CHAPTER 13 Splenectomy
Step 1. Surgical anatomy
♦ The spleen is mobilized by dividing the splenic attachments and ligating the vascular hilum without injury to the nearby stomach or pancreatic tail.
♦ Peritoneal attachments and splenic ligaments can be divided using electrocautery or ultrasonic cutting devices.
♦ The vascular supply requires adequate ligation for proper hemostasis. This can be achieved using energy devices as well as vessel sealing systems, clips, and laparoscopic staplers.
Step 2. Preoperative considerations
Patient preparation
♦ It is important to consider spleen size when preparing a patient for laparoscopic splenectomy. This will determine the port placement as well as the potential need for a hand-assist port.
♦ Any evidence of an accessory spleen seen on preoperative imaging should be noted, particularly for hematologic indications for splenectomy.
♦ Patients with idiopathic thrombocytopenic purpura (ITP) and a preoperative platelet count less than 20,000 should be prepared for intraoperative platelet transfusion. Steroids and intravenous immunoglobulin can be given prior to surgery to temporarily elevate the platelet count.
♦ While the risk for overwhelming postsplenectomy infections (OPSI) is small, it is advised that vaccinations be given 2 to 3 weeks prior to an elective operation. These should include vaccinations for encapsulated organisms: Streptococcus Pneumoniae, Haemophilus Influenza B, and Neisseria Meningitidis.
♦ Hand assistance may be helpful in cases of splenomegaly or when removal of an intact specimen is needed.
Equipment and instrumentation
♦ Standard laparoscopic instrumentation is required, including abdominal access devices (e.g., Veress needle or visualization ports), 12-mm and 5-mm ports; 30-degree endoscope; standard laparoscopic instruments including scissors, graspers, and electrocautery; suction-irrigator; and large endoscopic specimen retrieval bag.
♦ Specialized equipment is also necessary for vessel ligation and hemostasis. A variety of devices can be used, including laparoscopic staplers with vascular loads, clip appliers, ultrasonic coagulation, or bipolar electrocoagulation devices.
♦ Laparoscopic ultrasound may be helpful in locating accessory spleens or identification of vascular supply.
Anesthetic
♦ Laparoscopic splenectomy is performed under general anesthesia.
♦ Typically, sequential compression devices (SCDs) are placed on the lower extremities for deep venous thrombosis (DVT) prophylaxis.
♦ Preoperative antibiotics should be administered. A first-generation cephalosporin, such as cefazolin, is appropriate.
♦ A nasogastric tube is used to decompress the stomach during surgery, but it may be removed at the end of the operation.
♦ A Foley catheter can be placed before surgery and removed at the conclusion if a prolonged operative time is expected.
♦ Invasive monitoring is typically not needed for elective cases unless the patient has significant underlying cardiopulmonary disease.
♦ Platelets should be available for transfusion if patient is severely thrombocytopenic (<20,000).
Positioning
♦ The patient is placed in the right lateral decubitus position.
♦ Flexion of the operating table improves access. The kidney rest can also be used to increase the space between the costal margin and the anterior superior iliac spine.
♦ Stabilization of the patient’s position can be achieved using a beanbag device or rolls on either side of the patient.
♦ The reverse Trendelenburg position may aid with exposure of the hilum.
♦ Both the surgeon and the assistant typically stand on the right side of patient.
♦ The surgeon needs to be prepared for the possibility of conversion to an open procedure through a left subcostal or midline incision when placing the drapes.
Step 3. Operative steps
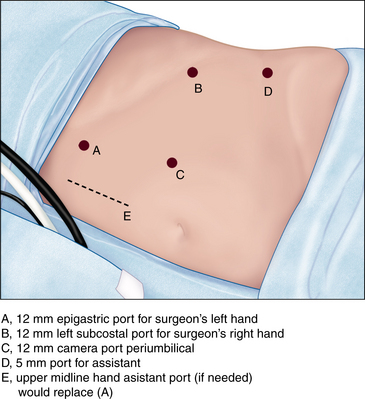
Access and port placement
♦ A Veress needle is inserted through a small left subcostal incision for insufflation, unless there are left upper quadrant adhesions or a prohibitively large spleen.
