Chapter 8 Spinal Cord Stimulation as a Treatment of Failed Back Surgery Syndrome
 SCS is a minimally invasive, reversible, cost-effective treatment that can reduce the pain associated with FBSS in carefully selected patients.
SCS is a minimally invasive, reversible, cost-effective treatment that can reduce the pain associated with FBSS in carefully selected patients. A screening trial mimics the therapeutic effect of SCS and thus predicts the results of system implantation.
A screening trial mimics the therapeutic effect of SCS and thus predicts the results of system implantation. Modern SCS systems provide a myriad of programming options. Rechargeable batteries can reduce patient risk associated with battery replacement and improve cost-effectiveness.
Modern SCS systems provide a myriad of programming options. Rechargeable batteries can reduce patient risk associated with battery replacement and improve cost-effectiveness. An examination of recent imaging studies (an MRI or CT myelogram) before a patient undergoes any SCS procedure will provide information about the depth of dorsal cerebrospinal fluid and the position of the spinal cord and allow the surgeon to optimize electrode selection, placement, and adjustment.
An examination of recent imaging studies (an MRI or CT myelogram) before a patient undergoes any SCS procedure will provide information about the depth of dorsal cerebrospinal fluid and the position of the spinal cord and allow the surgeon to optimize electrode selection, placement, and adjustment. Applying silicone elastomer adhesive during electrode anchoring can prevent longitudinal electrode migration. (This is not necessary or possible with some anchors and techniques, and alternatives are under development.) During system implantation, decrease mechanical stress by avoiding unnecessary bends of small radius and superfluous connectors and by not crossing a mobile joint or body segment with subcutaneous lead wire or extension cable.
Applying silicone elastomer adhesive during electrode anchoring can prevent longitudinal electrode migration. (This is not necessary or possible with some anchors and techniques, and alternatives are under development.) During system implantation, decrease mechanical stress by avoiding unnecessary bends of small radius and superfluous connectors and by not crossing a mobile joint or body segment with subcutaneous lead wire or extension cable.Introduction
By 1985, investigators recognized that FBSS is an important public health problem affecting 25,000 to 50,000 new patients each year.1 Many causes have been implicated for the development of FBSS, including inappropriate patient selection criteria for lumbosacral surgical procedures, shortfalls in the surgeon’s diagnostic or technical skills (operation not indicated, wrong site, incomplete decompression, and/or fusion),2 and inadequacies in available surgical techniques.
Electrical stimulation with implanted devices followed the 1965 publication of Melzack and Wall’s gate control theory of pain3 and the development of cardiac pacemaker technology. Today SCS is delivered with sophisticated techniques that take advantage of multichannel pulse generators powered by rechargeable batteries.
Establishing Diagnosis
The assessment of an FBSS patient should be multifaceted and should follow the same procedure used for any chronic pain syndrome. Review of the patient’s history and operative record (which should be sought routinely) helps to establish the underlying diagnosis. The presence of any issues of secondary gain, psychological or behavioral problems, or co-morbid pain conditions is of interest. A thorough pertinent physical examination helps to corroborate the diagnosis. A validated numeric rating or visual analog scale (VAS) can help to determine the intensity of the pain and follow the patient’s progress.4 Imaging studies provide valuable information that will guide treatment. Abnormalities revealed by imaging studies and the physical examination should be consistent with the patient’s pain. The patient might demonstrate nonorganic responses (Waddell signs) during the physical examination,5 but organic findings should predominate.
Specific prognostic factors have been identified for patients with FBSS concerning the likelihood that they might benefit from SCS. For example, the extent to which the patient’s pain is radicular is important (relieving axial low back pain with SCS is technically more difficult than relieving radicular pain).6,7 Technological advances, however, continue to permit clinicians to improve outcomes and extend the circumstances in which SCS is indicated for FBBS.
Anatomy
FBSS often occurs because a surgeon has assumed that a patient’s pain was caused by an anatomical abnormality that could be corrected with a surgical procedure. The same or similar anatomical abnormalities, however, might occur in asymptomatic individuals.8 Indeed, in consecutive patients with FBSS, Long and associates2 reported that most did not meet standard indications for their first surgical procedure. Treatment of FBSS with a repeat surgical procedure remains indicated, however, if a patient has a large disc fragment or severe stenosis compressing a nerve or nerves and causing a significant neurologic deficit or if there is gross spinal instability.
