CHAPTER 29 Splenectomy
Step 1: Surgical Anatomy
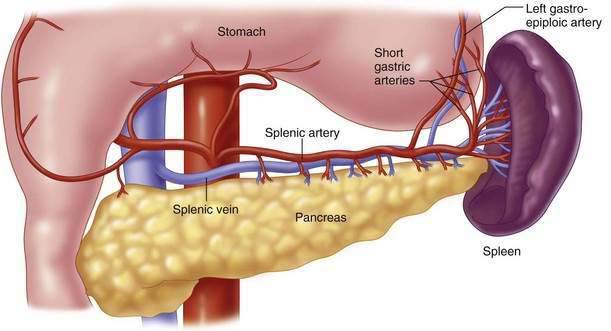
♦ The spleen is positioned anterior to the costodiaphragmatic recess, lateral to the greater curvature of the stomach, adjacent to the tail of the pancreas, anterior to the left kidney, and superior or posterior to the splenic flexure of the colon.
♦ The parietal peritoneum adheres to the splenic capsule along its lateral border opposite the hilum. These attachments make up the suspensory ligaments of the spleen, which tend to be avascular.
♦ The splenorenal ligament extends from the left kidney to the hilum of the spleen and is where the splenic vessels and tail of the pancreas are invested.
♦ The splenic artery arises from the celiac trunk and travels along the superior edge of the pancreas, where it branches to form the short gastric, left gastroepiploic, and terminal splenic branches (Fig. 29-1).
Step 2: Preoperative Conditions
Hematologic Disorders
Immune Thrombocytopenic Purpura
♦ Immune thrombocytopenic purpura (ITP) is characterized by a low platelet count, normal bone marrow, and an absence of other diseases that can cause thrombocytopenia.
♦ Splenectomy is used primarily only in patients with refractory severe symptomatic thrombocytopenia failing medical therapy.
 Indications include patients with ITP for 6 weeks and a platelet count of less than 10,000, irrespective of bleeding symptoms.
Indications include patients with ITP for 6 weeks and a platelet count of less than 10,000, irrespective of bleeding symptoms.
 Indications include patients with ITP for 6 weeks and a platelet count of less than 10,000, irrespective of bleeding symptoms.
Indications include patients with ITP for 6 weeks and a platelet count of less than 10,000, irrespective of bleeding symptoms.Hereditary Spherocytosis
♦ An autosomal dominant disease resulting from a deficiency of spectrin, which leads to membrane abnormalities.
Tumors
♦ Splenectomy was formerly used to assist in the staging of Hodgkin’s lymphoma. However, with the increasing accuracy of noninvasive imaging, including computed tomography (CT) scan, lymphangiography, and positron emission tomography scans, the number of staging splenectomies performed has decreased.
Cysts
♦ True cysts are further subdivided into parasitic and nonparasitic cysts.
 Most parasitic cysts are due to Echinococcus, which can be identified by the presence of calcifications and daughter cysts seen on CT scans.
Most parasitic cysts are due to Echinococcus, which can be identified by the presence of calcifications and daughter cysts seen on CT scans.
 Spillage or rupture of a hydatid cyst may cause anaphylaxis and contaminate the entire peritoneal cavity with infective scolices.
Spillage or rupture of a hydatid cyst may cause anaphylaxis and contaminate the entire peritoneal cavity with infective scolices.
 Splenectomy is the treatment of choice for parasitic cysts; however, injections of 3% normal saline, alcohol, and 0.5% silver nitrate are alternative treatments.
Splenectomy is the treatment of choice for parasitic cysts; however, injections of 3% normal saline, alcohol, and 0.5% silver nitrate are alternative treatments.
 Most parasitic cysts are due to Echinococcus, which can be identified by the presence of calcifications and daughter cysts seen on CT scans.
Most parasitic cysts are due to Echinococcus, which can be identified by the presence of calcifications and daughter cysts seen on CT scans. Spillage or rupture of a hydatid cyst may cause anaphylaxis and contaminate the entire peritoneal cavity with infective scolices.
Spillage or rupture of a hydatid cyst may cause anaphylaxis and contaminate the entire peritoneal cavity with infective scolices. Splenectomy is the treatment of choice for parasitic cysts; however, injections of 3% normal saline, alcohol, and 0.5% silver nitrate are alternative treatments.
Splenectomy is the treatment of choice for parasitic cysts; however, injections of 3% normal saline, alcohol, and 0.5% silver nitrate are alternative treatments.Step 3: Operative Technique
Laparoscopic Splenectomy
♦ The colon should be decompressed with either an enema or a laxative on the day before surgery, which will aid in visualization of the spleen.
