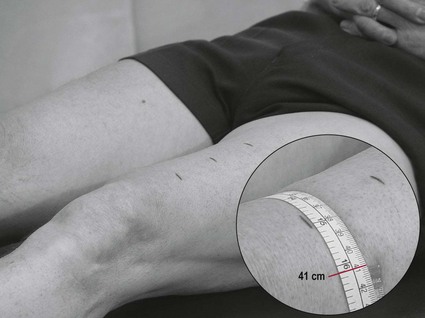
1. Mark on the limb 2 or 3 points of reference (Table 30.1, Fig. 30.1) depending upon the size of the limb. A standardized system of taking the measurements will improve repeatability
Table 30.1
Standardized markers for measuring limb girth
| Limb girth measurement | Markers for measurement |
| Limb girth – thigh | 15 cm, 20 cm, 25 cm superior to the tibial tuberosity (Fig. 30.1) |
| Limb girth – calf | 5 cm, 10 cm, 15 cm inferiorly to the tibial tuberosity |
| Limb girth – upper limb (upper arm) | 4 cm and 8 cm superiorly from the olecranon process |
| Limb girth – upper limb (forearm) | 4 cm inferiorly from the olecranon process |
2. Use a tape measure to measure the circumference of the limb at each mark
3. Repeat the measurement 3 times for each mark
Manual muscle strength testing
The most commonly used methods are:
• Isometric resisted movement: Used for differential diagnosis to implicate contractile tissue or to test nerve integrity (myotomes).
• Oxford grading (Dyck et al. 2005). This assessment utilizes a measurement scale from 0–5 (Medical Research Council 1976).
1 – Flicker or trace of contraction
2 – Full active range of movement with gravity eliminated
3 – Full active range of movement against gravity
4 – Full active range of movement against gravity and against minimal resistance
5 – Full range of movement against gravity and against maximal resistance (normal strength).
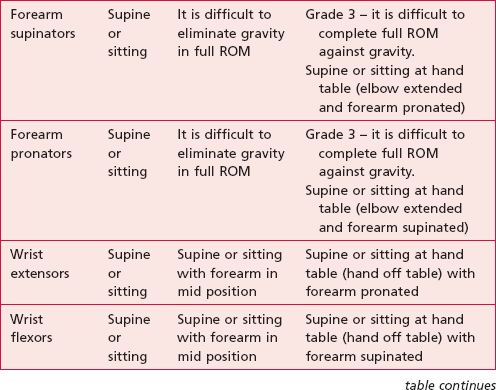
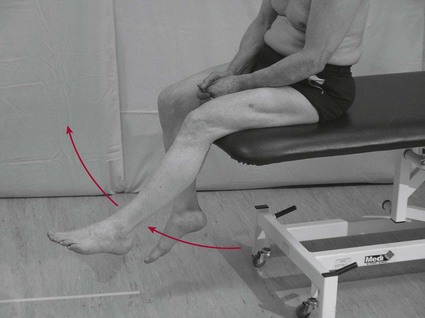
Oxford grading (MRC scale)
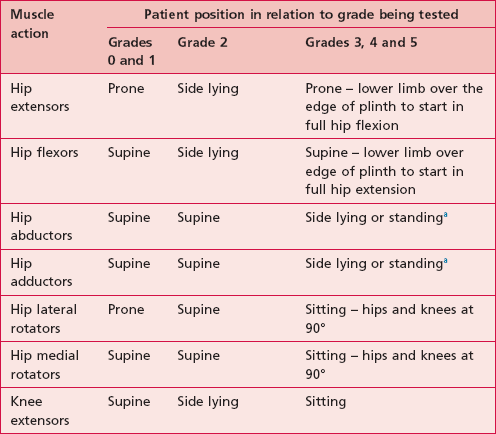
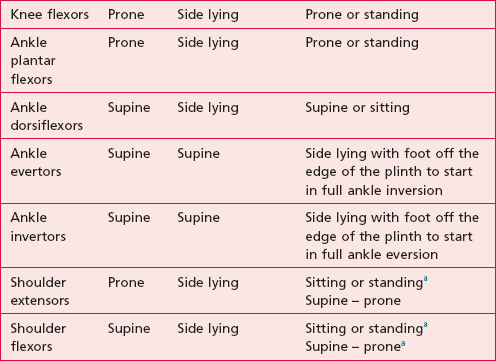
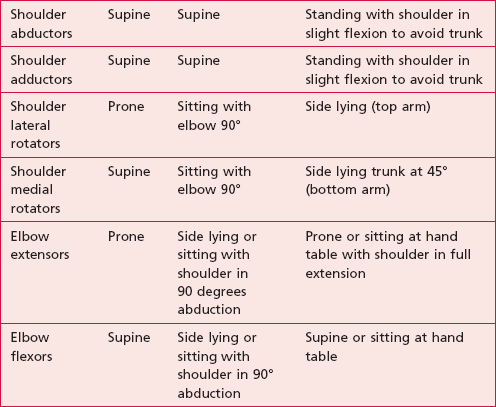
Patient
As the grades are defined in relation to the full active range of movement (ROM) and in relation to gravity, the position of the patient may need to be modified when testing each joint, each direction of movement and each grade. Table 30.2 provides a guide to the patient’s position necessary for each test to be completed. The patient needs to be sufficiently undressed to allow the therapist to observe and/or palpate the muscle being assessed. Palpating through clothes is not good practice.