Computer modeling of the electrical fields produced by SCS in the spinal cord9,10 revealed current and voltage distributions consistent with those found in studies of cadavers and primate spinal cords. The modeling studies have predicted that bipolar stimulation with closely spaced electrical contacts separated by 6 to 8 mm or less would be the best way to target longitudinal midline fibers and that the electrical field between two cathodes bracketing the physiological midline does not sum constructively in the midline.11 Modeling has also predicted advantages for three or more columns of contacts with lateral anodes.12 Clinical experience has confirmed that correct positioning and spacing of SCS electrodes is essential for pain relief.13 The longitudinal position of an electrode largely determines the segmental effects of stimulation; and rather than being beneficial, positioning electrodes more cephalad than the target area commonly elicits unwanted local segmental effects.14
Basic Science
In experimental studies SCS suppressed long-term potentiation of WDR neurons by reducing the C-fiber response15 and also changed the concentration of several neurotransmitters and their metabolites in CSF, including serotonin and substance P,16 glycine, adenosine, and noradrenaline.17,18 Supraspinal microdialysis in conscious rats revealed that SCS causes γ-aminobutyric acid (GABA) release in periaqueductal grey matter.19 SCS also induces GABA release in the dorsal horn20 (activation of the GABA-B receptor might be responsible for the therapeutic effect of SCS) and decreases the release of glutamate and aspartate.21 It is likely that SCS has additional, complicated effects on as-yet-unidentified neural transmitters and modulators. SCS is not thought to affect opioid receptor-mediated analgesia because naloxone does not inhibit SCS efficacy.22
In patients undergoing successful SCS treatment to reduce otherwise intractable neuropathic leg pain, positron emission tomography (PET) studies suggest that SCS also modulates supraspinal neurons.23 In these patients SCS increased cerebral blood flow significantly in the thalamus contralateral to the painful leg and in the associated bilateral parietal area, and this was associated with changes in pain threshold. SCS also activated the anterior cingulate cortex and prefrontal areas, which control the emotional response to pain.
Imaging
Imaging studies undertaken to establish the diagnosis of FBSS provide information about the patient’s postsurgical anatomy and whether or not the anatomic goals of the surgical procedure were met. This might explain the failure of the surgical procedure to relieve pain; however, established nerve injury can lead to persistent pain, even after technically successful surgery (Table 8-1). Radiographic imaging studies should reveal abnormalities concordant with the patient’s current pain complaints (see Table 8-1).
Table 8-1 Uses of Imaging Technology in Spinal Cord Stimulation Treatment
| Type | Timing | Purpose |
|---|---|---|
| MRI or CT myelogram of lumbar spine | Before SCS screening trial | Establish diagnosis of FBSS. |
| Reveal postsurgical anatomy. | ||
| Were goals of surgery met? | ||
| Are abnormalities consistent with current pain complaint? | ||
| MRI or CT myelogram of thoracic spine | Before SCS screening trial | Rule out pathology contributing to symptoms. |
| Rule out pathology that would compromise electrode placement. | ||
| Aid in planning electrode placement. | ||
| Fluoroscopy | During SCS procedure | Guide electrode placement. |
| Fluoroscopy or x-ray | After SCS procedure | Document electrode placement. |
| X-ray | Diagnosis of cause of complication | Electrode migration or fracture is possible. |
CT, Computed tomography; FBSS, failed back surgery syndrome; MRI, magnetic resonance imaging; SCS, spinal cord stimulation.
Imaging is also used to guide SCS treatment (see Table 8-1). For example, imaging the thoracic spine provides valuable information about the placement of thoracic electrodes. Imaging should take place before the procedure to rule out any pathological condition that might contribute to the patient’s pain or confound (or increase the risk of) electrode placement (e.g., stenosis). Fluoroscopic imaging during the procedure helps guide placement of the electrode and documents the final electrode position. Imaging is also used to diagnose the cause of a complication such as suspected electrode migration or fracture.
