Section 5 Spinal Injections
Spinal injection guidelines
Overview
Low back pain without disc herniation is the most common problem among chronic pain disorders, but a patho-anatomical cause can be established in only 15 % of all cases.1 Treatments to relieve this affliction have been many, among them spinal injections – engendering much controversy in the literature; opinions about efficacy, safety and relevance have differed greatly since their inception in the 1920s, with many studies considered poor quality.2–17
Although epidural injections are one of the most commonly used invasive interventions in the treatment of low back pain, with or without radicular pain, there is currently little consensus about this technique and wide variation in practice.21 There is also no agreement on the most effective approach for lumbar epidural injection, whether to use steroid, local anaesthetic, saline or a combination, or the exact volume required. Depot steroids are not licensed for spinal use18,19 but orthopaedic and pain specialists, rheumatologists and others use these injections extensively.20 The caudal route of administration may require a larger volume but is least likely to cause dural puncture.22,23
A paucity of well designed, randomized controlled studies, and a lack of statistically significant results in the existing literature mean that a solid foundation for the effectiveness of spinal injection therapy is lacking.9 NICE, the UK National Institute for Health and Clinical Excellence, recommended that patients with persistent non-specific low back pain should not be offered injections of therapeutic substances,24 but what impact this has had on clinical practice is uncertain.
A Cochrane Review found minor side-effects such as headache, dizziness, transient local pain, tingling, numbness and nausea reported in a small number of patients in only half the trials reviewed. The review concluded that there is no strong evidence for or against the use of any type of injection therapy for individuals with subacute or chronic low-back pain.10
Safety
All the contraindications listed in Section 2 apply, but particularly:
The incidence of intravascular uptake during lumbar spinal injection procedures is approximately 8.5%; it is greater in patients over 50, and if the caudal route is used rises to 11%. Absence of flashback of blood on pre-injection aspiration does not predict extravascular needle placement.31 Epidural steroid injection is safe in patients receiving aspirin-like antiplatelet medications, with no excess risk of serious haemorrhagic complications, i.e. spinal haematoma. Increased age, large needle gauge, needle approach, insertion at multiple interspaces, number of needle passes, large volume of injectant and accidental dural puncture are all relative risk factors for minor haemorrhagic complications.32
New neurological symptoms or worsening of pre-existing complaints that persist for more than 24 hours (median duration of symptoms 3 days, range 1–20 days) might occur after epidural injection,32 but in the authors’ experience this is rare.
Accuracy
Accuracy of blind caudal epidural injections compared with targeted placement has been assessed in a few studies. In one, successful placement on the first attempt occurred in three out of four subjects. Results were improved when anatomical landmarks were identified easily (88%) and no air was palpable subcutaneously over the sacrum when injected through the needle (83%). The combination of these two signs predicted a successful injection in 91% of attempts. In another study blind injections were correctly placed in only two out of three attempts, even when the operator was confident of accurate placement. When the operator was less certain, the success rate was less than half and if the patient was obese the success rate reduced even further. In a third prospective randomized, double-blind trial, the results showed no advantage of spinal endoscopic placement compared with the more traditional caudal approach.26–29,34,39
Efficacy
Lumber epidurals: a systematic review of epidural corticosteroids for back pain found at least 75% pain relief in the short term (1–60 days) with the number needed to treat (NNT) of 7 (7–16) and at least 50% pain relief in the long term (3–12 months) with NNT of 13 (7–314).3 A randomized, double-blind, controlled trial concluded that lumbar interlaminar epidural of local anaesthetic with steroid was effective in 86% of patients, and without steroid in 74%.31
A systematic review indicated positive evidence (Level II-2) for short-term relief of pain from disc herniation or radiculitis utilizing blind interlaminar epidural steroid injections; there was less strong evidence for long-term pain relief for these conditions and for the short- and long-term relief of pain from spinal stenosis and from discogenic pain without radiculitis or disc herniation.25 Another review of both caudal and lumbar epidurals also concluded that the best studies showed inconsistent results and benefits were of short duration only.6 Yet another showed strong evidence for epidurals in the management of nerve root pain due to disc prolapse, but limited evidence in spinal stenosis.22 A multicentre randomized controlled trial of epidurals for sciatica reported significant relief at 3 weeks but no long-term benefit.14
In the past, large volumes have been injected into the epidural space;33 however, a total injection volume of 8 ml is sufficient for a caudal epidural injection to reach the L4/5 level.34
Selective guided nerve-root injections of corticosteroids are significantly more effective than those of bupivacaine alone in obviating the need for operative decompression for 13–28 months following the injections in operative candidates. This finding suggests that patients who have lumbar radicular pain at one or two levels should be considered for treatment with selective nerve-root injections of corticosteroids prior to operative intervention. A significantly greater proportion of patients treated with transforaminal injection of steroid achieve relief of pain compared with those treated by transforaminal injection of local anesthetic or saline or intramuscular steroids.30 When symptoms have been present for more than 12 months, local anaesthetic alone may be just as effective as steroid and local anaesthetic together.
