CHAPTER 43 Spinal Orthoses
INTRODUCTION
Spinal orthoses are external devices which are typically applied circumferentially about the body with the intent of altering spinal motion. Lumbar supports fashioned from tree bark have been found in pre-Columbian cliff dwellings, and the use of orthoses was described both by Hippocrates and Galen.1 Centuries later, in the United States alone, some 1.8 million people use a spinal orthosis in any given year.2
CLASSIFICATION OF ORTHOSES
In 1973, the Task Force on the Standardization of Prosthetic-Orthotic Terminology Committee proposed a systematic nomenclature in which spinal orthoses are named by the segments that are immobized by the device.3 An orthosis spanning the cervical spine is a cervical orthosis (CO). An orthosis spanning the thoracic, lumbar, and sacral spine is a thoracolumbosacral orthosis (TLSO), while an orthosis spanning the lumbar and sacral spine is a lumbosacral orthosis (LSO). This terminology is accepted by all the major professional organizations which commonly deal with the devices, including the American Academy of Orthotics and Prosthetics, the American Academy of Physical Medicine and Rehabilitation, and the American Academy of Orthopedic Surgeons. The Center for Medicare and Medicaid Services (CMS), which is the most common payer for such devices, utilizes a procedural coding system which is based upon this terminology.
BIOMECHANICS
In the upper cervical spine, the occipitoatlantal joint accounts for 20% of the total available cervical flexion and extension. The atlantoaxial joint or C1–2 accounts for 14% of the total available cervical flexion and extension and 54% of the total available cervical rotation. Motion at these joints, however, accounts for only 10% of lateral bending. The greatest cervical flexion and extension takes place at C5–6 and C6–7, whereas the greatest side bending occurs at C2–3 and C3–4 with relatively less motion occurring at the lowest cervical levels.4
The thoracic facets are angled on average only 20° from the coronal plane and are positioned obliquely to the transverse and sagittal planes. Thus, lateral bending is most freely allowed at these segments. This mechanical feature is counterbalanced in the upper thoracic spine by the presence of the rib cage. The thoracic spine has been shown to be 27% stiffer in flexion, 45% stiffer in lateral bending, and 132% stiffer in extension due to the stabilizing effect of the rib cage.5 Upper thoracic segments are most mobile in axial rotation, while lower thoracic regions, less restricted by the ribs, allow the most lateral bending, flexion, and extension.4
The lumbar facet joints, which lay nearly parallel to the sagittal plane and at a nearly transverse angle to the transverse and coronal planes, will allow full flexion and extension, but limit rotation and side bending. Due to the true axis of rotation, obliquity, and contour of joint surfaces, there is some gliding of facet surfaces and some motion in the transverse and coronal planes; however, normal lumbar motion for flexion and extension is by far greater than normal lumbar axial rotation and lateral bending.4,6
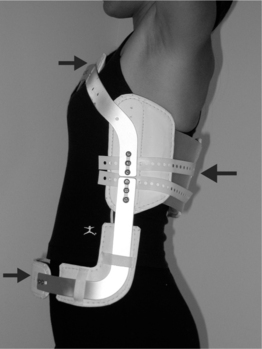
Motion control by spinal orthoses is based on the principle of a three-point pressure system. This is illustrated most readily with the flexion control TLSO Jewitt orthosis seen in Figure 43.1. The orthosis provides posteriorly directed forces originating from the sternal and suprapubic pads and an anteriorly directed force originating from the thoracolumbar pad. This configuration encourages hyperextension of the spine. Thus, a simple anterior wedge compression fracture located at the midpoint of the thoracolumbar pad would be ideally treated with this type of brace. Care must be taken when prescribing an orthoses to ensure that the site of intended action is located near the central fulcrum of the three-point system. Poorly prescribed devices can create destabilizing forces and worsen injuries.
With more complex fractures or disease, rotatory control may be required. Depending on the site of injury, the orthosis will be extended and incorporate more body surface contact area, typically in the form of a body jacket. For a T7–L3 level injury a full skin contact TLSO with a high-profile trim line extending to just below the clavicles can control rotation by acting against the opposite anterior superior iliac crest. Rotational control at L5–S1 is best achieved with a low-profile TLSO with a hip spica.7 If motion control is desired above the T7 level some authors recommend a cervical extension be added.8–10 When doubt exists about the effectiveness of a brace, flexion and extension radiographs can be taken while the patient is wearing the orthosis, keeping in mind special beam angulations may be required to avoid artifact due to the superimposition of the image of the orthosis on the image of the desired spinal segments.
