Chapter 9 Spinal Cord Infarction
Spinal cord infarction remains the less well-studied form of acute ischemic stroke. Although several useful studies describing the clinical and radiological features of spinal cord infarction have been published and the characteristics of the presenting syndrome are fairly well known, its risk factors (apart from aortic dissection and aortic surgery), area of maximal cord involvement, and prognosis are insufficiently understood. Furthermore, it remains a condition with no proven effective treatment.
Magnetic resonance imaging (MRI) allows documentation of spinal cord infarction. However, the true sensitivity of MRI for the early diagnosis of spinal cord ischemia is not well established. Imaging the cord is also important to exclude other causes of acute spinal cord syndrome such as cord compression (from displaced discs, epidural hematomas or abscesses, intradural extramedullary tumors, etc.), spinal cord hemorrhage, dural arteriovenous fistula, multiple sclerosis, neuromyelitis optica, infectious myelitis (e.g., West Nile virus), transverse myelitis (most often negative on early imaging), spinal cord contusion, or intramedullary tumors.1–3 MRI cannot be replaced by any other imaging modality for assessment of spinal cord infarction and exclusion of its differential diagnoses.
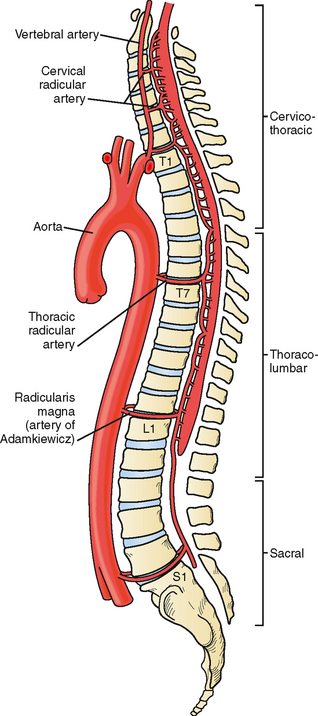
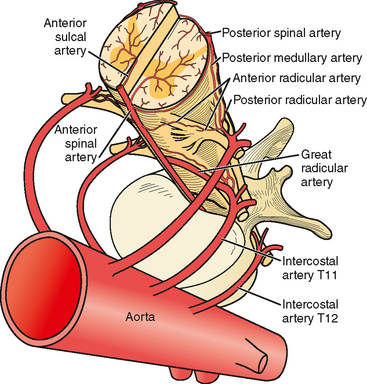
VASCULAR ANATOMY OF THE SPINAL CORD
The anterior spinal artery receives blood from the vertebral arteries in the cervical region and from radicular arteries in the thoracic and lumbar regions. Often two branches arising from each vertebral artery join at the upper cervical level to form the anterior spinal artery; however, many anatomical variations exist and these branches may arise from the posterior inferior cerebellar arteries or from cervical segmental branches. Just a few radicular arteries are responsible for the blood supply to the spinal arteries at the thoracolumbar level. They stem from segmental branches of the aorta (posterior intercostal and lumbar branches), which reach the intervertebral foramina and divide into the anterior and posterior radicular arteries. The largest radicular artery is the arteria radicularis magna of Adamkiewicz (or main anterior radicular artery), which most commonly arises on the left from T9 to T12 but occasionally can be positioned on the right (17% of cases) and arise anywhere from T5 to L4. Between the lower cervical and the mid- to lower thoracic levels, there are usually just two or three small radicular branches supplying this long segment of the cord. Hence the midthoracic area is traditionally considered a watershed territory at high risk for ischemia from hypoperfusion.4,5 Yet most cases of documented spinal cord ischemia do not occur in this area.6–8
Figures 9-1 and 9-2 illustrate the normal vascular anatomy of the spinal cord.