When conservative measures fail, nerve-root injections are effective in reducing radicular pain in patients with osteoporotic vertebral fractures and no evidence of nerve root palsy. These patients may be considered for this treatment before percutaneous vertebroplasty or operative intervention is attempted.35,36,38
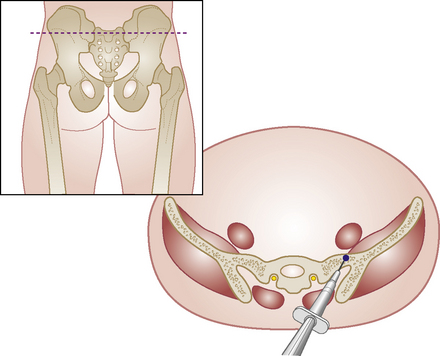
Injection of the sacroiliac joints for painful sacroiliitis appears to be safe and effective. It can be considered in patients with contraindications or complications with NSAIDs, or if other medical treatment is ineffective,37 though often manipulative techniques can obviate the need for an injection. However, accurate placement of the drug without the use of fluoroscopy is estimated to be successful in only 12 % of patients.40
Indications for spinal injection
The following are the main indications for caudal and nerve root injections:
Older patients with chronic back pain and stiffness increased on active extension may benefit from facet joint injections. A retrospective study of patients with spinal stenosis found that 35 % of patients had at least 50 % improvement; those with spondylolisthesis, single level stenosis and older than 73 had better outcomes.28 Less commonly, injections for coccydinia or sacroiliac joint pain can be attempted in cases of acute traumatic or post-natal pain.
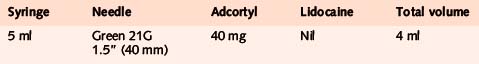