CERVICAL ORTHOSES
The term ‘soft collar’ refers to a broad strip of open-cell foam, plastic, or foam rubber encased in cotton stockinet with a Velcro closure (Fig. 43.2). It is the least restrictive and most common cervical orthosis. Soft cervical collars generally provide minimal restriction in range of motion.11–13 A collar which is too large tends to force the neck into extension, potentially decreasing the size of the neural foramina. A soft collar which positions the neck into approximately 10° of flexion maximizes the size of the foramina and minimizes the potential for nerve root irritation. A soft collar with the Velcro closure placed in the front may provide increased resistance to flexion, whereas a collar with the Velcro closure placed in the back may provide increased resistance to extension.13 A soft collar can provide warmth and comfort which may reduce pain and muscle spasm. Moreover, it often acts as a reminder for a person to avoid an active range of motion which may be painful. Another CO, the Thomas collar, initially developed by Hugh Owen Thomas, a physician in the nineteenth century, is a rigid collar, originally made of sheet metal and now typically made from rigid polyethylene, which mainly acts to restrict flexion and extension up to about 75% from neutral.14 It offers little control of lateral bending or rotation due to its lack of head and thorax contact.
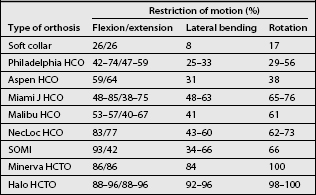
The Philadelphia, Miami J, Aspen, Malibu, NecLoc, and Stiffneck collars are also hard collars made of different materials with different types of linings. However, unlike the COs described above, these orthoses incorporate the mandible and the occiput in their design and can be classified as head cervical orthoses or HCOs. They provide head support and partially restrict motion of cervical spine in all planes, especially in the sagittal plane (Table 43.1). The Philadelphia HCO, which consists of two pieces of closed-cell polyethylene foam attached with Velcro closures (Fig. 43.3), is prototypical of the wide variety of HCOs which are produced in a multitude of sizes and shapes by different manufacturers. The Philadelphia HCO, like other prefabricated HCOs, is available in multiple configurations to accommodate a variety of clinical needs and neck shapes, including a snugly fitting version which can be used to control hypertrophic scarring.22 The Miami J and the Aspen HCOs consist of a two-piece semirigid plastic supporting structure with removable open cell foam liners. This design is often better tolerated than the solid orthoses made of closed-cell foam. In many instances, persons who require a HCO for an extended period of time will have a solid closed-cell foam orthosis, such as the Philadelphia collar, for showering and a HCO constructed like the Miami J or Aspen for everyday use. With regards to effectiveness in restriction of motion, numerous studies have been performed comparing the different types of HCOs. The results vary by study methodology, often with conflicting results.23,24
Cervical orthoses that include rigid vertical posts are cooler than hard collars, due to the lack of total skin contact, and are more stabilizing as they incorporate an additional inferior portion which is supported on the upper thorax. They are classified as head cervical thoracic orthoses or HCTOs. These orthoses may include two, three or four posts (Fig. 43.4). A prototypical HCTO is the three-posted sternal occipital mandibular immobilizer (SOMI) (Fig. 43.5). Because of its points of attachment, as described in its name, the SOMI greatly restricts cervical flexion, particularly lower cervical segments; however, because of a swivel-type occipital pad, it allows some extension.11 Lateral bending is also less restricted than flexion.
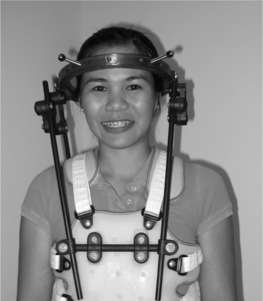
Maximal cervical immobilization is achieved with either a halo vest orthosis (Fig. 43.6) or a Minerva orthosis (Fig. 43.7). Both devices are HCTOs. A halo vest consists of a metal ring which is fixed to the outer table of the skull by four screws, a plastic chest jacket, and superstructure of bars and connectors which connect the ring to the jacket. The jacket is usually lined with sheepskin to improve pressure distribution and comfort. Due to the fixation of the halo ring to the skull, a halo vest has optimal rotational motion control. As a result, it is commonly used to immobilize the upper cervical segments, which, as described earlier, are the segments responsible for the majority of rotation of the cervical spine. However, because of its lack of total contact over the neck, intersegmental snaking of vertebral segments has been reported to occur.25,26 A Minerva HCTO, which has greater skin contact, may provide better control of this intersegmental motion and this may be a better option if this is a major concern.27 The Minerva orthoses may be prefabricated or custom made. The posterior section has a padded band that extends forward to encircle both the mandible and the forehead, thus creating a longer lever arm for cervical control.28 Its name derives from the mythological daughter of Zeus, a warrior who radiated thunderbolts from her forehead. One disadvantage of the halo device as compared to the Minerva orthosis is that it significantly changes the center of gravity of the wearer, potentially leading to balance difficulties and falls.29 Another disadvantage is the requirement of the halo to have pins seated into the skull which presents a risk for both infection and slippage.
