Sprains and Strains
General Treatment
1. First-aid treatment for sprain and strain injuries is summarized by the acronym RISE (rehabilitation, ice, support, and elevation.)
a. Rehabilitation: Rehabilitation replaces the outdated advice to put the joint at rest. Instead, early mobility, light touch weight bearing, and range of motion activities promote earlier recovery from sprain.
b. Ice: Ice reduces swelling and eases pain. Make sure to provide a layer of cloth between skin and ice to prevent freezing the underlying tissue. For ice or cold therapy to be effective, apply ice early and for up to 20 minutes at least three or four times a day, for the first 72 hours after injury.
c. Support: More helpful than compression is support of the injured tissues, ideally with an air splint type device or with taping (see Chapter 23 for taping information).
d. Elevation: Elevate the injured joint above the level of the heart as often as possible to reduce swelling.
2. Administer an oral nonsteroidal antiinflammatory drug (NSAID), such as ibuprofen 600 mg q6h, to reduce pain and inflammation.
Disorders
Signs and Symptoms
1. Ankle sprain: The most commonly injured ligaments (anterior and posterior talofibular and calcaneofibular ligaments) are on the lateral aspect of the joint (Fig. 21-1).
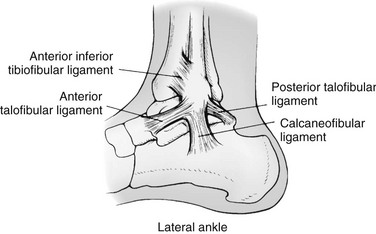
FIGURE 21-1 Ligament complexes of the ankle.
2. A syndesmosis injury, or “high ankle sprain,” may occur. Tenderness occurs over the anterior tibiofibular and deltoid ligaments. A positive squeeze test, in which pain radiates through the interosseous membrane with compression of the tibia against the fibula, exists. The fibula may be fractured. Symptoms of proximal fibular fracture include associated proximal fibular tenderness or crepitus.
3. A midfoot sprain can occur with associated tarsometatarsal fracture (Lisfranc’s injury). These injuries present as severe pain and marked swelling along the entire midfoot. This can be a problematic injury associated with compartment syndrome of the foot. Keep the patient non–weight bearing with elevation. Use ice if available. Evacuate the patient for definitive orthopedic reduction.
4. Differentiate ankle sprain from fracture (see Chapter 18).
Ruptured Achilles Tendon
Signs and Symptoms
1. An audible “pop,” with a sensation similar to being kicked in the calf
2. Difficulty plantar flexing the foot, although the plantaris muscle can plantar flex the foot as well. The only reliable sign is Thompson’s test
3. Thompson’s test: The patient is placed in a prone position with the foot hanging free. If there is no plantar flexion of the foot as the calf is squeezed, Thompson’s test is positive.
4. Swelling of the distal calf
5. Sometimes, a palpable defect in the tendon 2 to 6 cm ( to
to  inches) proximal to its insertion can be appreciated within the first hour. After that, if there is significant bleeding, the defect can be more difficult to detect
inches) proximal to its insertion can be appreciated within the first hour. After that, if there is significant bleeding, the defect can be more difficult to detect
Treatment
1. If the tendon is strained and not completely torn or ruptured, follow RISE.
2. Have the patient gently stretch the tendon to keep it flexible, then gradually put weight on the foot, with walking as pain allows.
3. In-shoe, firm heel lifts should be used in both shoes. The goal of using a heel lift is to reduce the strain on the Achilles tendon while allowing one to remain mobile, to permit the tendon to be less stretched and relaxed while healing slowly occurs. Because tendons have no blood supply, this healing typically requires weeks or months, and the tendon can easily be reinjured if it is stressed during this time.
4. If the Achilles tendon is ruptured, walking will be difficult. Splint the ankle in slight plantar flexion and evacuate the patient. Surgery is generally necessary to repair the torn tendon.
Patellofemoral Syndrome
Treatment
1. Apply ice, and allow the patient to rest.
2. Administer an NSAID, such as ibuprofen 600 mg q6h.
3. Place a wide supporting elastic band around the leg below the patella to help prevent pain during walking. This should not be overly tight.
4. Use two trekking or ski poles while hiking to help absorb impact and reduce pain.
5. Prevention is important to prevent future recurrences. The best prevention is aggressive lower extremity balancing (hamstring flexibility, hip abductor strengthening, and orthotics if pronated feet are present).
Iliotibial Band Syndrome
This is irritation of the connective tissue along the outside of the thigh.
Ligament Sprain
Signs and Symptoms
1. An audible “pop” at the time of the injury is common with ACL injuries and less common with MCL and LCL injuries.
2. Immediate pain that soon becomes a dull ache
3. Often marked swelling with joint effusion
4. For a severe sprain, instability of the knee while walking or turning
5. Severity based on percentage of ligament injured
a. First-degree sprain: pain but no instability when the knee is stressed
b. Second-degree sprain: pain and slight instability when the knee is stressed
c. Third-degree sprain: significant instability, often less pain when the knee is stressed than with lower-grade sprains. A third-degree sprain is a completely torn ligament.
Treatment
1. For first-degree sprain, use RISE. Walking can usually be resumed with little or no additional support.
2. For second-degree sprain, use RISE. Ensure that the patient wears a knee immobilizer while walking. This device should be cylindrical and extend from midthigh to midcalf (see Chapter 18).
3. For third-degree sprain, use RISE. Do not allow the patient to walk without a knee immobilizer. Use improvised crutches or ski poles for additional support. If, after applying a knee immobilizer, the patient’s knee still feels unstable and is prone to buckling with weight, evacuate the patient without allowing walking.
Torn Meniscus (Cartilage)
1. Significant axial compression (big ski jump landing flat on skis)
2. Squatting injuries (lifting up a heavy object from a squatting position or rotating/twisting while in the squatted position, especially in someone who may have an underlying ACL deficiency
Treatment
1. Apply ice, and allow the patient to rest.
2. Administer an oral NSAID such as ibuprofen 600 mg q6h.
3. If the knee feels unstable, apply a complete immobilizer.
4. If the patient has a locked knee (commonly associated with a “bucket-handle” meniscal tear), attempt to unlock it by positioning the patient with the leg hanging over the edge of a table or flat surface with the knee in approximately 90 degrees of flexion. After a period of relaxation, apply gentle longitudinal traction to the knee with internal and external rotation. Parenteral or oral pain medication and a muscle relaxant may facilitate the reduction. If the injury does not reduce easily, immobilize the patient and transport.
Thumb Sprain
The thumb (ulnar collateral ligament) is frequently injured when placed in extreme extension or abduction, such as occurs when it is caught in the strap of a ski pole when falling. Taping can prevent reproducing the mechanism of injury, particularly when grasping an object (see Chapter 23).