Guidelines
Many guidelines are published for medical therapies, invoking principles of evidence-based medicine (EBM). Ironically, to date little evidence exists that EBM or guidelines have improved patient care. We have published a set of practice parameters as a reference for referring physicians, clinicians offering SCS treatment, and patients.24
Indications/Contraindications
Relative contraindications to SCS include unresolved issues of secondary gain (e.g., an outstanding lawsuit or compensation claim), a major untreated psychiatric co-morbidity, and/or inappropriate medication use. The presence of a demand cardiac pacemaker requires electrocardiogram (ECG) monitoring and/or changing the pacemaker mode to a fixed rate.25
Equipment
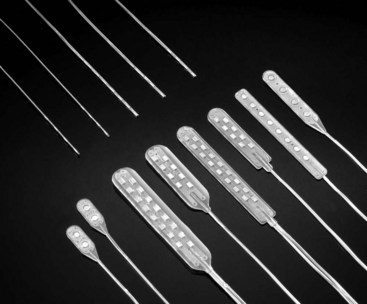
Equipment needed for the SCS screening trial (see following paragraphs) includes an electrode that will be connected to an external pulse generator and external programming equipment. A complete SCS system for chronic use requires at least one electrode (Fig. 8-1) with an extension cable and an implantable pulse generator (IPG) (Fig. 8-2).
Placement of plate/paddle electrodes requires surgical exposure of the epidural space. Plate/paddle electrodes have dorsal insulation to protect against excess posterior stimulation, and they offer better performance than do percutaneous electrodes in FBSS patients.26,27 They are available in one-, two-, three-, and five-column configurations. Compared with percutaneous electrodes, plate/paddle electrodes require only half the battery power.28 They require open (albeit minimal) exposure; this limits longitudinal mapping. They are more difficult to revise, remove, or replace, once encapsulated in scar tissue; however, this makes them inherently more resistant to migration.
Each type of electrode has multiple electrical contacts that can be configured in a multitude of ways (various combinations of anode/cathode/off/on). The SCS programming options are so numerous that it is impossible to test every combination (e.g., a four-contact electrode has 50 functional bipolar combinations of anodes and cathodes, an eight-contact electrode has 6050). Computerized methods are useful in finding and recording options for an individual patient.29 Typical stimulation parameters are set at 60 Hz frequency (pulse repetition rate) with 0.2- to 1-msec pulse width. Amplitude should be adjusted to the minimum level, on a scale from perceptual to discomfort (or motor) threshold that elicits adequate coverage of the area(s) of pain by paresthesia.
The longitudinal position of the electrode determines which segment of the body will experience paresthesia, and bipolar (or tripolar) stimulation has the greatest selectivity for longitudinal midline fibers.13 FBSS patients with associated axial low back pain require low thoracic electrode placement and sometimes need complex electrode arrays.
As shown in Fig. 8-2, the stimulator energy sources in use are: (1) radiofrequency-coupled passive implants that have a long life but require an external antenna, which can cause skin irritation and fluctuations in stimulation amplitude; (2) primary cell IPGs that require replacement at the end of battery life; and (3) IPGs with rechargeable batteries. Patients can turn IPGs on and off and use either an external magnet to make limited adjustments in amplitude or a remote transmitter capable of complicated adjustments.
Technique
The technical goal of SCS for FBSS is to cover the area of pain with a tingling sensation known as paresthesia (Table 8-2). Pain/paresthesia overlap is necessary (but not sufficient) to achieve pain relief. The paresthesia must be comfortable, and the stimulation must not cause a motor reaction. If pain/paresthesia overlap only occurs with uncomfortable stimulation (i.e., outside of the [often narrow] “usage range” between perception of paresthesia and discomfort or motor effects), treatment is compromised. In addition, the perception of extraneous stimulation paresthesia outside the area(s) of pain should be minimized.