Testing for grade 0 and 1
1. Ask the patient to attempt to either contract the muscle in a static position or attempt to move the limb in an appropriate direction related to the muscles function. The use of words such as ‘tighten or squeeze’ should inform the patient of what is required.
2. Observe and palpate the muscle in question (Fig. 30.2).
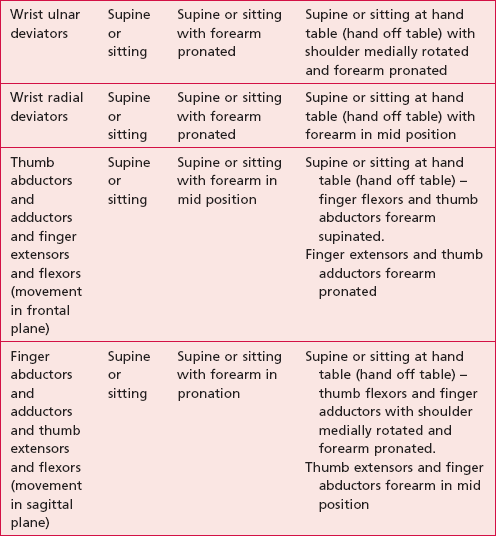
Testing for grade 2
1. The therapist needs to consider a suitable position so that the movement is:
a. Through the full ROM. For example, full extension of the hip starts at full hip flexion and ends at full hip extension
b. Not being assisted or resisted by gravity
c. Isolated. This may require the therapist to support the weight of the limb being tested, e.g. when assessing the hip abductors.
2. Ask the patient to ‘Move the body part from start position to finish position’ (Fig. 30.3).
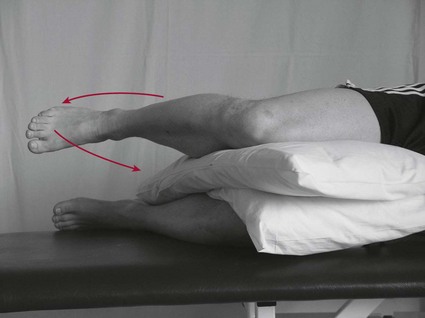
Testing for grade 3
1. The therapist needs to consider a suitable position so that the movement is:
b. Being resisted by gravity. With some muscle actions, it is not possible to carry out the full ROM against gravity in one movement. In these cases, a second posture should be sought in order to test the action in two halves. For example, to test shoulder flexion – supine with upper limb off the edge of the plinth to test full extension to neutral and in standing to test neutral to full flexion.
2. Ask the patient to ‘Move the body part from start position to finish position’ (Fig. 30.4).
Testing for grade 4
1. The therapist needs to consider a suitable position so that the movement is:
c. Additional ‘minimal resistance’ is provided throughout the ROM by the therapist. The therapist needs to consider how much resistance to use relating to ‘minimal’ and should modify the resistance applied according to the size of muscle being tested and the patient’s characteristics (e.g. age and gender).
2. Note: In clinical practice, the application of an additional resistance through the ROM is often considered to negate the need for the action to be against gravity.
3. Ask the patient to ‘Move the body part from start position to finish position’.
4. Apply minimal resistance throughout the full ROM (Fig. 30.5).
Testing for grade 5
1. The therapist needs to consider a suitable position so that the movement is:
b. Being resisted by gravity. Note the point made in grade 4 section
c. Additional ‘maximal resistance’ is provided throughout the ROM by the therapist. Grade 5 represents normal strength, however maximal resistance will need to be adapted according to which muscle action is being tested and other patient specific factors.
2. Ask the patient to ‘Move the body part from the start position to the finish position’.
3. Apply maximal resistance throughout the full ROM (Fig. 30.5).
Recording
The grade awarded is usually recorded in relation to the total possible score. For example grade 4 strength is notated as 4/5. A simple table (Table 30.3) or a list of results allowing comparison of left and right sides of the body is acceptable and gives a clear and easily understandable record of the findings.
Analysis
A comparison of scores for left and right sides of the body is the first step of analysis. However, if the impairment of strength is suspected to be bilateral, as in the case of Guillain–Barré syndrome and motor neuron disease, this analysis will be invalid. In this situation, a comparison can only be made against the therapist’s expectation of what ‘normal strength’ would be for that individual person. Any score below 5/5 is indicative of muscle weakness and should be targeted as requiring a strengthening programme.