THORACOLUMBOSACRAL ORTHOSES
The effects of a TLSO on the restriction of spinal motion, intra-abdominal pressure, intradiscal pressure, and muscle activity have all been studied, with conflicting results.30–32 No study has yet shown even near complete elimination of either segmental or gross spinal mobility by any orthosis. In one study of subjects without spinal abnormalities, who were custom fitted with a lumbosacral corset, chairback orthosis, or molded plastic TLSO, it was found that all three restricted gross body motion.31 Approximately two-thirds to one-half of orthotic free gross body motion was observed.31 When a mean percentage of restriction of all directional movement was calculated, the TLSO was found to be twice as effective as the corset, while the chairback brace was of intermediate effectiveness. The spinal motion controlled by wearing a TLSO is greatest at the upper and midlumbar segments. In contrast, motion controlled at the L4–S1 levels by wearing a TLSO is only minimal: an 8–12% reduction, or even an increase, as compared to spinal motion without a TLSO in place.30,33
Although increased intra-abdominal pressure is associated with increased lumbar spinal stability and decreased spinal load, the effect of a TLSO on abdominal muscle activity and abdominal pressure is controversial.32–36 Nevertheless, the available evidence seems to support that intra-abdominal pressure plays a role in the stabilization of the lumbar spine by a TLSO.
The effect of a TLSO or LSO on intradiscal pressure is also uncertain. Nachemson showed intradiscal pressure decreased by about 25% when subjects wore an inflatable lumbar corset.37 However, when he studied several other lumbar orthoses, an inconsistent effect on intradiscal pressure was found.38 Rohlmann studied several different lumbar orthoses regarding the effect on the load on an internal spinal fixation device, and did not find any reduction of the load by any of the orthoses.39 Since intradiscal pressure is increased with spinal flexion and decreased with the extension, a TLSO may indirectly reduce intradiscal pressures by restricting flexion.
If the principal objective of a prescribed orthosis is to limit flexion and extension of the thoracic spine, and there is not a strong need for rotational control, a simple flexion control orthosis is a good option. There are two principal types of flexion control TLSOs: the cruciform anterior spinal hyperextension (CASH) brace and the Jewitt orthosis (see Fig. 43.1 and 43.8). The basic biomechanical principles underlying these orthoses is a three-point fixation.. Such orthoses are commonly made of flat aluminum bars with a vinyl-covered foam pad attached posteriorly over the midspine and two other vinyl-covered foam pads attached anteriorly over the sternum and pubis. The Jewitt orthosis is most effective for simple compression fractures or thoracic sprains between T7 and L1. It should be avoided for fractures or thoracic sprains above T6 as the sternal pad can act as fulcrum and actually worsen the condition.
The chairback orthosis is a traditional, partially open orthosis for the lower spine that can be classified as a lumbosacral flexion extension control orthosis (LS FEO). This orthosis restricts trunk flexion through a posteriorly directed force across the superior and inferior aspects of the anterior abdominal corset and an anteriorly directed force from the center of the two posterior uprights. Extension is limited by anteriorly directed forces from the thoracic and pelvic bands, and posteriorly from the midsection of the abdominal corset.40 Currently, this orthosis is primarily used to treat low back pain in a stable spine rather than for fracture immobilization since other orthoses offer greater restriction of motion.41 The chairback orthosis can be seen as basic building block to which additional supports can be added to increase support and restriction of motion. By adding lateral supports, the chairback becomes a Knight spinal orthosis or a lumbosacral flexion extension lateral control orthosis (LS FELO) (Figs 43.9, 43.10). This orthosis is also mainly used for low back pain in a stable spine and sometimes for immobilization of stable lumbar fractures which have maintained their vertebral body height.41 By extending the chairback orthosis superiorly to include the thoracic spine through posterior uprights that terminate above the scapula, the orthosis becomes a Taylor orthosis or a thoracolumbosacral flexion extension control orthosis (TLS FEO). Biomechanically, the interscapular band and the axillary straps in the Taylor orthosis resist extension and flexion, respectively. When a Knight LS FELO design extends superiorly to encompass the thoracic spine similar to a Taylor TLS FEO, a Knight-Taylor orthosis or a thoracolumbosacral flexion extension lateral control orthosis (TLS FELO) is created (Fig. 43.11). This orthosis provides increased resistance to lateral bending, in addition to flexion and extension, by the addition of long vertical lateral supports to which the thoracic and pelvic bands attach.