Table 8-2 Positive Outcomes of Spinal Cord Stimulation Treatment
| Desired outcome | Goal | Requirements |
|---|---|---|
| Technical | Overlap pain with comfortable paresthesia Minimize extraneous paresthesia No motor effects |
Well-trained implanter Correct longitudinal, left-right, and dorsal-ventral position of electrode Correct stimulation parameters (pulse amplitude, width, and repetition rate) Correct contact combination (anode/cathode/off) Appropriate use of plate/paddle electrode |
| Clinical | ≈50% relief of baseline pain | Well-trained implanter Proper patient selection Use of appropriate equipment Equipment implanted and adjusted optimally |
| Potential benefits | Decrease or eliminate pain medication Improve physical functioning and ability to engage in activities of daily life Enhance quality of life Return to work Improve emotional state |
Factors beyond successful spinal cord stimulation therapy |
Percutaneous Catheter Electrode Implantation
After removing the needle, pass the anchoring sleeve/strain relief through the dorsal fascia and tie it with one suture before injecting a small amount (<0.1 ml) of silicone elastomer adhesive between the inner surface of the sleeve and the outer surface of the lead. This virtually eliminates electrode migration.30 Add ligatures around the anchor as appropriate and secure the sleeve flat against the dorsal fascia with the most caudal anchoring suture. Finally, confirm the position of the electrode under fluoroscopy.
Patient Management/Evaluation
If SCS pain relief disappears, it is important to determine first if the system is operating correctly. Sometimes fibrosis around implanted electrodes increases impedance and interferes with treatment; this generally can be overcome through reprogramming. A minority of SCS patients experience clinical failure, which is the unexplained loss of pain relief despite a functioning system that continues to provide appropriate pain/paresthesia overlap. When this occurs, SCS can sometimes be potentiated with adjuvant medication.31
Outcomes Evidence
Patient-rated pain relief is the usual primary outcome criterion for SCS and for pain treatments in general, with success commonly defined as a minimum 50% relief (see Table 8-2). Secondary outcome measures include ability to conduct activities of daily living, work status, medication requirements, neurological function, and patient satisfaction with the procedure. To reduce bias in SCS studies, collection of follow-up data by a disinterested third party is desirable. Since SCS elicits paresthesia, blinding is not feasible; thus any randomized controlled trial (RCT) of SCS loses points on rating scales commonly used in EBM.
Two decades ago we compared retrospective data in FBSS patients who underwent reoperation32 with those who received SCS and found that SCS patients enjoyed reduced morbidity and pain and improved neurological function, quality of life, and ability to engage in activities of daily living.6,33
In the first RCT of SCS vs. reoperation in FBSS patients,34 45 subjects (90% of those who received insurance authorization for study participation) were available for a mean follow-up of 3 years. SCS success was 9 of 19, whereas reoperation success was 3 of 26. Only 5 of the 24 subjects randomized to SCS crossed to reoperation, whereas 14 of the 26 randomized to reoperation crossed to SCS. No patient who crossed from SCS to reoperation achieved success with reoperation, but 6 of the 14 who crossed from reoperation to SCS achieved success with SCS. Success was defined as at least 50% pain relief and patient satisfaction with treatment.
An international multicenter RCT (the PROCESS study)35 randomized 100 subjects with FBSS to conventional medical management (CMM) or SCS plus CMM. By 6 months the subjects randomized to SCS achieved significantly greater pain relief and improved functional capacity and health-related quality of life than did those randomized to CMM. The investigators followed the 42 subjects randomized to SCS who actually received SCS for 24 months and found significantly improved leg pain relief, functional capacity, and quality of life compared with baseline scores.36 At the time the randomized group reached 24 months’ follow-up, 72 patients had received SCS as a final treatment, through either randomization or cross over. Of these, 34 (47%) achieved the primary outcome (more than or equal to 50% pain relief) vs. 1 of 15 patients who received only CMM.
The initial cost of an SCS system is high. Nevertheless, several cost-effectiveness analyses have demonstrated that SCS treatment lowers the total cost of health care for patients with neuropathic pain compared with alternative treatments. In a cost study based on data from the first 40/42 (of 50) patients enrolled in the RCT of SCS vs. reoperation,34 every analysis (intention-to-treat, treated-as-intended with cross over counted as failure of randomized treatment, and final treatment) showed that SCS achieved economic dominance by being more effective and less expensive than reoperation.37
In 2008 the National Institute for Health and Clinical Excellence (NICE) in the United Kingdom conducted a systematic review and technology assessment of the use of SCS.38 The model, which compared the cost of treating FBSS with SCS vs. CMM and reoperation and assumed an IPG battery life of 4 years, predicted that SCS would produce additional quality-adjusted life years at a cost the United Kingdom health service would be willing to pay.