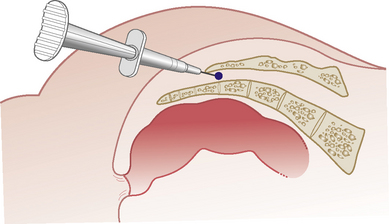
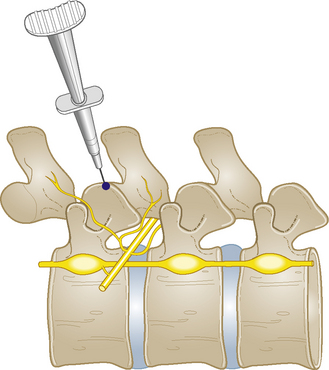
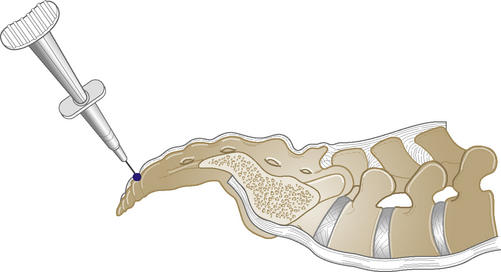
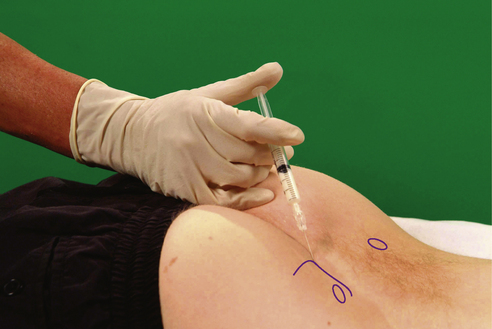
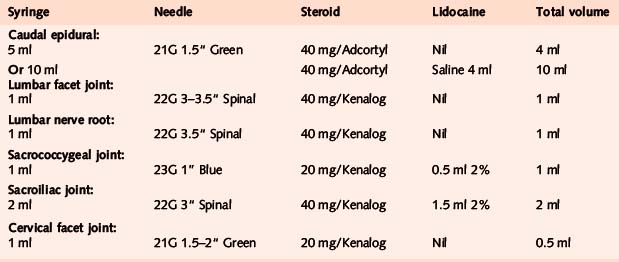
Caudal epidural
Acute or chronic low back pain or sciatica
Alternative approach
If the affected level is higher than the common L5/S1 level or the patient is large, more volume may be required to reach these levels. In this case we recommend the addition of up to 10 ml of normal saline, depending on the level of the lesion and the size of the patient.39
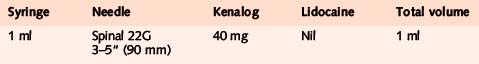
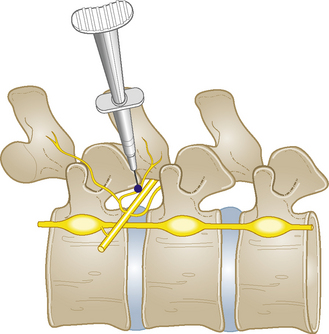
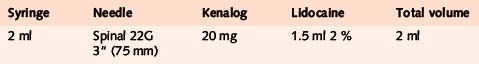
Lumbar facet joint
Chronic capsulitis
Comments
Sometimes it is impossible to enter the joint, but controlled studies have shown that depositing the solution into the capsule can be therapeutically effective11.
Sacrococcygeal joint
Sacroiliac joint
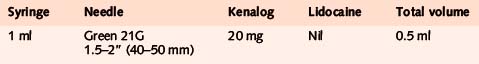
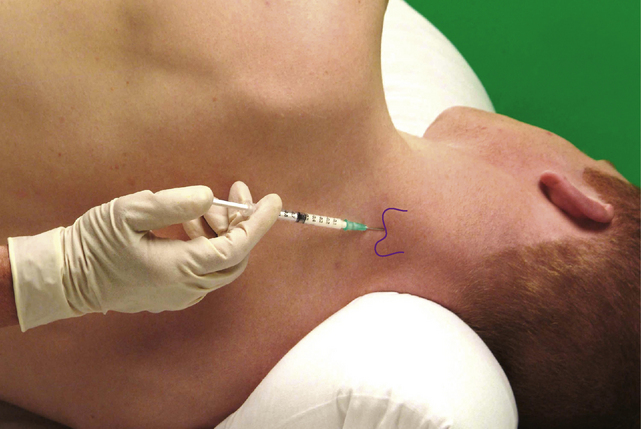
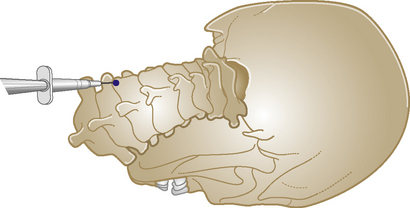
Cervical facet joint
1. Manchikanti L., Cash K.A., McManus C.D., et al. Preliminary results of randomized double-blind controlled trial of fluoroscopic lumbar interlaminar epidural injections in managing chronic lumbar discogenic pain without disc herniation or radiculitis. Pain Physician. 2010;13(4):E279-E292.