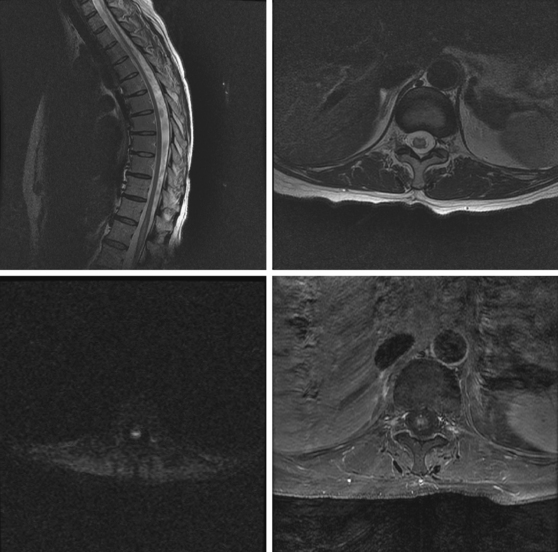
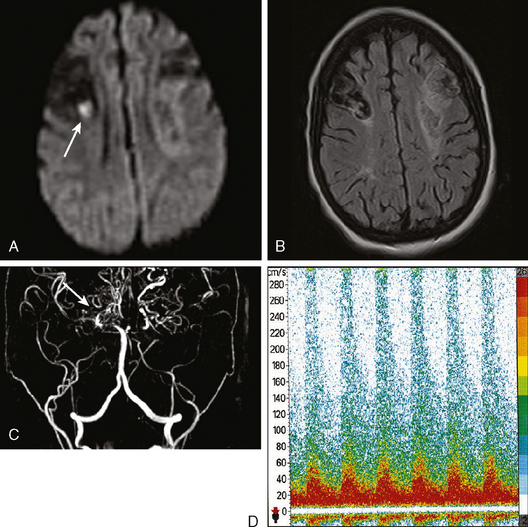
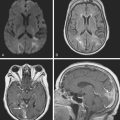
A 52-year-old woman with history of ovarian cancer in remission and no previous vascular disease presented with sudden onset of bilateral leg weakness. She had acute back pain initially, but it was short lasting. There was no loss of sphincter control. In the emergency department, she had flaccid paraplegia and leg areflexia. On sensory examination, she had decreased superficial pain and temperature sensation in both legs, but there was no sensory level detected in the trunk. Proprioception was normal. Computed tomography (CT) angiogram of chest and abdomen excluded aortic dissection but disclosed diffuse atherosclerotic changes throughout the descending aorta. MRI of the thoracolumbar spine revealed changes consistent with acute spinal cord ischemia from T11 to the tip of the conus medullaris (Figure 9-3). She was treated with interventions to optimize blood pressure, intravenous dexamethasone, and lumbar drainage. Over the following 48 hours, her sensation in the legs became nearly normal, but she only regained minimal motor function (some activation of hip flexors). She developed signs of neurogenic bladder and bowel. Comprehensive vascular evaluation uncovered no other mechanisms for the spinal cord ischemia other than aortic atherosclerosis. Three months later, her neurological condition remained unchanged.
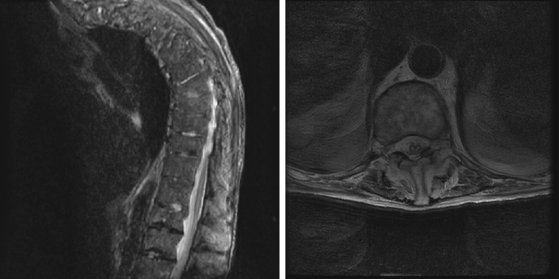
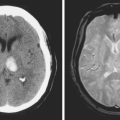
A 74-year-old man with history of severe peripheral vascular disease requiring bilateral iliac-to-femoral artery bypass surgery was admitted to the hospital for surgical repair of an enlarging thoracoabdominal aneurysm. A cerebrospinal drainage catheter was inserted before the initiation of the vascular surgery. The surgery was completed without apparent complications. However, following surgery the patient was noticed to be paraplegic. Neurological examination showed dense flaccid paraparesis with minimal movement of the toes as the only preserved motor function. No definitive sensory level was noted. MRI of the spine on postoperative day 2 was severely limited by motion artifact. A repeat MRI of the spine obtained 10 days after surgery (Figure 9-4) confirmed the presence of spinal cord infarction extending from T10–11 to the conus. The patient experienced no neurological recovery and was discharged 2 weeks later with persistent paraplegia, neurogenic bladder and bowel, and medications to control his severe back pain. He died 2 months after discharge in a nursing home from suspected pulmonary embolism (his preventive regimen of anticoagulation had been stopped after an episode of melena).
MANAGEMENT AND PROGNOSIS
1 Brinar VV, Habek M, Brinar M, Malojcic B, Boban M. The differential diagnosis of acute transverse myelitis. Clin Neurol Neurosurg. 2006;108:278-283.
2 Fortuna A, Ferrante L, Acqui M, Trillo G. Spinal cord ischemia diagnosed by MRI. Case report and review of the literature. J Neuroradiol. 1995;22:115-122.
3 Fukui MB, Swarnkar AS, Williams RL. Acute spontaneous spinal epidural hematomas. AJNR Am J Neuroradiol. 1999;20:1365-1372.
4 Cheshire WP, Santos CC, Massey EW, Howard JFJr. Spinal cord infarction: etiology and outcome. Neurology. 1996;47:321-330.
5 Shamji MF, Maziak DE, Shamji FM, Ginsberg RJ, Pon R. Circulation of the spinal cord: an important consideration for thoracic surgeons. Ann Thorac Surg. 2003;76:315-321.
6 Masson C, Pruvo JP, Meder JF, Cordonnier C, Touze E, De La Sayette V, et al. Spinal cord infarction: clinical and magnetic resonance imaging findings and short term outcome. J Neurol Neurosurg Psychiatry. 2004;75:1431-1435.