Technical Aspects of Spinal Cord Stimulation
Beginning in 1986 we developed and used a patient-interactive computer program to allow patients to find the parameter settings that would optimize pain/paresthesia overlap and battery life and as a means of conducting blinded RCTs comparing electrode designs.39 In one study, we compared results with a four-contact percutaneous electrode vs. a four-contact surgical plate/paddle electrode and found that the plate/paddle electrode provided the best pain/paresthesia coverage, low back coverage, and battery longevity.28 At mean follow-up of 1.9 years, compared with patients with percutaneous electrodes, twice as many patients with plate/paddle electrodes reported a successful outcome (at least 50% sustained relief of pain and patient satisfaction) and a reduction or elimination of pain medication.26 A statistically significant advantage for the plate/paddle electrode disappeared, however, at longer follow-up in our small sample of 24 patients.
To determine if use of two percutaneous electrodes bracketing the physiological midline would enhance paresthesia coverage of the low back, we tested parallel percutaneous electrodes bracketing the midline (for chronic use) vs. a single percutaneous electrode placed on the midline for temporary use during the screening trial.40 The single electrode provided the best pain/paresthesia overlap at the lowest amplitude requirement. Nevertheless, 53% of the patients reported success at 2.3-year mean follow-up with the parallel percutaneous electrodes.
Next we compared results of treating axial low back pain using a four-contact percutaneous electrode with those obtained using a surgical plate/paddle electrode with two parallel rows of eight contacts (16 total).41 The percutaneous electrode provided marginally better pain/paresthesia overlap with significantly improved symmetry using significantly lower voltage. Compared with the surgical plate/paddle electrode, however, the percutaneous electrode required a slightly higher scaled amplitude to cover the low back and produced significantly increased extraneous coverage.
Our findings indicate that an electrode array comprising dual columns of contacts bracketing the midline presents disadvantages that might be overcome if a third column is placed on the midline. Indeed, a computer model developed at the University of Twente predicts the effect of such electrode configurations on the stimulation of dorsal column and root fibers.42 Both a longitudinal tripole electrode and a transverse tripole (each with a central cathode) reportedly have advantages in selectively recruiting the presumed stimulation target neurons.12
Reducing Risks and Avoiding Complications
SCS implantation can lead to spinal cord or nerve injury, dural puncture causing CSF leakage, hematoma, or infection (Table 8-3). To avoid spinal cord or nerve injury, it is helpful to obtain an MRI or computed tomography (CT) myelogram of the target area before placing an electrode. To avoid dural puncture, the patient should be conscious during the procedure; and, if possible, electrodes should not be placed in scarred areas. A standard preoperative coagulation profile should be undertaken to help avoid hematoma, and the patient should be monitored overnight. Standard precautions should be taken to avoid infection.
Table 8-3 Reducing the Risk of Spinal Cord Stimulation Complications
| Potential Adverse Outcomes | Risk Reduction |
|---|---|
| Spinal cord or nerve injury | Image (MRI, CT myelogram) target area before electrode placement. |
| Patient is conscious during procedure. | |
| Dural puncture (CSF leak) | Avoid placing electrodes in area with scarring. |
| Patient is conscious during procedure. | |
| Hematoma | Perform preoperative review of coagulation history. |
| Monitor patient overnight. | |
| Infection | Prophylactic antibiotics |
| Standard sterile precautions | |
| Generator failure | Train patient in proper system use. |
| Consider IPGs with rechargeable batteries. | |
| Lead fatigue fracture | Avoid unnecessary extension cables and connectors. |
| Position service loops to relieve strain. | |
| Avoid crossing mobile body segments. | |
| Electrode migration | “Glue” lead anchor to lead. |
| Disturbance from exposure to electromagnetic field | Educate patient to avoid exposure. |
CSF, Cerebrospinal fluid; CT, computed tomography; IPG, implantable pulse generator; MRI, magnetic resonance imaging.
