CHAPTER 6 Soft Tissue Impingement of the Ankle Joint
Lateral ligament sprains of the ankle joint are the most common musculoskeletal injury. They are especially common in sports such as ballet dancing, cross-country running, soccer, and basketball. Ankle sprains account for 45% of all injuries in basketball and 31% of all injuries in soccer.1–3
After an ankle sprain, anterolateral impingement syndrome is a common cause of continued lateral ankle pain and disability. This syndrome, which has been well documented, occurs in 20% to 40% of patients.1 The diagnosis is often elusive, especially in ankles that are stable on examination. Morris, who called the condition athlete’s ankle, first described impingement in the ankle in the literature in 1943.4 It was later called footballer’s ankle in a report by McMurray.5
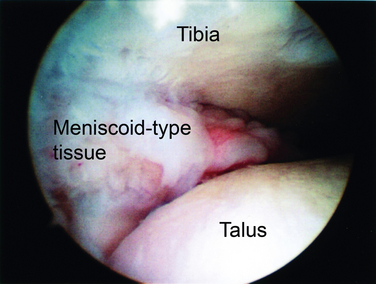
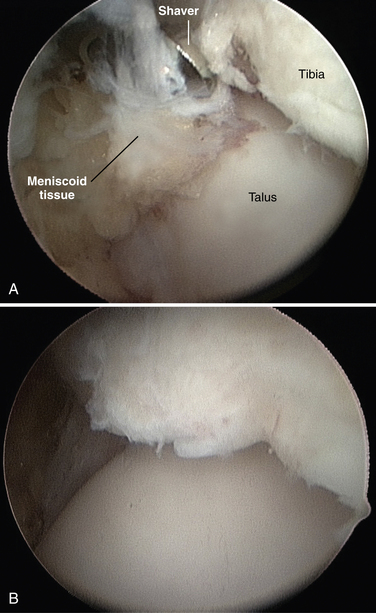
The pathologic anatomy was first described as soft tissue pathology by Wolin and coworkers in 1950.6 They described nine patients with continued pain and swelling of the lateral aspect of the ankle after an inversion injury. Arthrotomy of the ankle in these patients revealed a dense mass of hyalinized connective tissue that extended into the joint from the anteroinferior portion of the anterior talofibular ligament (ATFL). Wolin called this a meniscoid lesion because of its resemblance to a torn meniscus in the knee (Fig. 6-1). He believed pain and disability resulted from entrapment of this tissue between the fibula and talus with dorsiflexion of the ankle. Excision of this tissue resulted in pain relief in all nine patients.
Waller7 later described an anterolateral corner compression syndrome that resulted in pain along the anteroinferior fibula and the anterolateral talus. Patients typically had a pronated foot with a valgus heel. This mechanism resulted in a synovial compression and chondromalacia of the lateral aspect of the talar dome. Guhl8 described this condition as anterolateral synovial impingement when there is no evidence of ligamentous tissue and only hypertrophied synovium in the pathologic specimen. Andrews and colleagues9 emphasized the meniscoid lesion and hypothesized that it was caused by partial tearing of the ATFL. They thought the partially torn ligament became entrapped in the anterolateral gutter. Pain relief was reported with excision of this tissue.
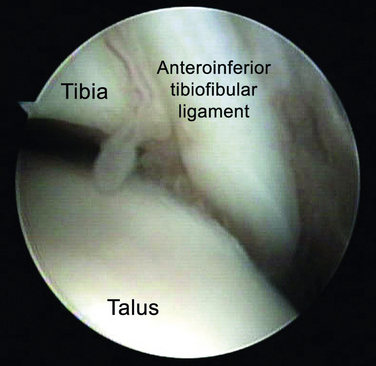
Based on histopathologic analysis, Ferkel and associates10 thought the impingement was caused by hypertrophied synovium. Later, Bassett and colleagues11 described a distal fascicle of the anterior-inferior tibiofibular (syndesmotic) ligament (Fig. 6-2). During dorsiflexion of the ankle, this ligament was shown to come into contact with the anterolateral aspect of the talar dome. Presence of this fascicle was confirmed in 10 of 11 cadaveric specimens.
