Chapter 1 SORE MOUTH
EXAMINATION OF THE MOUTH
Wear gloves, a mask and spectacles or goggles for oral examinations.
Extraoral
Is there any facial swelling, asymmetry or altered cutaneous sensation? Are the submandibular and other cervical lymph nodes palpable?
CAUSES OF SORE MOUTH
| Trauma | Gastrointestinal |
Infections
Fungal infections
These are usually due to Candida. Thrush (acute pseudomembranous candidiasis), usually due to Candida albicans, is a relatively common cause of sore mouth. The diagnosis can usually be made clinically from the scattered white plaques resembling clotted milk that are easily wiped off the oral mucosa, leaving a red base. If doubt remains, laboratory confirmation is available by microscopy and culture of a swab. Always look for predisposing factors. Systemic causes include pharmacotherapy with immunosuppressive drugs, steroids, cytotoxic therapy, or antibiotics, as well as human immunodeficiency virus (HIV) infection, particularly before HAART begins, and diabetes.
Management
Topical antifungals, amphotericin B 10 mg lozenges three times daily for 1 week, dissolved slowly in mouth or nystatin pastilles 100,000 units or lozenges 500,000 units, allowed to dissolve in mouth or as a suspension 100,000 units/mL four times daily for 1 week. In immunocompromised states, oral itraconazole (contraindicated in acute hepatitis) 100–200 mg daily for 1 week may be needed.
Viral infections
Herpes simplex (human herpes virus type 1, less commonly 2)
Oral herpes simplex infections usually present in young children with fever, malaise, enlarged tender submandibular lymph nodes, widespread small irregular mouth ‘ulcers’ and swollen inflamed gums (often dismissed as ‘teething’). The diagnosis can usually be made clinically, but laboratory tests include a smear for microscopy, swab for culture or direct immunofluorescence of a saline mouth rinse and a blood sample to show an immediate rise in IgM antibody. Aqueous 0.2% chlorhexidine mouth baths or, for the immunocompromised, aciclovir 400 mg five times daily for 5 days or famciclovir for aciclovir-resistant infections. Recurrent herpes simplex infections are usually restricted to the lips (herpes labialis or ‘cold sores’), and only rarely affect the oral cavity, which may be involved, however, where HSV is reactivated in immunocompromised states. Early application of 5% aciclovir or penciclovir cream is useful for treating cold sores.
Gum disorders
Gingivitis
Chronic gingival inflammation is common and results from bacterial plaque and calculus deposits on the teeth. The gum margins are red, bleed easily while brushing teeth or eating but usually this gingivitis is painless. A red line limited to the entire gingival margin (linear gingival erythema) can be a marker of HIV infection.
Dry mouth (xerostomia)
Patients with xerostomia are mostly middle aged or elderly women and complain of difficulty in eating, swallowing, altered taste and an uncomfortably leathery dry mouth. The tongue is depapillated with a ‘cobblestone’ appearance, the normal pool of saliva is absent and the buccal mucosa is glazed, erythematous and adherent. Dental caries becomes a problem and oral Candida infections can occur.
There are many causes of dry mouth (see Table 1.2). Note that salivary flow rates do not significantly decrease with ageing, but medication is a significant cause of xerostomia in the elderly. The symptoms can be relieved by sips of tap water (usually contains fluoride), or conveniently delivered with a plastic spray bottle. Fluoride in toothpaste, plus a sodium fluoride 0.2% mouth rinse, 10 mL once a week, protects against caries. Sugar-free sweets usefully promote salivation. Candida infections causing thrush or a red dry sore mouth with angular cheilitis respond to nystatin or amphotericin B (as detailed above). Poor denture hygiene or a continuous day-and-night wearing habit favour candidiasis.
| Reduced salivary flow | |
| Medication | |
ORAL ULCERATION
| Trauma | Viral infection |
| Idiopathic |
DLE = discoid lupus erythematosus; SLE = systemic lupus erythematosus.