Equipment-related complications include generator failure, electrode fatigue fracture, electrode migration, and disturbance from exposure to an electromagnetic field (see Table 8-3). Generators can fail, but the incidence of battery failure can be reduced by helping the patient learn to use the system properly and by implanting rechargeable batteries. Lead fatigue failure can be reduced by minimizing the use of connectors, positioning service loops to relieve strain, avoiding crossing mobile body segments, and placing the generator in the patient’s flank or lateral abdomen. Fixing the electrode in place properly virtually eliminates migration.30
1 Heithoff KB, Burton CV. CT evaluation of the failed back surgery syndrome. Orthop Clin North Am. 1985;16:417-444.
2 Long DM, et al. Clinical features of the failed-back syndrome. J Neurosurg. 1988;69:61-71.
3 Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;150:971-978.
4 Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27:117-126.
5 Waddell G, et al. Nonorganic physical signs in low back pain. Spine. 1980;5:117-125.
6 North RB, et al. Spinal cord stimulation for chronic, intractable pain: experience over two decades. Neurosurgery. 1993;32:384-394.
7 Burchiel KJ, et al. Prospective, multicenter study of spinal cord stimulation for relief of chronic back and extremity pain. Spine. 1996;21:2786-2794.
8 Tong HC, et al. Magnetic resonance imaging of the lumbar spine in asymptomatic older adults. J Back Musculoskeletal Rehab. 2006;19:67-72.
9 Coburn B, Sin W. A theoretical study of epidural electrical stimulation of the spinal cord. I. Finite element analysis of stimulus fields. IEEE Trans Biomed Eng. 1985;32:971-977.
10 Holsheimer J, Strujik JJ, Rijkhoff NJM. Contact combinations in epidural spinal cord stimulation: a comparison by computer modeling. Stereotact Funct Neurosurg. 1991;56:220-233.
11 Holsheimer J, Wesselink WA. Effect of anode-cathode configuration on paresthesia coverage in spinal cord stimulation. Neurosurgery. 1997;41:654-659.
12 Struijk JJ, et al. Theoretical performance and clinical evaluation of transverse tripolar spinal cord stimulation. IEEE Trans Rehabil Eng. 1998;6:277-285.
13 Barolat G, et al. Mapping of sensory responses to epidural stimulation of the intraspinal neural structures in man. J Neurosurg. 1993;78:233-239.
14 Law J. Spinal stimulation: Statistical superiority of monophasic stimulation of narrowly separated bipoles having rostral cathodes. Appl Neurophysiol. 1983;46:129-137.
15 Wallin J, et al. Spinal cord stimulation inhibits long-term potentiation of spinal wide dynamic range neurons. Brain Res. 2003;973:39-43.
16 Linderoth B, et al. Dorsal column stimulation induces release of serotonin and substance P in the cat dorsal horn. Neurosurgery. 1992;31:289-296.
17 Meyerson BA, Brodin E, Linderoth B. Possible neurohumoral mechanisms in CNS stimulation for pain suppression. Appl Neurophysiol. 1985;48:175-180.
18 Cui JG, et al. Adenosine receptor activation suppresses tactile hypersensitivity and potentiates spinal cord stimulation in mononeuropathic rats. Neurosci Lett. 1997;223:173-176.
19 Linderoth B, et al. An animal model for the study of brain transmitter release in response to spinal cord stimulation in the awake, freely moving rat: Preliminary results from the periaqueductal grey matter. Acta Neurochir(Wien). 1993;58(suppl):156-160.
20 Stiller CO, et al. Release of gamma-aminobutyric acid in the dorsal horn and suppression of tactile allodynia by spinal cord stimulation in mononeuropathic rats. Neurosurgery. 1996;39:367-374.
21 Cui JG, et al. Spinal cord stimulation attenuates augmented dorsal horn release of excitatory amino acids in mononeuropathy via a GABAergic mechanism. Pain. 1997;73:87-95.
22 Freeman TB, Campbell JN, Long DM. Naloxone does not affect pain relief induced by electrical stimulation in man. Pain. 1983;17:189-195.