The Williams flexion orthosis, a lumbosacral extension lateral control orthosis (LS ELO), is another traditional, partially open orthosis. It was originally designed for treatment of spondylolisthesis and is still used for that purpose today.42,43 Extension is limited by posterior oblique bars and a pelvic band, but some flexion is allowed due to a mobile anterior thoracic band. Lateral bending is restricted by lateral bars attached to the thoracic and pelvic bands. All of the aforementioned orthoses with an open design will allow some rotatory movement of the spine. A thermoplastic version of the Williams flexion orthosis is available which is called the Raney flexion LSO. This orthosis has semirigid anterior and posterior shells, which immobilize the lumbosacral spine in a flexed position, not allowing further flexion as is possible with the Williams flexion orthosis. The Raney flexion LSO is an LS FELO.
When rotatory control is necessary, a more restrictive TLSO which encases the trunk, such as the commonly prescribed plastic body jacket, is required (Fig. 43.12). These TLSOs are known as thoracolumbosacral flexion extension lateral rotatory control orthoses (TLS FELROs). Some body jacket models have a posterior inflatable pillow intended to adjust the snugness of fit. When a high trim line with subclavian pads is employed these orthoses are known colloquially as cowhorn braces. A shorter version of the body jacket, an LS FELRO, which ends below the xiphoid process and scapula, is designed to restrict motion in the lower trunk to L3 (Fig. 43.13). A rigid TLS FELRO or LS FELRO depending on the level of abnormality is the orthosis of choice for postsurgical immobilization or external stabilization of lumbar fracture. However, it should be noted that a rigid TLS FELRO or LS FELRO may actually increase motion of L5–S1 level as mentioned earlier.30 If it is necessary to immobilize this level, then a hip spica extension should to be attached to the orthosis.
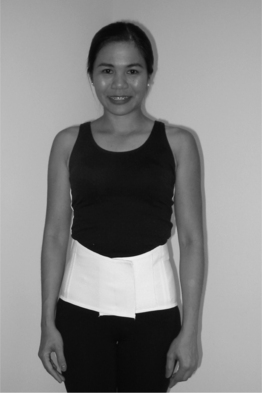
The most frequently prescribed orthosis for low back pain is an LS corset (Fig. 43.14). Typically, these are flexible orthoses, less restrictive than those mentioned above, made of fabric that is woven with synthetic elastic material. The upper extent of the orthoses, which encircle the torso, is the xiphoid process anteriorly and a point just below the lower margin of scapula posteriorly, while the lower extent is the pubic symphysis and apices of the buttocks. Laces or Velcro straps allow for control of fit. Many are reinforced with either metal or plastic removable stays that can be inserted into an incorporated posterior pocket. Due to the elastic nature of the LS corsets, if worn snugly, intra-abdominal cavity pressures may increase thereby reducing the loading force on the spine. LS corsets provide a moderate degree of lumbosacral motion control.44 In addition, LS corsets may provide warmth to lumbar area, improve trunk proprioception, and act as a reminder for avoiding lumbosacral motion which may cause pain.45
Sacroiliac orthoses (Fig. 43.15), also referred to as sacroiliac belts because of their narrow width and low positioning over the pelvis between the iliac crests and the inguinal ligaments, have been prescribed to reduce postpartum sacroiliac diastases or pubic symphysis separation. To prevent superior migration of the orthosis, groin or garter straps are often added. These are most frequently used by manual laborers. The United States National Institute for Occupational Safety and Health does not support the use of back belts as a preventive measure.46 In contrast, the United States Occupational Safety and Health Administration’s recent ergonomics regulation classified lumbar supports as personal protective equipment and suggested that they may prevent back injuries in certain settings.47 In summary, the literature in this area is inconclusive.48
MATERIALS, MANUFACTURING, AND FIT OF SPINAL ORTHOSES
Most spinal orthoses today are made principally from plastic polymers such as polyethylene and polypropylene. These polymers offer the advantages of being relatively lightweight, strong, and easy to maintain. They resist corrosion, mildew, and fatigue and have great durability. When heated, they become malleable and can be shaped. Many of the more durable and rigid thermoplastics require heating to high temperatures and therefore must be custom fitted on molds rather than directly on the patient. In these cases the orthotist will first cover the area of the body to be immobilized with plaster to create a negative mold. The next step involves building a positive mold by filling the initial negative mold with plaster. This positive mold is in turn modified to accommodate pressure-sensitive areas. The thermoplastic is then molded to the positive plaster mold. Some thermosetting plastics, such as polyester, once set, cannot be reshaped and must be altered by grinding or cutting. Orthoses are often uncomfortable to wear at the beginning and many adjustments and alterations may need to be made by the orthotist before the patient is comfortable. Fitting, both of custom and off-the-shelf orthoses, optimally should be performed in sitting, supine, and standing positions. As one would expect, custom fitting often improves compliance and results.49 Of note, computer-aided design and computer-aided manufacture (CAD-CAM), although not widely used today, may facilitate correct fit and comfort in the future by allowing more precise body contour measurements and orthotic manufacturing.