Traumatic
Traumatic ulcers from lip, cheek or tongue biting or due to ill fitting dentures are common. They are usually solitary and irregular. After the cause is removed, the ulcer heals spontaneously and a chlorhexidine mouth rinse speeds healing.
Recurrent aphthous ulcers
These tend to start in childhood or adolescence. Minor aphthae occur in crops of 2–10 simultaneous ulcers with an erythematous halo and yellow or grey slough on the lips, cheeks, sides and ventral surface of the tongue and heal spontaneously in 7–10 days. The cause remains unknown. Any pain and discomfort is usually minor but responds to topical steroids such as triamcinolone acetonide 0.1% paste (rather messy), or fluocinonide 0.1% in Orabase or betamethasone 0.05% in Orabase if more severe or an aqueous chlorhexidine 0.2% mouthrinse. Associated folate, iron or B12 deficiencies or anaemias should be corrected.
Crohn’s disease
A similar clinical and histological appearance is occasionally encountered in patients in whom investigations for intestinal Crohn’s disease are negative. This condition has been called ‘orofacial granulomatosis’ and may respond to dietary elimination of ingredients such as cinnamon or monosodium glutamate or other dietary additives. Others assert that these lesions are Crohn’s disease. Topical steroids applied to the ulcers may be helpful.
Erythema multiforme
Young men are most often affected by this bullous eruption. Target or iris-like skin lesions on the limbs and erosions in the mouth are pathognomonic. In severe cases, the conjunctiva or genital mucosa may also be involved, with fever (toxic epidermal necrosis or Stevens-Johnson syndrome). Occasionally only the mouth is involved.
White lesions
Lichen planus
Middle-aged women are mostly affected by lichen planus. The characteristic itchy red-violet polygonal skin papules on the forearms and shins may be absent. Typically, white interconnecting striae and papules form a lace-like pattern especially on the buccal mucosa and ventral surface of the tongue, usually in a bilaterally symmetrical distribution. The gingivae can be red and atrophic (desquamative gingivitis). Ulceration in the erosive form may be severe. The diagnosis is often obvious clinically but a biopsy should be undertaken in doubtful cases. Remember that lichenoid reactions to drugs or dental fillings or graft-versus-host reaction may mimic idiopathic lichen planus quite closely. Aqueous chlorhexidine 0.2% and topical steroids provide some relief for the soreness. Brief courses of systemic prednisone, retinoids or other immunosuppressive agents may be used by specialists in cases of severe erosive lichen planus. Oral cancer is a rare complication of long-standing erosive lichen planus, especially in middle-aged or elderly women.
Squamous cell carcinoma
A solitary ulcer with a raised indurated margin, which persists for 3 weeks despite any treatments, must be biopsied to exclude a carcinoma. A swelling, a white patch or gingival swelling causing loosening of the adjacent teeth, are other presentations.
SUMMARY
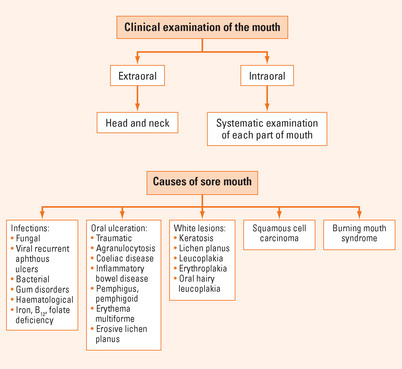
Causes of sore mouth
Think about infections (fungal, viral, bacterial), gum disorders (gingivitis), dry mouth (xerostomia: medicines are an important cause in the elderly as is poor denture hygiene) and haematological causes (iron deficiency, vitamin B12 and folate deficiency) (Figure 1.1).
White lesions
Many white mucosal patches result from friction of the teeth or tobacco smoking, and are usually reversible and non-dysplastic. A biopsy is recommended.

 finger breadths can be inserted between upper and lower incisors.
finger breadths can be inserted between upper and lower incisors.