61 Stellate Ganglion Block (Cervicothoracic Sympathetic Ganglion Block)
Stellate ganglion blocks can be performed to treat sympathetically maintained pain (reflex sympathetic dystrophy, causalgia, complex regional pain syndrome type I). The stellate ganglion is the fusion of the inferior cervical and first thoracic sympathetic ganglia. Almost all of the sympathetic innervation of the head, neck, and upper extremity travels via pathways through the stellate ganglion. The stellate ganglion is approximately 0.5 to 2.5 cm in size.1 Despite its name, the stellate ganglion is fusiform, triangular, or globular in shape on magnetic resonance scans.2 Stellate ganglion block is used to diagnose and treat chronic pain syndromes of the upper extremity and head and neck.
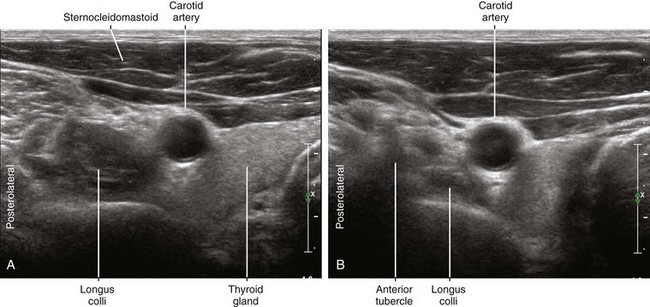
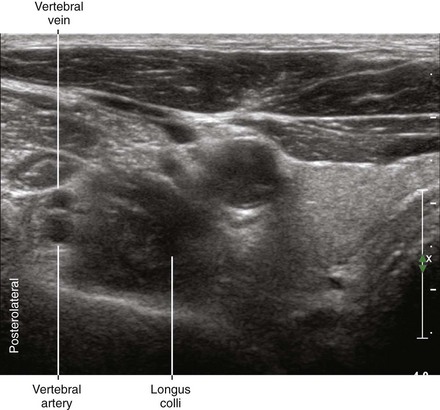
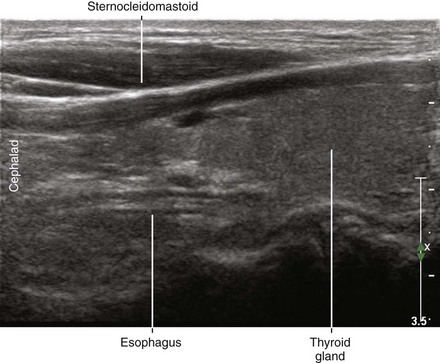
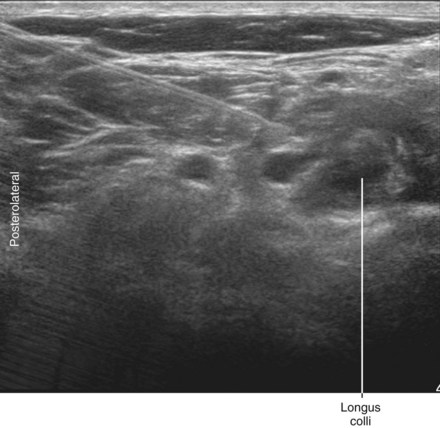
At the level of the first thoracic vertebral level, the stellate ganglion lies lateral and posterior to the lateral edge of the longus colli muscle. As the cervical sympathetic chain travels cephalad, it comes to lie anterior to the longus colli muscle.3,4 This muscle lies over the anterior surface of the cervical transverse processes.
Anatomic Structures to Be Identified for Stellate Ganglion Block
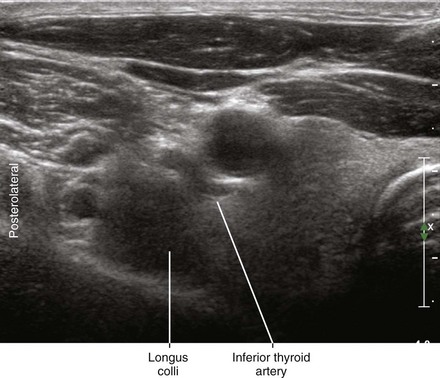
Inferior Thyroid Artery
The inferior thyroid artery has a tortuous course (hence its alternate name, the “serpentine” artery).5 This artery travels over the surface of the longus colli muscle from lateral to medial.