NORMAL AND PATHOLOGIC ANATOMY
The lateral ligamentous complex consists of the ATFL, the calcaneofibular ligament (CFL), and the posterior talofibular ligament (PTFL). The ATFL arises from the anterior aspect of the distal fibula and inserts on the body of the talus just anterior to the articular facet. It is usually 1.5 to 2 cm long and spans the anterior aspect of the ankle joint. It is confluent with the anterior lateral capsule. The CFL arises just distal to the origin of the ATFL; it does not arise from the tip of the fibula. The ligament runs posterior, medial, and inferior to its origin to insert on the calcaneus. It becomes confluent with the peroneal tendon sheath near its insertion. The PTFL arises from the posteromedial aspect of the lateral malleolus and runs medially to insert on the posterior aspect of the talus. The insertion is broad and involves almost the entire lip of the talus. The PTFL, like the ATFL, is confluent with the joint capsule.1,12
There are three sites of impingement in anterolateral ankle impingement.1 The first involves the ATFL and the area of the lateral gutter and lateral talar dome. The second involves the inferior fascicle of the AITFL, known as Bassett’s ligament. The third is the superior portion of the AITFL.
PATIENT EVALUATION
History and Physical Examination
Patients with anterolateral impingement typically present with a history of multiple ankle sprains followed by chronic, persistent ankle pain, especially with ambulation. Other complaints include ankle weakness and a feeling of the ankle giving way. It is not uncommon to have persistent catching and swelling in the anterolateral aspect of the ankle. Pain often is vague and poorly localized. It may involve the sinus tarsi and the syndesmotic region, depending on the location of the impingement. Pain is usually absent at rest and commences with weight bearing.13,14
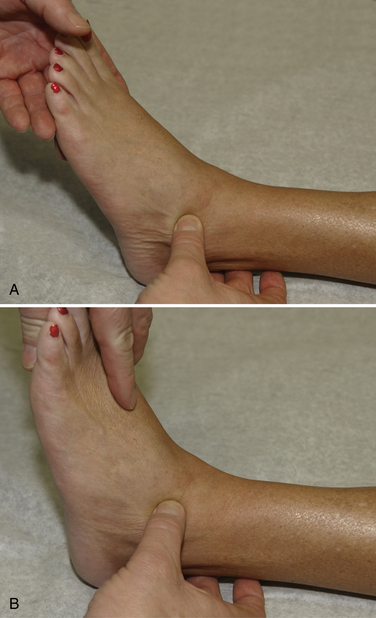
Physical examination begins with observing the patient walk into the room. Because of marked inflammation and pain, the patient may have an antalgic gait. Inspection of the ankle frequently reveals swelling in the anterolateral aspect of the ankle and the lateral gutter. Palpation may elicit pain along the ATFL, along the lateral gutter, and occasionally along the CFL and the syndesmosis (Fig. 6-3). Pain over the ATFL and syndesmosis increases with dorsiflexion of the ankle during palpation. Tenderness depends on the location of the impingement. Determining the origin of the pain is important. Range of motion is typically normal with plantar flexion, but dorsiflexion may be limited because of the impingement. Excessive foot pronation, pes planus, and posterior tibial tendonitis can aggravate the condition. Patients usually do not have increased laxity with anterior drawer or varus stress testing. The examiner must be careful in differentiating pain in the anterolateral gutter from pain in the sinus tarsi. If injection of local anesthetic into the sinus tarsi eliminates the pain, the diagnosis is not anterolateral impingement.1,13,14
Diagnostic Imaging
Imaging modalities include radiography, tomography, computed tomography (CT), and magnetic resonance imaging (MRI). Radiographs are typically negative. They show absence of fractures, no widening of the ankle mortise, and no significant degenerative changes. Anterior tibial osteophytes and a shallow talar neck may be present. Stress radiographs are negative because no instability is present.
Tomography and CT findings are typically negative. Hauger and colleagues15 performed CT arthrography for patients with symptoms of anterolateral impingement. The investigators concluded that CT arthrography was a valid test if there was a nodular formation in the lateral gutter or if there was an irregular appearance of the edges of the lateral gutter. These findings corresponded to a meniscoid lesion or an abundant fibrous reaction on arthroscopy. These findings were also statistically associated with a chondropathy.