COMPLICATIONS OF ORTHOSIS USE
Pressure sores develop at areas of orthosis and skin contact. The greater the orthosis and skin contact surface area, the lower the unit pressure per area, and the lower the risk for skin breakdown. Unfortunately, due to the limited skin surface area available for contact by any particular cervical orthosis, mandibular and occipital sores are especially frequent.50 Marginal mandibular nerve palsy in which a branch of the facial nerve is compressed by a hard collar and manifested by the drooping of the lower lip with drooling has been described.51 Dysphagia and aspiration can develop due to the limitation of the normal cervical flexion which occurs during a normal swallow.
In the case of total skin contact type of orthoses, heat dissipation may become a problem and users should be instructed to wear absorptive cotton garments under the orthoses, so that perspiration does not lead to skin maceration. Excessive use of moisturizing lotions should also be avoided. Some manufactures will perforate portions of the orthoses to allow for air circulation and cooling. Fit should be snug but not tight. A cervical orthosis adjusted to provide a skin–orthosis interface pressure greater than 25 mmHg does not provide any greater immobilization of the cervical spine than a cervical orthosis adjusted to provide a skin–orthosis interface pressure of 25 mmHg. Moreover, higher interface pressures are often not tolerated, causing individuals to loosen their orthoses.52 Polyethylene foam or its equivalent may need to be added to or removed from parts of the orthosis to improve fit, and thus comfort, by eliminating pressure points and increasing skin surface contact.
SPECIFIC INDICATIONS FOR SPINAL ORTHOSES
Neck pain
Although soft collars are commonly proscribed after ‘whiplash’ injuries, there is no strong evidence in the literature that they are beneficial for this condition. In a 3-year prospective trial of 97 subjects exposed to whiplash trauma in motor vehicle collisions who were prescribed either an active intervention, which consisted of active exercises, including cervical rotation, without use of a cervical orthosis, or a standard intervention, which consisted of initial rest, soft collar use, and gradual self-mobilization, it was found that pain intensity and sick leave were significantly reduced in the group who received the active intervention.53,54 In another prospective study, 197 subjects with neck pain following motor vehicle collisions who did not have fractures, subluxations, or focal deficits were randomly assigned to use either a soft collar or no collar. No difference was found between the groups with regards to complete recovery, deterioration, or improvement in symptoms.55
Low back pain
Biomechanical studies have demonstrated that the disc is the major anterior load-bearing structure while the facet joints are the major posterior load-bearing structures.56 When in an upright standing position, facets carry 10–20% of the compressive load and more than 50% of the anterior shear load on the spine. When the spine is extended, the compressive load is transmitted through the pedicles, lamina, and articular facets. This load transmission in extension can relieve some of the load on the anterior column of the spine, including the vertebral body and intravertebral disc. Rotation combined with axial compression and flexion also appears to load the facets. In contrast, when the spine is fixed in a flexed position, the compressive load will be significantly decreased on the facets and increased on intervertebral discs, the latter leading to increased intradiscal pressures.