2. Watts R.W., Silagy C.A. A meta-analysis on the efficacy of epidural corticosteroids in the treatment of sciatica. Anaesth Intensive Care. 1995;23:564-569.
3. McQuay H.J., Moore R.A. Epidural steroids for sciatica. Anaesth Intensive Care. 1996;24:284-285. (letter)
4. Samanta A., Beardsley J. Sciatica: which intervention? Br Med J. 1999;319:302-303.
5. Bush K., Hillier S. A controlled study of caudal epidural injections of triamcinolone plus procaine for the management of intractable sciatica. Spine. 1991;16(5):572-575.
6. Koes B., Scholten R., Mens J., et al. Efficacy of epidural steroid injections for low back pain and sciatica: a systematic review of randomised clinical trials. Pain. 1995;63:279-288.
7. Carette S., Leclaire R., Marcoux S., et al. Epidural corticosteroid injections for sciatica due to herniated nucleus pulposus. N Engl J Med. 1997;336(23):1634-1640.
8. Slosar P., White A.H. Controversy – the use of selective nerve root blocks: diagnostic, therapeutic or placebo? Spine. 1998;20:2253-2256.
9. Riew K.D., Yin Y., Gilula L., et al. The effect of nerve root injections on the need for operative treatment of lumbar radicular pain. A prospective, randomised, controlled, double blind study. J Bone Joint Surg Am. 2000;82:1589-1593.
10. Staal J.B., de Bie R., de Vet H.C.W., et al. Injection therapy for subacute and chronic low-back pain. Cochrane Database Syst Rev. (3):2008. Art. No.: CD001824. DOI:10.1002/14651858.CD001824.pub3
11. Carette S., Marcoux S., Truchon R., et al. A controlled trial of corticosteroid injections into facet joints for chronic low back pain. N Engl J Med. 1991;325(14):1002-1007.
12. Jackson D.W., Rettig A.C., Wiltse L.L. Epidural cortisone injections in the young athletic adult. Am J Sports Med. 1980;8(4):239-243.
13. Valat J.-P., Giraudeau B., Rozenburg S., et al. Epidural corticosteroid injections for sciatica: a randomised, double blind, controlled clinical trial. Ann Rheum Dis. 2003;62:639-643.
14. Arden N.K., Price C., Reading I., et al. A multicentre randomized controlled trial of epidural corticosteroid injections for sciatica: the WEST study. Rheumatology. 2005;44(11):1399-1406.
15. Buttermann G.R. Treatment of lumbar disc herniation: epidural steroid injection compared with discectomy; a prospective, randomized study. J Bone Joint Surg Am. 2004;86:670-679.
16. van Tulder M., Koes B. Low back pain and sciatica (acute and chronic). London: BMJ Books. 2004:286-291. Clinical Evidence Concise No. 11
17. Samanta A., Samanta J. Is epidural injection of steroids effective for low back pain? Br Med J. 2004;328:1509-1510.
18. Ferner R.E. Prescribing licensed medicines for unlicensed indications. Prescribers J. 1996;36(2):73-78.
19. Wildsmith J.A. Routes of drug administration: 6. Intrathecal and epidural injection. Prescribers J. 1996;36(2):110-115.
20. Fanciullo G.J., Hanscom B., Seville J., et al. An observational study of the frequency and pattern of use of epidural steroid injection in 25,479 patients with spinal and radicular pain. Reg Anesth Pain Med. 2001;26(1):5-11.
21. Cluff R., Mehio A.K., Cohen S.P., et al. The technical aspects of epidural steroid injections: a national survey. Anesth Analg. 2002;95:403-408.
22. Abi S., Datt S., Lucas L. Role of epidural steroids in management of chronic spinal pain: Systematic review of effectiveness and complications. Pain Physician. 2005;8(1):127-143.