In the above example, the left shoulder muscles are generally weaker than the right in the directions identified.
Outcome measure
Research
The gold standard for assessing muscle strength is isokinetic dynamometry, which measures isokinetic muscle strength (e.g. Cybex (Medway, MA) and KinCom (IsoKinetic International, Harrison, TN). However, the clinical usefulness of such machines is limited by their cost and size. The hand held dynamometer is more realistic for use in a clinical setting but only provides an objective measure for isometric muscle strength.
References and Further Reading
Ada, L, Dorsch, S, Canning, CG. Strengthening interventions increase strength and improve activity after CVA: a systematic review. Australian Journal of Physiotherapy. 2006; 52:241–248.
Brown, DA, Kautz, SA. Increased workload enhances force output during pedaling exercise in persons with post-CVA hemiplegia. Stroke. 1998; 29:598–606.
Badics, E, Wittmann, A, Rupp, M. Systematic muscle building exercises in the rehabilitation of CVA patients. NeuroRehabilitation. 2002; 17:211–214.
Bale, M, Strand, LI. Does functional strength training of the leg in subacute stroke improve physical performance? A pilot randomized controlled trial. Clinical Rehabilitation. 2008; 22(10–11):911–921.
Chae, J, Yang, G, Park, BK, et al. Muscle weakness and cocontraction in upper limb hemiparesis: relationship to motor impairment and physical disability. Neurorehabilitation and Neural Repair. 2002; 16:241–248.
Dyck, PJ, Boes, CJ, Mulder, D, et al. History of standard scoring notation and summation of neuromuscular signs: a current survey and recommendation. Journal of the Peripheral Nervous System. 2005; 10:158–173.
Hara, Y, Akaboshi, K, Masakado, Y, et al. Physiologic decrease of single thenar motor units in the F-response in CVA patients. Archives of Physical Medicine and Rehabilitation. 2000; 81:418–423.
Kim, CM, Eng, JJ. The relationship of lower-extremity muscle torque to locomotor performance in people with CVA. Physical Therapy. 2003; 83:49–57.
Knuttgen, H, Kraemer, W. Terminology and measurement in exercise performance. Journal of Applied Sport Science and Research. 1987; 1:1–10.
Kraemer, WJ, Adams, K, Cafarelli, E, et al. American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Medicine and Science in Sports and Exercise. 2002; 34:364–380.
Lieber, RL. Skeletal muscle structure, function and plasticity: the physiological basis of rehabilitation,, ed 2. Philadelphia: Lippincott Williams and Wilkins; 2002.
Medical Research Council (MRC). Aids to the investigation of the peripheral nervous system. London: Her Majesty’s Stationery Office; 1976.
Mercier, C, Bourbonnais, D. Relative shoulder flexor and handgrip strength is related to upper limb function after CVA. Clinical Rehabilitation. 2004; 18:215–221.
Moore, DP, Kowalske, KJ. Neuromuscular rehabilitation and electrodiagnosis of myopathy. Archives of Physical Medicine and Rehabi1itation. 2000; 81:S32–S35.
Morris, SL, Dodd, KJ, Morris, ME. Outcomes of progressive resistance strength training following CVA: a systematic review. Clinical Rehabilitation. 2004; 18:27–39.
Palastanga, N, Field, D, Soames, R. Anatomy and human movement: structure and function,, ed 5. Edinburgh: Butterworth Heinemann/Elsevier; 2006.
Ryan, AS, Dobrovolny, CL, Smith, GV, et al. Hemiparetic muscle atrophy and increased intramuscular fat in CVA patients. Archives of Physical Medicine and Rehabilitation. 2002; 83:1703–1707.
Sharp, SA, Brouwer, BJ. Isokinetic strength training of the hemiparetic knee: effects on function and spasticity. Archives of Physical Medicine and Rehabilitation. 1997; 78:1231–1236.
Sterr, A, Freivogel, S. Intensive training in chronic upper limb hemiparesis does not increase spasticity or synergies. Neurology. 2004; 63:2176–2177.
Taylor, NF, Dodd, KJ, Prasad, D, et al. Progressive resistance exercise for people with multiple sclerosis. Disability and Rehabilitation. 2006; 2818:1119–1126.
Weiss, A, Suzuki, T, Bean, J, et al. High intensity strength training improves strength and functional performance after CVA. American Journal of Physical Medicine and Rehabilitation. 2000; 794:369–376.
Yang, Y-R, Wang, R-Y, Lin, K-H, et al. Task-oriented progressive resistance strength training improves muscle strength and functional performance in individuals with stroke. Clinical Rehabilitation. 2006; 20:860–870.