Clinically, lumbar positioning into either flexion or extension by an orthosis has the potential to decrease low back pain depending on the condition treated, as demonstrated in the studies described below. Gavin reported the results of a prospective study of 36 persons, who had back or leg pain for greater than 6 months, who were fitted with the test instrument of Willner, a rigid aluminum TLSO with a sagittal lumbar pad that is adjustable into lumbar flexion or extension, for a 5-day trial. For subjects with discogenic pain, including disc herniation, multiple-level disc bulging, and degenerative disc disease, the geometry of the orthosis was set in maximum extension, whereas, for subjects with spondylolisthesis, lumbar stenosis, or the pain thought to originate from the facet joints, the geometry of the orthosis was set in maximum lumbar flexion. Twenty-nine of the subjects were fitted after an acceptable trial into a TLSO in a degree of flexion or extension deemed optimal for comfort. Six of 25 subjects had recurrence of pain and underwent surgery, the remainder did not undergo surgery by 3–12 months.57
For young athletes with discogenic back pain, Micheli reported that treatment with a modified Boston brace, a TLSO which uses prefabricated thermoplastic pelvic modules designed to provide antilordotic straightening of the lumbar spine, was effective in reducing pain in only 50% of subjects. However, for 31 young athletes with spondylolysis, he reported good to excellent results in 90% using the same orthosis.58
In 1985, Willner reported on the orthotic treatment with a rigid TLSO, set in lumbar flexion, of adults with pain due to spinal stenosis with claudication, isthmic spondylolisthesis with documented slippage of 25–50% of L5–S1, or low back pain of unknown etiology with a negative myelogram and X-rays showing only spondylosis. Evaluation occurred on average after 1 year of brace use. For the subjects with spondylolisthesis, similar to the results reported by Micheli five years earlier, 13/15 had pain relief and 2/15 had pain improvement. For the subjects with stenosis, the majority, 6/7, had pain improvement or relief. For the subjects with low back pain of unknown etiology, the majority, 17/26, had no improvement.59
In 1981, Million studied 19 subjects with back pain present for greater than 6 months who also did not have any other abnormality other than lumbar spondylosis. Subjects were randomly assigned a lumbar corset with or without a spinal support. The spinal support was a heat-molded plastic insert, molded to the subjects back in the upright position, that was placed into a pocket in the back of the corset. At both 4 and 8 weeks, there was a significant relief of symptoms in only those who wore the lumbar corset with the lumbar support.60
Osteoporosis
Spinal orthoses are commonly used to treat osteoporotic compression fractures, using the biomechanical principles outlined previously, with few outcome studies available to recommend their use. However, in 2004, Pfeifer reported on a partial crossover prospective study of 62 subjects with at least one vertebral fracture and an angle of kyphosis greater than 60° resulting from osteoporosis who wore a specific orthosis for 6 months. This orthosis consisted of an abdominal pad and lightweight metal splint which was fitted along the spine and attached with Velcro straps. After 6 months of use, the subjects were found to have a 73% increase in back extensor strength, an 11% decrease in angle of kyphosis, and a 38% decrease in average pain. There was only a 3% reported drop-out rate, possibly indicating good compliance with orthosis use.61
1 Gavin TM, Patwardhan AG, Bunch WH, et al. Principles and components of spinal orthoses. In: Goldberg B, Hsu JD, editors. Atlas of orthoses and assistive devices. 3rd edn. St. Louis: Mosby; 1997:155-194.
2 Russell JN, Hendershot GE, LeClere F, et al. Trends and differential use of assistive technology devices: United States, 1994. Adv Data. 1997;13(292):1-9.
3 Harris EE. A new orthotics terminology – guide to its use for prescription and fee schedules. Orthotics Prosthetics. 1973;27:6-19.
4 White AA, Panjabe MM. Clinical biomechanics of the spine. Philadelphia: JB Lippincott, 1990.
5 Andriacchi T, et al. A model for studies of the mechanical interaction between the human spine and the ribcage. J Biomech. 1974;7:497.
6 Fielding JW. Normal and selected abnormal motion of the cervical spine from the second cervical vertebra to the seventh cervical vertebra based on cineradiography. J Bone Joint Surg. 1964;46A:1779.
7 Jones RF, Snowdon E, Coan J, et al. Bracing of thoracic and lumbar spine fractures. Paraplegia. 1987;25:386-393.
8 Harlow ML, Russ JC, Nolinske TL, et al. Orthotic management of the spine. In: Meyer PRJr, editor. Surgery of spine trauma. New York: Churchill Livingston; 1989:279-304.
9 Meyer PR. Fractures of the thoracic spine: T1–T10. In: Meyer PRJr, editor. Surgery of spine trauma. New York: Churchill Livingston; 1989:525-571.
10 Nachemson AL. Orthotic treatment for injuries and diseases of the spinal column. Phys Med Rehabil: State Art Rev. 1987;1:11-24.