7 Nedeltchev K, Loher TJ, Stepper F, Arnold M, Schroth G, Mattle HP, et al. Long-term outcome of acute spinal cord ischemia syndrome. Stroke. 2004;35:560-565.
8 Weidauer S, Nichtweiss M, Lanfermann H, Zanella FE. Spinal cord infarction: MR imaging and clinical features in 16 cases. Neuroradiology. 2002;44:851-857.
9 Novy J, Carruzzo A, Maeder P, Bogousslavsky J. Spinal cord ischemia: clinical and imaging patterns, pathogenesis, and outcomes in 27 patients. Arch Neurol. 2006;63:1113-1120.
10 Mascalchi M, Cosottini M, Ferrito G, Salvi F, Nencini P, Quilici N. Posterior spinal artery infarct. AJNR Am J Neuroradiol. 1998;19:361-363.
11 Mawad ME, Rivera V, Crawford S, Ramirez A, Breitbach W. Spinal cord ischemia after resection of thoracoabdominal aortic aneurysms: MR findings in 24 patients. AJNR Am J Neuroradiol. 1990;11:987-991.
12 Faig J, Busse O, Salbeck R. Vertebral body infarction as a confirmatory sign of spinal cord ischemic stroke: report of three cases and review of the literature. Stroke. 1998;29:239-243.
13 Suzuki T, Kawaguchi S, Takebayashi T, Yokogushi K, Takada J, Yamashita T. Vertebral body ischemia in the posterior spinal artery syndrome: case report and review of the literature. Spine. 2003;28:E260-E264.
14 Thurnher MM, Bammer R. Diffusion-weighted MR imaging (DWI) in spinal cord ischemia. Neuroradiology. 2006;48:795-801.
15 Fujikawa A, Tsuchiya K, Takeuchi S, Hachiya J. Diffusion-weighted MR imaging in acute spinal cord ischemia. Eur Radiol. 2004;14:2076-2078.
16 Loher TJ, Bassetti CL, Lovblad KO, Stepper FP, Sturzenegger M, Kiefer C, et al. Diffusion-weighted MRI in acute spinal cord ischaemia. Neuroradiology. 2003;45:557-561.
17 Kuker W, Weller M, Klose U, Krapf H, Dichgans J, Nagele T. Diffusion-weighted MRI of spinal cord infarction—high resolution imaging and time course of diffusion abnormality. J Neurol. 2004;251:818-824.
18 Bammer R, Augustin M, Prokesch RW, Stollberger R, Fazekas F. Diffusion-weighted imaging of the spinal cord: interleaved echo-planar imaging is superior to fast spin-echo. J Magn Reson Imaging. 2002;15:364-373.
19 Zhang J, Huan Y, Qian Y, Sun L, Ge Y. Multishot diffusion-weighted imaging features in spinal cord infarction. J Spinal Disord Tech. 2005;18:277-282.
20 Bowen BC, Saraf-Lavi E, Pattany PM. MR angiography of the spine: update. Magn Reson Imaging Clin N Am. 2003;11:559-584.
21 Cina CS, Abouzahr L, Arena GO, Lagana A, Devereaux PJ, Farrokhyar F. Cerebrospinal fluid drainage to prevent paraplegia during thoracic and thoracoabdominal aortic aneurysm surgery: a systematic review and meta-analysis. J Vasc Surg. 2004;40:36-44.
22 Acher CW, Wynn MM, Hoch JR, Popic P, Archibald J, Turnipseed WD. Combined use of cerebral spinal fluid drainage and naloxone reduces the risk of paraplegia in thoracoabdominal aneurysm repair. J Vasc Surg. 1994;19:236-246.
23 Fleck TM, Koinig H, Moidl R, Czerny M, Hamilton C, Schifferer A, et al. Improved outcome in thoracoabdominal aortic aneurysm repair: the role of cerebrospinal fluid drainage. Neurocrit Care. 2005;2:11-16.
24 Safi HJ, Hess KR, Randel M, Iliopoulos DC, Baldwin JC, Mootha RK, et al. Cerebrospinal fluid drainage and distal aortic perfusion: reducing neurologic complications in repair of thoracoabdominal aortic aneurysm types I and II. J Vasc Surg. 1996;23:223-228.
25 Cambria RP, Davison JK, Carter C, Brewster DC, Chang Y, Clark KA, et al. Epidural cooling for spinal cord protection during thoracoabdominal aneurysm repair: a five-year experience. J Vasc Surg. 2000;31:1093-1102.
26 Weaver KD, Wiseman DB, Farber M, Ewend MG, Marston W, Keagy BA. Complications of lumbar drainage after thoracoabdominal aortic aneurysm repair. J Vasc Surg. 2001;34:623-627.
27 Blacker DJ, Wijdicks EF, Ramakrishna G. Resolution of severe paraplegia due to aortic dissection after CSF drainage. Neurology. 2003;61:142-143.