♦ A nasogastric tube should be used to decompress the stomach, and a Foley or Credé maneuver is used to empty the bladder before prepping and draping the patient.
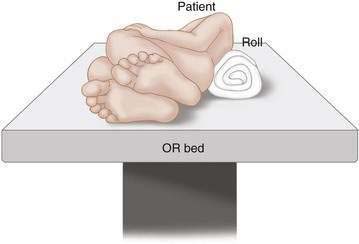
♦ The patient should be placed in the supine position.
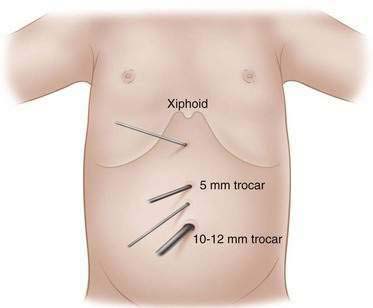
♦ A 10- to 12-mm umbilical trocar should be placed, and a 5-mm 30- to 70-degree laparoscope is used to identify the spleen.
♦ Both surgeon and assistant will operate from the patient’s right side.
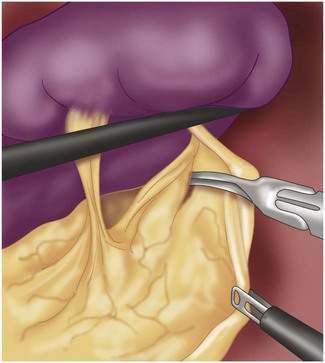
♦ Initially the omental attachments to the caudal aspect of the spleen are divided using a cautery device (Fig. 29-4).
♦ The short gastric vessels are then identified in the gastrosplenic ligament by placing traction on the greater curve of the stomach.
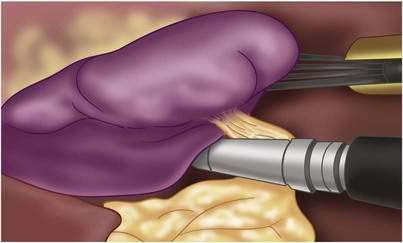
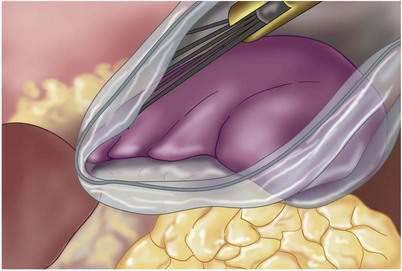
♦ After the short gastric vessels have been divided, the spleen is retracted medially to expose the suspensory ligaments. These avascular ligaments are divided so that the only remaining area of attachment is the hilum.
Open Splenectomy
♦ Open splenectomies are not done as commonly any longer, but there are circumstances when this approach is needed.
♦ After identifying the spleen, dorsal and medial traction should be placed on the spleen to stretch and define the splenorenal and splenophrenic ligaments.
♦ The incision begins at the caudal omental attachments, extends into the lesser sac, and continues to the stomach and short gastric vessels.
♦ The dissection around the spleen laterally should continue until the suspensory ligaments have been transected and the spleen is delivered to the level of the wound.
♦ After complete mobilization of the spleen, traction is placed on the gastrosplenic ligament to expose the short gastric vessels. These are divided with sutures or an energy device.
♦ The splenic artery is then identified at the superior border of the pancreas, and the artery and vein are separately divided and ligated.
♦ In some cases the tail of the pancreas will extend into the hilum; in these patients it is recommended to divide the vessels after they have branched to avoid a pancreatic injury.
Step 4: Postoperative Care
Thrombocytosis
Overwhelming Post-Splenectomy Infection
♦ The incidence of overwhelming post-splenectomy infection (OPSI) is difficult to determine.
♦ The presenting symptoms of patients with OPSI include fever, chills, sore throat, malaise or myalgia, diarrhea, and vomiting.
♦ Progression may be rapid with development of shock, disseminated intravascular coagulation, respiratory distress, coma, and death within hours of presentation.
Step 5: Pearls and Pitfalls
Brunicardi F, Andersen D, Billiar T, et al. Schwartz’s principles of surgery, 8th ed. New York: McGraw-Hill Professional; 2004.
Cameron JL. Current surgical therapy, 8th ed. St. Louis: Mosby; 2007.
Mulholland M, Lillemore K, Doherty G, et al. Greenfield’s surgery: Scientific principles and practice, 4th ed. Baltimore: Williams & Wilkins; 2005.
Netter F. Atlas of human anatomy, 4th ed. Philadelphia: Saunders; 2006.
Townsend C, Beauchamp R, Evers B, Mattox K. Sabiston textbook of surgery, 17th ed. Philadelphia: Saunders; 2004.