♦ Using a 30-degree endoscope greatly facilitates visualization.
♦ Once the camera and ports are introduced, a visual examination of the abdomen is made to search for access injuries and accessory spleens.
♦ The objective is to triangulate the ports (camera and working instruments) around the spleen:
Description of procedure
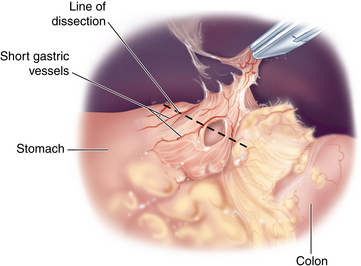
Splenic flexure mobilization
♦ The first step is to mobilize the splenic flexure of the colon medially by incising the splenocolic ligament. To avoid colonic injury, electrocautery is used sparingly (Figure 13-2).
♦ Entry into Gerota’s fascia posteriorly should be avoided.
♦ The gastrosplenic ligament and short gastric vessels are best divided with appropriate energy devices or ultrasonic coagulation.
♦ The splenophrenic ligament provides excellent lateral retraction of the spleen and should be left intact until the final steps of the procedure.
♦ The spleen is then elevated, exposing the vascular hilum medially.
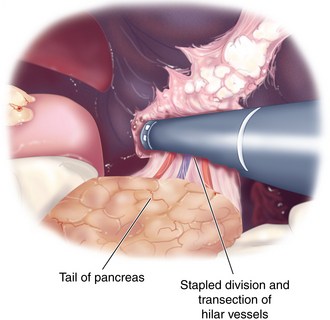
♦ Hilar vessels are ligated and divided using electrocautery, ultrasonic shears, hand ties, or staplers. These devices can also be used in combination depending on the size of the vessels and hilar vascular anatomy (Figure 13-3).
♦ Care is taken to avoid injury to the pancreatic tail.
♦ When possible, the artery is ligated first, followed by the vein, but this often depends upon hilar anatomy.
♦ Once the hilum is divided, the posterior and lateral attachments are divided.
Removal of spleen
♦ The approach for splenic removal will depend on size and pathology. Usually the spleen is placed into an endoscopic bag, and the opening of the bag is brought through the left subcostal port site with extension of the incision or hand port incision, if present.
♦ The spleen is morcellated within the bag using ringed forceps and removed piecemeal.
♦ Care must be taken not to rupture the bag or spill splenic tissue into the peritoneal cavity.
♦ A larger spleen that needs to be examined intact may require the surgeon to extend the incision, or connect two incisions, for extraction.
Step 4. Postoperative care
♦ Patients are typically admitted to the hospital for 1 to 2 days postoperatively for recovery.
♦ Nasogastric decompression is not necessary in most patients.
♦ Postoperative hematocrit or platelet count may be checked.
♦ A liquid diet is initiated on postoperative day 1 and advanced as tolerated.
♦ Pain management generally includes patient-controlled analgesia (PCA) with or without nonsteroidal anti-inflammatory agents.
Step 5. Pearls and pitfalls
♦ Clips should be avoided near the hilar vessels because they can become caught within a stapling device and will result in an inadequate deployment of staples.
♦ Platelet transfusion should occur after the artery is ligated to provide maximum benefit and avoid sequestration.
♦ The inspection for any accessory spleens should occur at the beginning of the procedure prior to disruption of the field.
♦ The specimen retrieval bag should be monitored with the laparoscope during morcellation to avoid rupture.
George JN, Woolf SH, Raskob GE, et al. Idiopathic thrombocytopenic purpura: a practice guideline developed by explicit methods for the American Society of Hematology. Blood. 1996;88;1:3-40.
Keidar A, Feldman M, Szold A. Analysis of outcome of laparoscopic splenectomy for idiopathic thrombocytopenic purpura by platelet count. Am J Hematol. 2005;80(2):95-100.
Schilling RF. Estimating the risk for sepsis after splenectomy in hereditary spherocytosis. Ann Intern Med. 1995;122(3):187-188.