11 Johnson RM, Hart DL, Simmons EF, et al. Cervical orthosis: a study comparing their effectiveness in restricting cervical motion in normal subjects. J Bone Joint Surg [Am]. 1977;59:332-339.
12 Colachis SC, Strohm BR, Ganter EL. Cervical spine motion in normal women. Arch Phys Med Rehabil. 1973;5:161-169.
13 Carter VM, Fasen JM, Roman J, et al. The effect of a soft collar, used normally recommended or reversed, on three planes of cervical range of motion. J Orthop Sports Phys Ther. 1996;23:209-215.
14 Kamenetz HL. Eponymic orthoses. In: Redford JB, editor. Orthotics etcetera. 3rd edn. Baltimore: Williams and Wilkins; 1986:803.
15 Lunsford TR, Davidson M, Lunsford BR. The effectiveness of four contemporary cervical orthoses in restricting cervical motion. J Prosthet Orthop. 1994;6:93-99.
16 Lysell E. Motion of the cervical spine [Thesis]. An experimental study on autopsy specimans. Acta Orthop Scand Suppl. 1969;123:1.
17 Maiman D, Millington P, Novack S, et al. The effect of the thermoplastic Minerva body jacket on cervical spine motion. Neurosurgery. 1989;25:363-368.
18 Ducker TB. Restriction of cervical spine motion by cervical collars [abstract]. Proceedings of 58th Annual Meeting of the American Association of Neurological Surgery, Park Ridge, IL, 1990.
19 Johnson RM, Owen JR, Callahan RA. Cervical orthoses: a guide to their selection and use. Clinical Orthop Rel Res. 1981;154:34-45.
20 Flanagan P, Gavin TM, Gavin DQ, et al. Spinal orthoses. In: Lusardi MM, Nielsen CC, editors. Orthotics and prosthetics in rehabilitation. Boston: Butterworth-Heinemann, 2000.
21 Anderson DG, Vaccaro AR, Gavin KF, et al. Spinal orthoses. In: Vaccaro AR, Betz RR, Zeidman SM, editors. Principles and practice of spine surgery. St. Louis: Mosby, 2003.
22 Edelstein JE, Bruckner J. Trunk and cervical orthoses. In: Orthotics: a comprehensive clinical approach. Thorofare: SLACK Inc.; 2002:113.
23 Askins V, Eismont FJ. Efficacy of five cervical orthoses in restricting cervical motion. A comparison study. Spine. 1997;22(11):1193-1198.
24 Gavin TM, Carandang G, Havey R, et al. Biomechanical analysis of cervical orthoses in flexion and extension: a comparison of cervical collars and cervical thoracic orthoses. J Rehabil Res Dev. 2003;40(6):527-537.
25 Koch RA, Nickel VL. The halo vest: an evaluation of motion and forces across the neck. Spine. 1978;3:103-107.
26 Lind B, Sihlbom H, Nordwell A. forces and motions across the neck in patients treated with halo-vest. Spine. 1988;13:162-167.
27 Benzel E. A comparison of the Minerva and Halo jackets for stabilization of the cervical spine. J Neurosurg. 1989;70:411-414.
28 Sharpe KP, Rao S, Ziogas A. Evaluation of the effectiveness of the Minerva cervicothoracic orthosis. Spine. 1995;81:255-257.
29 Richardson JK, Ross AM, Riley B, et al. Halos vest effects on balance. Arch Phys Med Rehabil. 2000;81:255-257.
30 Norton PL, Brown T. The immobilizing efficiency of back braces the effect on the posture and motion of the lumbosacral spine. Bone Joint Surg. 1957;39A:111-139.
31 Lantz SA, Schultz AB. Lumbar orthosis wearing. I. Restriction of gross body motions. Spine. 1986;11:834-837.
32 Cholewicki J, Juluru K, Radecold A, et al. Lumbar spine stability can be augmented with an abdominal belt and/or increased intra-abdominal pressure. Eur Spine J. 1999;8:388-395.
33 Fidler MW, Plasmans CMT. The effect of four types of support on the segmental mobility of the lumbosacral spine. J Bone Joint Surg. 1983;65A:943-947.
34 Morris JM, Lucas DB, Bressler MS. Role of the trunk in stability of the spine. J Bone Joint Surg. 1961;43A:327-351.
35 Waters RL, Morris JM. Effect of spinal supports on the electrical activity of muscles of the trunk. J Bone Joint Surg Am. 1970;52:51-60.
36 Lantz SA, Schultz AB. Lumbar spine orthosis wearing. II. Effect on trunk muscle myoelectric activity. Spine. 1986;11:838-842.