Phrenic Nerve
The phrenic nerve crosses over the anterior surface of the anterior scalene muscle from lateral to medial. On ultrasound scans the phrenic nerve appears as a small (<1 mm in diameter) monofascicular structure.6 The phrenic nerve lies adjacent to the C5 ventral ramus at the level of the cricoid cartilage (C6). Performing stellate block caudal to this level helps avoid the phrenic nerve within the lateral to medial needle path. Similarly, the superficial cervical artery (transverse cervical artery) that also lies over the anterior scalene muscle can be avoided in this fashion.
Approach and Suggested Technique
For the lateral-to-medial in-plane approach the needle is placed through the anterior scalene muscle into the longus colli muscle. This is usually done between C6 and C7 or between C7 and T1. Gentle pressure is held on the injection syringe as the needle is slowly withdrawn until a rim of local anesthetic is seen to distribute around the lateral aspect of the longus colli muscle. There is debate regarding the correct layer for successful stellate block as being over, under, or within the fascia that invests the longus colli muscle.7 Regardless, a rim of local anesthetic that outlines the surface of the longus colli muscle is predictive of block success. Because the site of injection is distant from the stellate ganglion (which lies closer to the level of T1), 5 to 15 mL of local anesthetic is used for the block. The head of the bed is elevated after injection to promote caudal and posterior distribution toward the stellate ganglion.
Postprocedure neurologic examination is performed to rule out somatic brachial plexus block. A temperature increase of the ipsilateral upper extremity and Horner’s syndrome is expected with successful block. The sympathetic efferents to the arm are primarily found in the C8 and T1 roots.8 It is therefore important that local anesthetic distribute to the sympathetic chain at or below those levels. Bilateral stellate ganglion blocks should be avoided or at least temporally staggered because of the risk of bilateral pneumothorax, cardiac accelerator nerve fiber block, recurrent laryngeal nerve block, and phrenic nerve block.
Key Points
| Stellate Ganglion Block | The Essentials |
|---|---|
| Anatomy | The CSG lies on the posterolateral aspect of LC at C7. |
| The STG lies near the head of the first rib. | |
| The ITA, VA, ESO, PN, can lie in the needle path. | |
| Positioning | Supine with arms at side, blue foam headrest |
| Operator | Standing at the side of the patient |
| Display | Across the table |
| Transducer | High-frequency linear, 38- to 50-mm footprint |
| Initial depth setting | 35 to 50 mm |
| Needle | 21 gauge, 70 mm in length |
| Anatomic location | Begin by imaging the C6 and C7 transverse processes. |
| Perform the block between C6 and C7 or between C7 and T1. | |
| Approach | In-plane from lateral to medial |
| Aim the needle through the AS into the LC. | |
| Slowly inject as the needle is withdrawn. | |
| Sonographic assessment | The injection should rim over the lateral surface of the LC. |
| Anatomic variation | Common (a distinct STG is not present in 20%) |
1 Erickson SJ, Hogan QH. CT-guided injection of the stellate ganglion: description of technique and efficacy of sympathetic blockade. Radiology. 1993;188(3):707–709.
2 Hogan QH, Erickson SJ. MR imaging of the stellate ganglion: normal appearance. AJR Am J Roentgenol. 1992;158(3):655–659.
3 Ebraheim NA, Lu J, Yang H, et al. Vulnerability of the sympathetic trunk during the anterior approach to the lower cervical spine. Spine. 2000;25(13):1603–1606.
4 Civelek E, Karasu A, Cansever T, et al. Surgical anatomy of the cervical sympathetic trunk during anterolateral approach to cervical spine. Eur Spine J. 2008;17(8):991–995.
5 Narouze S. Beware of the “serpentine” inferior thyroid artery while performing stellate ganglion block. Anesth Analg. 2009;109(1):289–290.
6 Kessler J, Schafhalter-Zoppoth I, Gray AT. An ultrasound study of the phrenic nerve in the posterior cervical triangle: implications for the interscalene brachial plexus block. Reg Anesth Pain Med. 2008;33:545–550.
7 Gofeld M, Bhatia A, Abbas S, et al. Development and validation of a new technique for ultrasound-guided stellate ganglion block. Reg Anesth Pain Med. 2009;34(5):475–479.
8 Hogan QH, Erickson SJ, Haddox JD, et al. The spread of solutions during stellate ganglion block. Reg Anesth. 1992;17(2):78–83.