23. Snarr J. Risks, benefits and complications of epidural steroid injections: case report. AANA J. 2007;75(3):183-188.
24. National Collaborating Centre for Primary Care. Low back pain: early management of persistent non-specific low back pain. 2009. (NICE Guideline CG88). May 2009
25. Conn A., Buenaventura R.M., Datta S., et al. Systematic review of caudal epidural injections in the management of chronic low back pain. Pain Physician. 2009;12:109-135.
26. Price C.M., Roger P.D., Prosser A.S.J., et al. Comparison of the caudal and lumbar approaches to the epidural space. Ann Rheum Dis. 2000;59(11):879-882.
27. Stitz M.Y., Sommer H.M. Accuracy of blind versus fluoroscopically guided caudal epidural injection. Spine. 1999;24(13):1371.
28. Barre L., Lutz G.E., Southern D., et al. Fluoroscopically guided caudal epidurals for lumbar/spinal stenosis. Pain Physician. 2004;7(2):187-193.
29. Botwin K., Brown L.A., Fishman M., et al. Fluoroscopically guided caudal epidural injections in degenerative lumbar spinal stenosis. Pain Physician. 2007;10(4):547-548.
30. Ghahreman A., Ferch R., Bogduk N. The efficacy of transforaminal injection of steroids for the treatment of lumbar radicular pain. Pain Med. 2010;11(8):1149-1168.
31. Manchikanti M., Singh V., Falco F.J.E., et al. Evaluation of effectiveness of lumbar interlaminar epidural injections in managing chronic pain of lumbar disc herniation of radiculitis: a randomized double-blind controlled trial. Pain Physician. 2010;13:343-355.
32. Horlocker T., Zahid H., Bajwa Z.H., et al. Risk assessment of hemorrhagic complications associated with non-steroidal anti-inflammatory medications in ambulatory pain clinic patients undergoing epidural steroid injection. Anesth Analg. 2002;95:1691-1697.
33. Cyriax J. Epidural injection. Textbook of Orthopaedic Medicine, 2. London: Bailliére Tindall. 1984:178.
34. Bryan B.M., Lutz C., Lutz G.E. Fluoroscopic assessment of epidural contrast spread after caudal injection. Journal of Orthopaedic Medicine. 2000;22(2):38-41.
35. Riew K., Yuming Y., Gilula L., et al. Effect of nerve root injections on the need for operative treatment of lumbar radicular pain. A prospective, randomised, controlled, double blind study. J Bone Joint Surg Am. 2000;82:1589-1593.
36. Ng L.C., Sell P. Outcomes of a prospective cohort study on peri-radicular infiltration for radicular pain in patients with lumbar disc herniation and spinal stenosis. Eur Spine J. 2004;13(4):325-329.
37. Maugars Y., et al. Assessment of the efficacy of sacroiliac corticosteroid injections in spondylarthropathies: a double-blind study. Br J Rheumatol. 1996;35:767-770.
38. Kim D., Yun Y., Wang J. Nerve-root injections for the relief of pain in patients with osteoporotic vertebral fractures. J Bone Joint Surg Br. 2003;85(2):250-254.
39. Dashfield K., Taylor M., Clekven J., et al. Comparison of caudal steroid epidural with targeted steroid placement during spinal endoscopy for chronic sciatica; a prospective randomized, double-blind trial. Br J Anaesth. 2005;94(4):514-516.
40. Hansen H. Is fluoroscopy necessary for sacroiliac injections? Pain Physician. 2003;6:155-158.
41. Jones D.S., Chattopadhyay C. Suprascapular nerve block for the treatment of frozen shoulder in primary case: a randomised trial. Br J Gen Pract. 1999;49:39-41.
42. Jackson D., Evans N., Thomas B. Accuracy of needle placement in the intra-articular space of the knee. J Bone Joint Surg Am. 2002;84:1522-1527.