37 Nachemson A, Morris JM. In vivo measurements of intradiscal pressure. J Bone Joint Surg Am. 1964;46:1077-1092.
38 Nachemson A, Schultz A, Andersson G. Mechanical effectiveness studies of lumbar spine orthoses. Scand J Rehabil Med Suppl. 1983;9:139-149.
39 Rohlmann A, Bergmann G, Graichen F, et al. Braces do not reduce loads on internal spinal fixation devices. Clin Biomechanics. 1999;14:97-102.
40 Spratt KF, Weinstien JN, Lehmann TR, et al. Efficacy of flexion and extension treatments incorporating braces for low-back pain patients with retrodisplacement, spondylolisthesis, or normal sagittal translation. Spine. 1993;18:1839-1849.
41 Nachemson AL. Orthotic treatment for injuries and diseases of the spinal column. Phys Med Rehabil. 1987;1:22-24.
42 Williams PC. Lesions of the lumbosacral spine–lordosis brace. J Bone Joint Surg. 1937;19:702.
43 Kim SS, Denis F, Lonstein JE, et al. Factors affecting fusion rate in adult spondylolisthesis. Spine. 1990;15:979-984.
44 Vogt L, Pfeifer K, Portscher M, et al. Lumbar corsets: their effect on three-dimensional kinematics of the pelvis. J Rehabil Res Dev. 2000;37:495-499.
45 McNair PJ, Heine PJ. Trunk proprioception: enhancement through lumbar brace. Arch Phy Med Rehabil. 1999;80:96-99.
46 National Institute for Occupational Safety and Health. Workplace use of back belts. Centers for Disease Control and Prevention. Washington: US Department of Health and Hyman Services, 1992. Pub. No. 94–122
47 Occupational Safety and Health Administration. Ergonomic program: final rule. In: Federal Register 2000; 65(220)68261–870. Washington.
48 Ammendolia C, Kerr MS, Bombadier C, et al. Canadian Task Force on Preventive Health Care. Use of back belts to prevent occupational low-back pain. Recommendation statement. CMAJ. 2003;169(3):213-218.
49 Bernardoni G. Are off-the-shelf TLSOs helpful or harmful? Newsletter and Articles Ballert Orthopedics of Chicago. www.ballert-op/newsletter.
50 Davis J, Parks S, Detlef C, et al. Clearing the cervical spine in obtunded patients: The use of dynamic fluoroscopy. J Trauma. 1995;39(3):435-438.
51 Rogers J, Rogers W. Marginal mandibular nerve palsy due to compression by a cervical hard collar. J Ortho Trauma. 1994;9(2):177-179.
52 Fisher SV. Proper fitting of the cervical orthosis. Arch Phys Med Rehabil. 1978;59(11):505-507.
53 Rosenfeld M, Seferiadis A, Carlsson J, et al. Active intervention in patients with whiplash-associated disorders improves long-term prognosis: a randomized controlled clinical trial. Spine. 2003;28(22):2491-2498.
54 Rosenfeld M, Gunnarsson R, Borenstein P. Early intervention in whiplash-associated disorders: a comparison of two treatment protocols. Spine. 2000;25(14):1782-1787.
55 Gennis P, Miller L, Gallagher EJ, et al. The effect of soft cervical collars on persistent neck pain in patients with whiplash injury. Acad Emerg Med. 1996;3(6):568-573.
56 Schultz AB, Ashton-Miller JA. Biomechanics of the human spine. In: Mow VC, Hayes WC, editors. Basic orthopaedic biomechanics. New York: Raven Press, 1991.
57 Gavin TM, Boscardin JB, Patwardhan AG, et al. Preliminary results of orthotic treatment for chronic low back pain. JPO. 1993;5(1):5-9.
58 Micheli LJ, Hall JE, Miller ME. Use of modified Boston brace for back injuries in athletes. Am J Sports Med. 1980;8(5):351-356.
59 Willner S. Effect of a rigid brace on back pain. Acta Orthop Scand. 1985;56(1):40-42.
60 Million R, Nilsen KH, Jayson MI, et al. Evaluation of low back pain and assessment of lumbar corsets with and without back supports. Ann Rheum Dis. 1981;40(5):449-454.
61 Pfeifer M, Begerow B, Minne HW. Effects of a new spinal orthosis on posture, trunk strength, and quality of life in women with postmenopausal osteoporosis: a randomized trial. Am J Phys Med Rehabil. 2004;83(3):177-186.