MRI has a sensitivity of 83.3%, a specificity of 78.6%, and a diagnostic accuracy of 78.8%.1 Sagittal, T1-weighted and short tau inversion recovery (STIR) images can delineate edema or a soft tissue mass that has caused displacement of the subcutaneous fat normally found immediately adjacent to the lateral gutter. Rubin and coworkers16 described the use of T2-weighted and fast-spin or STIR images in at least two orthogonal planes to study soft tissue anterolateral impingement. They found that accurate assessment of the anterolateral gutter could be made only when fluid was distending the compartment. They also found that if the ATFL was not visualized, they could not differentiate whether the offending soft tissue was synovial tissue or the ligament. In such cases, they recommended physical examination and stress radiographs to help determine the cause of the impingement. They concluded that an MRI finding of an abnormal soft tissue mass in the lateral gutter distinct from the ATFL suggested the diagnosis of soft tissue impingement. Huh and associates17 showed that contrast-enhanced, three-dimensional, fast-gradient recalled acquisition in steady state with radiofrequency spoiling MRI revealed high specificity of soft tissue impingement evaluation in patients with chronic post-traumatic ankle pain. Kinematic MRI has also been used to evaluate soft tissue impingement with some success.
TREATMENT
Indications and Contraindications
Failure of conservative treatment, including a short period of immobilization, progressive weight bearing, physical therapy, nonsteroidal anti-inflammatory medications, and selective injections for 3 to 6 months, is an indication for arthroscopic evaluation and treatment. Contraindications are limited and include functional instability and complex regional pain syndrome.1
Conservative Management
Initial treatment should include a period of at least 3 months of conservative care. Initial treatment methods are varied and include a period of immobilization. This may be a period of absolute immobilization in a cast or relative immobilization in a boot. Progressive weight bearing after immobilization is a good idea, especially if there was a recent ankle sprain. Beneficial physical therapy includes Achilles tendon stretching and anterior tibial and peroneal tendon strengthening. Ankle stabilization bracing or taping during athletic activities may alleviate some pain. Nonsteroidal anti-inflammatory medications for a short period may decrease some of the inflammation. Local steroid injections can help to decrease inflammation. Selective anesthetic injections may help differentiate anterolateral impingement from other diagnoses, such as sinus tarsi syndrome.1,13,14
Arthroscopic Technique
Curettes, picks, and elevators of appropriate size for ankle instrumentation should be available. Many small shavers can be used for soft tissue and bone to facilitate access to the ankle joint to remove pathologic tissue. Monopolar or bipolar, 2.0-mm radiofrequency probes are also helpful.
Ankle distraction has evolved considerably from the time when invasive distraction was always used. For arthroscopic procedures, particularly in the anterior compartment, several commercial products are available that enable soft tissue distraction. Noninvasive distraction can be gravity distraction or manual distraction, in which the operating surgeon uses a strap around the ankle to open the joint (Fig. 6-4). We prefer a Velcro strap to a metallic distractor because it allows easier on and off positioning and greater control of the amount of tension applied.
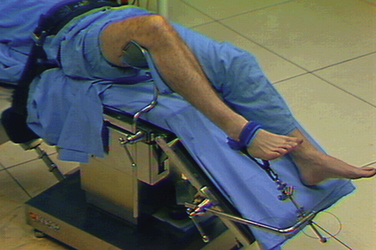
Arthroscopy of the ankle is usually performed with the patient in the supine position and the knee level or flexed. The lateral decubitus position with the patient supported on a beanbag or the prone position can be used for subtalar and hindfoot arthroscopy. We use a special thigh holder that is located inferior to the thigh tourniquet to elevate the leg and avoid pressure to the popliteal area (Fig. 6-5). The holder should be well padded to avoid neurovascular injury. The hip is flexed 40 to 90 degrees. The entire table is raised, and the head is elevated so the foot of the table can be lowered. This position allows the surgeon to stand or sit. It also provides posterior access to the ankle.
Ankle arthroscopy is usually performed through the anterolateral and the anteromedial portals (Table 6-1). Use of a central portal has been discontinued because of the potential for neurovascular injury.
| Portal Site | Landmarks | Structures at Risk |
|---|---|---|
| Anteromedial | Medial to anterior tibialis tendon |
With proper distraction, the arthroscope can swing across the midportion of the joint. There is a sulcus between the tibia and talus that allows the arthroscope to be pushed posteriorly. From this position, the operator should be able to see the posterior capsule. The arthroscope is then moved to the medial portal, allowing the surgeon to look down the medial gutter. If after diagnostic examination of the joint the diagnosis of soft tissue impingement is made, the arthroscope is placed medially, and a motorized shaver is brought into the lateral portal. The soft tissue entrapped between the tibia and talus that can be seen with forced dorsiflexion is then removed. Care is taken to visualize the AITFL. If the ligament is thought to be causing part of the impingement or it is partly frayed, a portion of it can be removed with the shaver or the radiofrequency probe (Fig. 6-6).
