119 Splenomegaly
Salient features
History
• Night sweats, low-grade fever: from hypermetabolic state caused by overproduction of white blood cells in chronic myeloid leukaemia
• Abdominal fullness: from splenomegaly
• Bleeding, bone pain: bone marrow infiltration in myeloproliferative disorders
• History of residence in endemic areas of malaria, kala-azar
• Family history of Gaucher’s disease
• History of fever (infectious mononucleosis, infective endocarditis)
• Blurred vision, respiratory distress, priapism (from leukostasis in chronic myeloid leukaemia)
• Occasionally transverse myelitis (from myelopoiesis in epidural space).
Examination
• Massive spleen. There may be associated anaemia.
• Start low while examining for the spleen and be gentle during palpation. Even if you are certain it is the spleen, you must go through the motions of ruling out a palpable kidney: do a bimanual palpation and check for ballottement; feel for the splenic notch; auscultate for splenic rub.
• Look for enlarged lymph nodes and anaemia.
• Remember that the spleen must be at least two or three times its usual size before it can be felt.
• Remember that the spleen normally does not extend beyond the anterior axillary line and lies along the 9th, 10th and 11th ribs. The spleen percussion sign is a useful diagnostic technique (Ann Intern Med 1967;67:1265).
Advanced-level questions
In which conditions can a moderately enlarged spleen (two to four finger-breadths or 4–8 cm) be felt?
In which common conditions would the spleen be just palpable?
• Lymphoproliferative disorders
• Portal hypertension secondary to cirrhosis
• Glandular fever (infectious mononucleosis)
• Sarcoid, rheumatoid arthritis, collagen disease, idiopathic thrombocytopenia, congenital spherocytosis and polycythaemia rubra vera (95% of those with polycythaemia vera have a mutation affecting the JAK2 signalling molecule)
What do you understand about the terms myeloid metaplasia and extramedullary hematopoiesis?
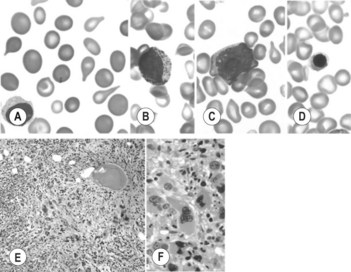
Myeloid metaplasia and extramedullary hematopoiesis are used interchangeably. They describe the process of ectopic haematopoietic activity that may occur in any organ system but predominantly affects the liver and spleen. It may or may not be associated with bone marrow fibrosis (myelofibrosis). ‘Myelofibrosis with myeloid metaplasia’ is usually used to describe idiopathic myelofibrosis or agnogenic myeloid metaplasia (N Engl J Med 2000;342:1255–65). Myelofibrosis is characterized by splemomegaly, teardrop poiklocytosis in peripheral smear, leukoerythroblastic blood picture and giant abnormal platelets, hypercellular marrow with reticulin or collagen fibrosis (Fig. 119.2).
What do you understand by the term chronic myeloid disorders?
Chronic myeloid disorders include:
• chronic myeloid leukaemia: characterized by elevated white blood cell count, marked left-shift to myeloid series, but a low percentage of promyelocytes and blasts, presence of Philadelphia chromosome or bcr/abl
• myelodysplastic syndromes: characterized by cytopenias with a hypercellular bone marrow, morphologic abnormalities in two or more hematopoietic cell lines
• atypical chronic myeloid disorder
• chronic myeloproliferative disease: polycythaemia vera, essential thrombocythaemia, myelofibrosis with myeloid metaplasia: