CHAPTER 71 Spleen
The spleen consists of a large encapsulated mass of vascular and lymphoid tissue situated in the upper left quadrant of the abdominal cavity between the fundus of the stomach and the diaphragm. Its shape varies from a slightly curved wedge to a ‘domed’ tetrahedron. The shape is mostly determined by its relations to neighbouring structures during development. The superolateral aspect is shaped by the left dome of the diaphragm with the inferomedial aspect being influenced mostly by the neighbouring splenic flexure of the colon, the left kidney and stomach. Its long axis lies approximately in the plane of the tenth rib. Its posterior border is approximately 4 cm from the mid-dorsal line at the level of the tenth thoracic vertebral spine. Its anterior border usually reaches the mid-axillary line.
RELATIONS
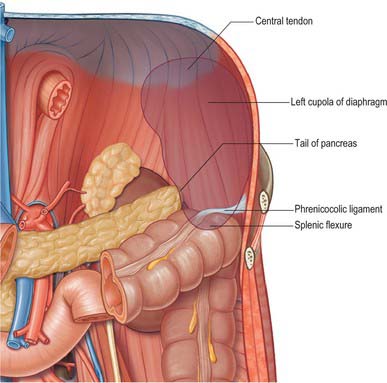
The spleen has a superolateral diaphragmatic and an inferomedial visceral surface (Fig. 71.1). There are superior and inferior borders and anterior and posterior extremities or poles. The diaphragmatic surface is convex and smooth and faces mostly superiorly and laterally although the posterior part may face posteriorly and almost medially as it approaches the inferior border. The diaphragmatic surface is related to the abdominal surface of the left dome of the diaphragm which separates it from the basal pleura, the lower lobe of the left lung and the ninth to eleventh left ribs (Fig. 71.2). The pleural costodiaphragmatic recess extends down as far as its inferior border. The visceral surface faces inferomedially towards the abdominal cavity, and is irregular and marked by gastric, renal, pancreatic and colic impressions. The gastric impression faces anteromedially and is broad and concave where the spleen lies adjacent to the posterior aspect of the fundus, upper body and upper greater curvature of the stomach. It is separated from the stomach by a peritoneal recess, which is limited by the gastrosplenic ligament. The renal impression is slightly concave and lies on the lowest part of the visceral surface, separated from the gastric impression above by a raised strip of splenic tissue and the splenic hilum. It faces inferomedially and slightly backwards, being related to the upper and lateral area of the anterior surface of the left kidney and sometimes to the superior pole of the left suprarenal gland. The colic impression lies at the inferior pole of the spleen and is usually flat. It is related to the splenic flexure of the colon and the phrenicocolic ligament. The pancreatic impression is often small when present and lies between the colic impression and the lateral part of the hilum. It is related to the tail of the pancreas which lies in the splenorenal ligament. The hilum of the spleen is a long fissure pierced by several irregular apertures through which the branches of the splenic artery and vein as well as nerves and lymphatics enter and leave the spleen; it lies in the visceral surface closer to the inferior border and anterior border.
PERITONEAL CONNECTIONS OF THE SPLEEN
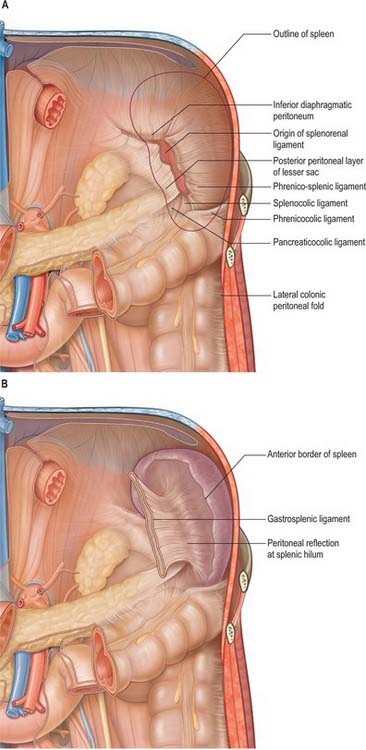
The spleen is almost entirely covered by peritoneum that adheres firmly to its capsule, and is separated from the stomach and left kidney by recesses of the greater sac. It develops in the upper dorsal mesogastrium (see Figs 73.6 to 73.7), and remains connected via folds of peritoneum to the posterior abdominal wall (by the splenorenal, phrenicocolic and phrenicosplenic ligaments) and to the anterolateral abdominal wall and stomach (by the gastrosplenic ligament) (Fig. 71.3A). The splenorenal ligament is formed from two layers of peritoneum. The anterior layer is continuous with the peritoneum of the posterior wall of the lesser sac over the left kidney and with peritoneum of the splenic hilum where it runs into the posterior layer of the gastrosplenic ligament. The posterior layer of the splenorenal ligament is continuous with the peritoneum over the inferior surface of the diaphragm and runs onto the splenic surface over the renal impression. The splenic vessels lie between the layers of the splenorenal ligament: the tail of the pancreas is usually present in its lower portion (see Fig. 64.5B). The length of the splenorenal ligament may vary. Longer ligaments tend to make the spleen more mobile and may predispose the spleen to injury due to rotational shear forces during trauma, however they also make the mobilization of the spleen easier during surgery. The presence of the pancreatic tail within the splenorenal ligament must be remembered because it can be injured during ligation of the splenic vessels, causing pancreatitis or a pancreatic duct fistula to form.