PEARLS& PITFALLS
Postoperative Rehabilitation Protocol
Sutures are removed at 4 to 5 days after surgery.14 At that time, the patient is allowed to start active assisted range-of-motion exercises, strengthening, and touch-down weight bearing. Patients progress to partial and full weight bearing as motion and strength return.
CONCLUSIONS
Anterior soft tissue impingement is a frequent cause of chronic ankle pain after ankle sprain. Presenting symptoms include vague and persistent pain in the area of the anterolateral gutter and occasionally the sinus tarsi. Pain is typically absent at rest and is exacerbated with activity. Physical examination reveals pain with forced dorsiflexion of the ankle, and ligamentous instability is not found with anterior drawer testing. Fullness and swelling may be found in the area of the anterolateral gutter. Causes of the impingement include synovial hypertrophy, the distal fascicle of the AITFL, and an impinging AITFL.
1. Coughlin MJ, Mann RA, Saltzman CL. Surgery of the Foot and Ankle, 8th ed. St. Louis, MO: Mosby; 2006.
2. Ekstrand J, Tropp H. The incidence of ankle sprains in soccer. Foot Ankle. 1990;11:41-44.
3. Sandelin J. Acute Sports Injuries. A Clinical and Epidemiological Study. 1988 University of Helsinki Helsinki, Finland [dissertation]
4. Morris LH. News notes. J Bone Joint Surg. 1943;25:220.
5. McMurray TP. Footballer’s ankle. J Bone Joint Surg Br. 1950;32B:68-69.
6. Wolin I, Glassman F, Sideman S, Levinthal DH. Internal derangement of the talofibular component of the ankle. Surg Gynecol Obstet. 1950;91:193-200.
7. Waller JF. Hindfoot and midfoot problems of the runner. In: Mack RP, editor. Symposium on the Foot and Leg in Running Sports. St. Louis, MO: Mosby–Year Book; 1982:64-71.
8. Soft tissue synovial pathology. In: Guhl JF, editor. Ankle Arthroscopy; Pathology and Surgical Techniques. Thorofare, NJ: Slack; 1988:93-135.
9. Andrews JR, Drez DJ, McGinty JB. Symposium. arthroscopy of joints other than the knee, Contemp Orthop. 91984 71-100.
10. Ferkel RD, Karzel RP, Del Pizzo W, et al. Arthroscopic treatment of anterolateral impingement of the ankle. Am J Sports Med. 1991;19:440-446.
11. Basset FH 3rd, Gates HS 3rd, Billys BJ, et al. Talar impingement by the anteroinferior tibiofibular ligament. a cause of chronic pain in the ankle after inversion sprain, J Bone Joint Surg Am. 72A1990 55-59.
12. Lassiter TEJr, Malone TR, Garrett WEJr. Injury to the lateral ligaments of the ankle. Orthop Clin North Am. 1989;20:629-640.
13. Jacobson KE, Liu SH. Anterolateral impingement of the ankle. J Med Assoc Ga. 1992;81:297-299.
14. Liu SH, Raskin A, Osti L, et al. Arthroscopic treatment of anterolateral ankle impingement. Arthroscopy. 1994;10:215-218.
15. Hauger O, Moinard M, Lasalarie JC, et al. Anterolateral compartment of the ankle in the lateral impingement syndrome. appearance on CT arthroscopy, AJR Am J Roentgenol. 1731999 685-690.
16. Rubin D, Tishkoff N, Britton C, et al. Anterolateral soft-tissue impingement in the ankle. diagnosis using MR imaging, AJR Am J Roentgenol. 1691997 829-835.
17. Huh Y-M, Suh J-S, Lee J-W, Song H-T. Synovitis and soft tissue impingement of the ankle. assessment with enhanced three-dimensional FSPGR MR imaging, J Magn Reson Imaging. 192004 108-116.