23 Kishima H, et al. Modulation of neuronal activity after spinal cord stimulation for neuropathic pain; H(2)15O PET study. Neuroimage. 2010;49:2564-2569.
24 North RB, Shipley J. Practice parameters for the use of spinal cord stimulation in the treatment of neuropathic pain. Pain Med. 2007;8(S4):S200-S275.
25 Ekre O, et al. Feasibility of spinal cord stimulation in angina pectoris in patients with chronic pacemaker treatment for cardiac arrhythmias. Pacing Clin Electrophysiol. 2003;26:2134-2141.
26 North RB, et al. Spinal cord stimulation electrode design: s prospective, randomized, controlled trial comparing percutaneous with laminectomy electrodes. Part II. Clinical outcomes. Neurosurgery. 2005;57:990-995.
27 Villavicencio AT, et al. Laminectomy versus percutaneous electrode placement for spinal cord stimulation. Neurosurgery. 2000;46:399-405.
28 North RB, et al. Spinal cord stimulation electrode design: a prospective, randomized, controlled trial comparing percutaneous and laminectomy electrodes. Part I. Technical outcomes. Neurosurgery. 2002;51:381-389.
29 North RB, et al. Patient-interactive, computer-controlled neurological stimulation system: clinical efficacy in spinal cord stimulator adjustment. J Neurosurg. 1992;76:967-972.
30 Renard VM, North RB. Prevention of percutaneous electrode migration in spinal cord stimulation by a modification of the standard implantation technique. J Neurosurg Spine. 2006;4:300-303.
31 Lind G, et al. Baclofen-enhanced spinal cord stimulation and intrathecal baclofen alone for neuropathic pain: long-term outcome of a pilot study. Eur J Pain. 2008;12:132-136.
32 North RB, et al. Failed back surgery syndrome: five-year follow-up in 102 patients undergoing repeated operation. Neurosurgery. 1991;28:685-691.
33 North RB, et al. Failed back surgery syndrome: Five-year follow-up after spinal cord stimulator implantation. Neurosurgery. 1991;28:692-699.
34 North RB, et al. Spinal cord stimulation versus repeated lumbosacral spine surgery for chronic pain: a randomized, controlled trial. Neurosurgery. 2005;56:98-106.
35 Kumar K, et al. Spinal cord stimulation versus conventional medical management for neuropathic pain: a multicenter randomized controlled trial in patients with failed back surgery syndrome. Pain. 2007;132:179-188.
36 Kumar K, et al. The effects of spinal cord stimulation in neuropathic pain are sustained: a 24-month follow-up of the prospective randomized controlled multicenter trial of the effectiveness of spinal cord stimulation. Neurosurgery. 2008;63:762-768.
37 North RB, et al. Spinal cord stimulation versus reoperation for failed back surgery syndrome: a cost effectiveness and cost utility analysis based on a randomized, controlled trial. Neurosurgery. 2007;61:361-369.
38 National Institute for Health and Clinical Excellence (NICE). Spinal cord stimulation for chronic pain of neuropathic or ischemic origin. London: NICE Technology Appraisal Guidance, National Institute for Health and Clinical Excellence; 2008. accessed from http://www.nice.org.uk/nicemedia/live/12082/42367/42367.pdf July 8, 2010
39 Fowler K, North R. Patient-interactive PC interface to implanted, multichannel stimulators, Proceedings of 39th Annual Conference on Engineering in Medicine and Biology. Baltimore, Md: Biomedical Engineering Society; 1986. p 380
40 North RB, et al. Spinal cord stimulation for axial low back pain: a prospective, controlled trial comparing dual with single percutaneous electrodes. Spine. 2005;30:1412-1418.
41 North RB, et al. Spinal cord stimulation for axial low back pain: a prospective, controlled trial comparing 16-contact insulated electrode arrays with 4-contact percutaneous electrodes. Neuromodulation. 2006;9:56-67.
42 Holsheimer J, Struijk JJ, Tas NR. Effects of electrode geometry and combination on nerve fibre selectivity in spinal cord stimulation. Med Biol Eng Comput. 1995;33:676-682.