The gastrosplenic ligament also has two layers (Fig. 71.3B). The posterior layer is continuous with the peritoneum at the splenic hilum and over the posterior aspect of the stomach. The anterior layer is formed from the peritoneum that is reflected off the gastric impression and reaches the greater curvature of the stomach anteriorly. The short gastric and left gastroepiploic branches of the splenic artery pass between its layers. Division of the gastrosplenic ligament during surgery may be hazardous if the ligament is short because ligation of the short gastric vessels may risk injury to the greater curvature of the stomach.
VASCULAR SUPPLY AND LYMPHATIC DRAINAGE
Splenic artery
The spleen is supplied exclusively from the splenic artery (see Fig. 70.7). This is the largest branch of the coeliac axis and its course is among the most tortuous in the body. From its origin the artery runs a little way inferiorly, then turns rapidly to the left to run initially horizontally above the level of the neck of the pancreas, before ascending as it passes more laterally. It is less steeply inclined than the body and tail of the pancreas and so comes to lie posterior to the superior border of the gland. It lies in multiple loops or even coils which appear above the superior border of the pancreas and descend to lie behind the gland. The splenic artery lies anterior to the left kidney and left suprarenal gland and runs in the splenorenal ligament posterior to the tail of the pancreas. It divides into two or three main branches before entering the hilum of the spleen (Fig. 71.1). As these branches enter the hilum they divide further into four or five segmental arteries that each supply a segment of the splenic tissue. There is relatively little arterial collateral circulation between the segments, which means that occlusion of a segmental vessel often leads to infarction of part of the spleen. There is, however, considerable venous collateral circulation between the segments, making segmental resection of the spleen practically impossible. The splenic artery gives off various branches to the pancreas in its course and gives off short gastric arteries to the stomach just prior to dividing or from its terminal branches.
Splenic vein
The splenic vein is formed within the splenorenal ligament, close to the tip of the tail of the pancreas, by five or six tributaries that emerge from the hilum of the spleen (Fig. 71.4). The tributaries are thin walled and often spread over several centimetres because the hilum is long and thin (Fig. 71.1). This must be remembered during surgical removal of the spleen because the venous tributaries must be divided close to the hilum to avoid injury to the pancreatic tail. They should be ligated in several groups to prevent the risk of avulsion of the veins from the splenic hilum and consequent profuse bleeding before the resection is complete.
INNERVATION
The spleen is innervated by the splenic plexus, which consists of branches of the coeliac plexus, left coeliac ganglion and right vagus that accompany the splenic artery. The fibres are mainly sympathetic and terminate around blood vessels and in the non-striated muscle of the splenic capsule and trabeculae. Most appear to be noradrenergic, vasomotor, and are concerned with the regulation of blood flow through the spleen. Adrenergic agonists inhibit the concentration of red cells in the splenic blood (so called ‘plasma skimming’) indicating that sympathetic activity causes an increase in the ‘fast’ circulation of the spleen as opposed to slow filtration (Reilly 1985).
