80 Spinal Cord Disorders
Etiology and Pathogenesis
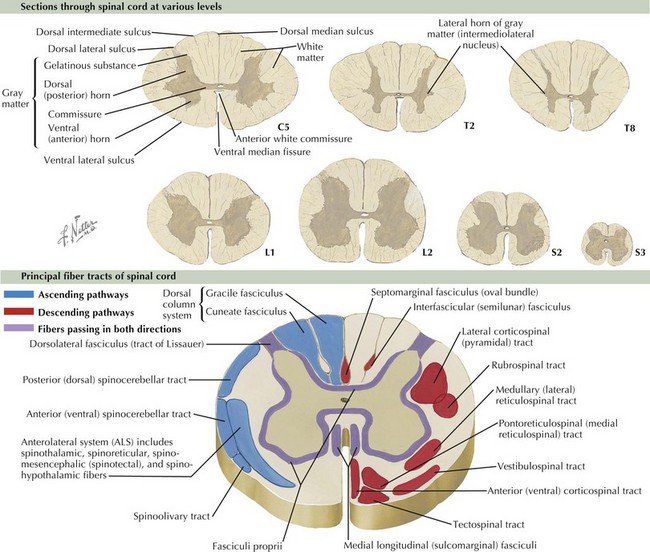
According to the Centers for Disease Control and Prevention, spina bifida, the most common neural tube defect, occurs at a rate of two in 10,000 live births and results in varying degrees of disability from clinically normal to paraplegia. Traumatic spinal cord injury occurs at a rate of about 40 cases per million people per year and annually costs $9.7 billion in health care costs. Of these cases, it is estimated that up to half occur in adolescence and young adulthood. To diagnose and treat the disorders of the spinal cord, an understanding of its anatomy and how to examine for dysfunction of the spinal cord is imperative. The spinal cord is divided into four sections: cervical, thoracic, lumbar, and sacral (C, T, L, and S). It terminates at vertebral body level L2–L3 in infants, and in grown children and adults, it terminates at level L1–L2, where the cauda equina, the collection of nerves exiting the cord, begins. The spinal cord itself is sectioned in to a central H-shaped region of gray matter and surrounding white matter tracts (Figure 80-1).
Clinical Presentation and Differential Diagnosis
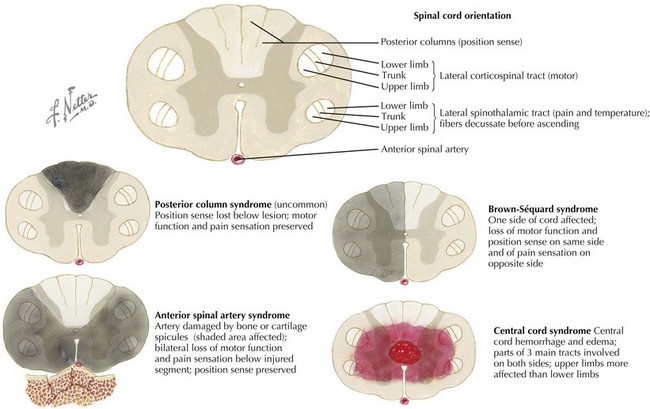
There are common patterns of motor and sensory involvement depending on the localization of disease within the spinal cord. Table 80-1 describes the features of some typical patterns or spinal cord disease and their common causes (Figure 80-2).
Table 80-1 Features of Typical Patterns or Spinal Cord Disease and Common Causes
| Localization | Common Pattern of Weakness and Sensory Loss | Common Causes in Pediatric Patients |
|---|---|---|
| Cervical spinal cord |
Evaluation and Management
Because the etiology of transverse myelitis is so diverse, from demyelinating and inflammatory or autoimmune disease to infections to nutritional and metabolic derangements, the evaluation of these patients is similarly broad. The evaluation for transverse myelitis should include an MRI of the brain to look for lesions above the foramen magnum that would suggest multiple sclerosis (see Chapter 78). It should also include serum tests such as inflammatory markers, vitamin levels (such as B12, folate, vitamin D, and copper), a rheumatologic evaluation (including autoantibody seen in systemic lupus erythematosus, Sjögren’s syndrome, sarcoidosis, and other autoimmune disease), as well as serum infectious evaluation as indicated (Lyme disease, Mycoplasma, HIV, Epstein-Barr virus, cytomegalovirus). If there are risk factors, the patient should have evaluation for tuberculosis. Finally, cerebrospinal analysis including cell count, glucose, protein, culture, cytology, oligoclonal bands, myelin basic protein, immunoglobulin G, and viral polymerase chain reaction tests (enterovirus, herpesviruses) as indicated are important for determining diagnosis and treatment. For viral myelitis, treatment is typically supportive.
Bracken, MB: Steroids for acute spinal cord injury. Cochrane Database Syst Rev 2:CD001046, 2002.
Bracken MB, Holford TR. Neurological and functional status 1 year after acute spinal cord injury: estimates of functional recovery in National Acute Spinal Cord Injury Study II from results modeled in National Acute Spinal Cord Injury Study III. J Neurosurg. 2002;96(3 suppl):259-266.
Defresne P, Hollenberg H, Husson B, et al. Acute transverse myelitis in children: clinical course and prognostic factors. J Child Neurol. 2003;18(6):401-406.
Hall ED, Springer JE. Neuroprotection and acute spinal cord injury: a reappraisal. NeuroRx. 2004;1(1):80-100.
Kaplin AI, Krishnan C, Deshpande DM, et al. Diagnosis and management of acute myelopathies. Neurologist. 2005;11(1):2-18.
Lammertse D, Dungan D, Dreisbach J, et al. National Institute on Disability and Rehabilitation: Neuroimaging in traumatic spinal cord injury: an evidence-based review for clinical practice and research. J Spinal Cord Med. 2007;30(3):205-214.
Wagner R, Jagoda A. Spinal cord syndromes. Emerg Med Clin North Am. 1997;15(3):699-711.