MICROSTRUCTURE
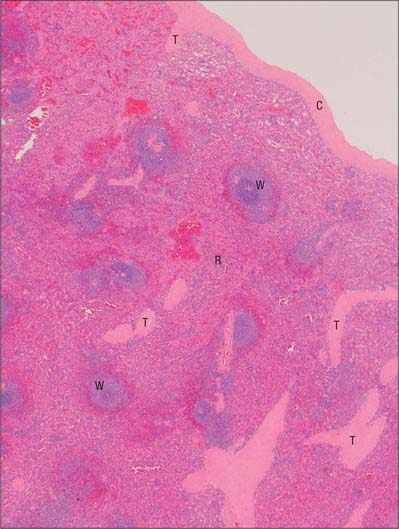
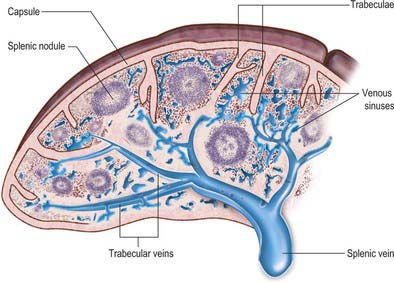
Microscopically, the parenchymal tissue of the spleen consists of two major components, white pulp and red pulp, named on the basis of their appearance when a fresh spleen is transected (Fig. 71.5). The white pulp is composed of lymphoid tissue in which B and T lymphocytes mature and proliferate under antigenic stimulation (Fig. 71.6). The red pulp is a unique filtration device that enables the spleen to clear particulate material from the blood as it perfuses the spleen. It is composed of a complex system of interconnected spaces populated by large numbers of phagocytic macrophages that remove effete red blood cells, microorganisms, cellular debris and other particulate matter from the circulation.
Fibrous framework of the spleen
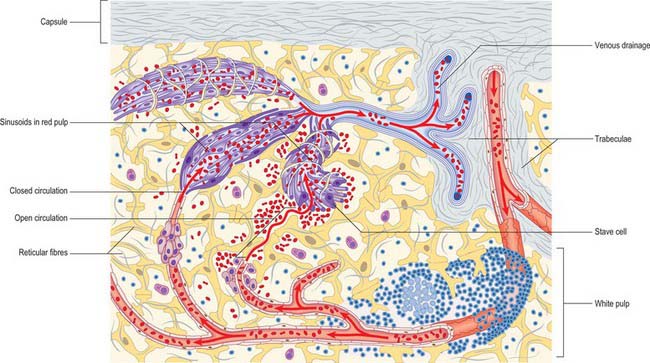
The serosa of the peritoneum covers the entire organ except at its hilum and along the lines of reflexion of the splenorenal and gastrosplenic ligaments. Deep to this layer is the connective tissue capsule, a continuous layer approximately 1.5 mm thick, containing abundant type I collagen fibres and some elastin fibres. The capsule has an outer and an inner lamina in which the directions of the collagen fibres differ, thereby increasing its strength. Numerous trabeculae extend from the capsule into the substance of the spleen, where they branch to form a supportive framework. The largest trabeculae enter at the hilum and provide a conduit for the splenic vessels and nerves, dividing into branches in the splenic pulp (Figs 71.6 and 71.7). Within the spleen, these branches become continuous with a delicate network of type III (reticular) collagen fibres that pervades both red and white pulps and is secreted by fibroblasts within its meshes.
Red pulp
The red pulp constitutes the majority (75%) of the total splenic volume. It contains large numbers of venous sinusoids that ultimately drain into tributaries of the major splenic veins. The sinusoids are separated from each other by a fibrocellular network consisting of small bundles of delicate collagen type III fibres, the reticulum, and numerous reticular fibroblasts and splenic macrophages. Seen in two-dimensional sections, these intersinusoidal regions appear as strips of tissue, the splenic cords, which alternate with splenic sinuses (Fig. 71.6). In reality, they form a three-dimensional continuum around the venous spaces.
Venous sinusoids
Venous sinusoids are elongated ovoid vessels approximately 50 μm in diameter, lined by a characteristic, ‘incomplete’ endothelium that is unique to the spleen. Their endothelial cells are long and narrow, and aligned with the long axis of the sinusoid; they are often called stave cells, because they are reminiscent of planks in a barrel (Fig. 71.6). Stave cells are attached to their neighbours at intervals along their length by short stretches of intercellular junctions. These junctions alternate with intercellular slits which allow blood cells to squeeze into the lumen of the sinusoid from the surrounding splenic cords. A discontinuous basal lamina is present on the abluminal aspect of the sinus. The sinusoids are supported externally by circumferentially and longitudinally disposed reticular fibres, which are components of the fibrous reticulum.
Splenic microcirculation
Open and closed splenic circulations
Views on the intermediate circulation of the spleen differ on whether blood passes from the arterioles (or their terminal capillaries) directly into the venous sinuses (a closed circulation), or is instead discharged into a network of spaces in the splenic cords before entering the sinuses through the minute slits in their walls (an open circulation). In humans, evidence favours the presence of an anatomically and physiologically open circulation, in which blood percolates slowly through the reticular tissue of the splenic cords and filters through slits in the sinus walls before joining the majority of the blood flow (see Fig. 71.6). There is thought to be an additional closed vascular route, but this is likely to provide only a minor contribution to splenic circulation.