Soft Tissue Healing Considerations After Surgery
Robert Cantu and Jason A. Steffe
Physical therapists work daily on a variety of connective tissue types that are dynamic and have an amazing capacity for change. Changes in these types of tissues are driven by a number of factors, including trauma, surgery, immobilization, posture, and repeated stresses. The physical therapist should have a good working knowledge of the normal histology and biomechanics of connective tissue. Additionally, the astute therapist should have a thorough understanding of the way connective tissue responds to immobilization, trauma, and remobilization. Both experienced and novice physical therapists can benefit from a good “mental picture” of how connective tissue operates as they think through, strategize, and treat postsurgical patients.
The classic view of connective tissue and its response to trauma and immobilization is that these tissues are inert and noncontractile, with muscle fibers being the only contractile element. While the body of literature documenting this view is solid and well accepted, newer studies have uncovered some exciting possibilities regarding the “contractility” of connective tissue. If fascia, ligaments, and tendons have a limited ability to behave like contractile tissue, many of the changes therapists have felt immediately after performing manual techniques can be validated and substantiated. Additionally, treatment strategies would change, or if not change, be better explained. In the context of postsurgical management, treating “inert” tissue as “contractile” could certainly change treatment perspectives.
Surgery Defined
Because this text primarily considers postsurgical rehabilitation, an operational definition of surgery is in order. For the purpose of considering injury and repair of soft tissue, surgery may be defined as controlled trauma produced by a trained professional to correct uncontrolled trauma. The reason for this specific, contextual definition is that connective tissues respond in characteristic ways to immobilization and trauma. Because surgery is itself a form of trauma that is usually followed by some form of immobilization, the physical therapist must understand the way tissues respond to both immobilization and trauma.
This chapter begins by presenting the classical view of basic histology and the biomechanics of connective tissue. Next, the histopathology and pathomechanics of connective tissue (i.e., the way connective tissues respond to immobilization, trauma, and remobilization) will be addressed. This chapter will also address some basic principles of soft tissue mobilization based on the basic science behind immobilization, trauma, and remobilization of the connective tissue. Finally, there will be a discussion of the more recent literature suggesting the limited contractility potential of connective tissue.
Histology And Biomechanics Of Connective Tissue
The connective tissue system in the human body is quite extensive. Connective tissue makes up 16% of the body’s weight and holds 25% of the body’s water.1 The “soft” connective tissue forms ligaments, tendons, periosteum, joint capsules, aponeuroses, nerve and muscle sheaths, blood vessel walls, and the bed and framework of the internal organs. If the bony structures were removed, then a semblance of structure would remain from the connective tissue.1–5
A majority of the tissue affected by mobilization are “inert” connective tissue. During joint mobilization, for example, the tissues being mobilized are the joint capsule and the surrounding ligaments and connective tissue. Arthrokinematic rules are followed, but the tissue being mobilized is classified as inert connective tissue. Therefore, background knowledge of the histology and histopathology of connective tissue is essential for the practicing physical therapist.
Normal Histology and Biomechanics of Connective Tissue Cells
Connective tissue has two components: (1) the cells and (2) the extracellular matrix. The two cells of primary importance in connective tissue are the fibroblast and the myofibroblast. The fibroblast synthesizes all the inert components of connective tissue, including collagen, elastin, reticulin, and ground substance.1–5 The myofibroblast is a specialized cell that contains smooth muscle elements and has a capacity to contract.6–9
Extracellular Matrix
The extracellular matrix of connective tissue includes connective tissue fibers and ground substance. The connective tissue fibers include collagen (the most tensile), elastin, and reticulin (the most extensible). Collagen, elastin, and reticulin provide the tensile support that connective tissue offers. Extensibility or the lack of it is driven by the relative density and percentage of the connective tissue fibers. Tissues with less collagen density and a greater proportion of elastin fibers are more pliable than tissue with a greater density and proportion of collagen fibers.1–3
The ground substance of connective tissue plays a very different role in the connective tissue response to immobility, trauma, and remobilization. The ground substance is the viscous, gel-like substance in which the cells and connective tissue fibers lie. It acts as a lubricant for collagen fibers in conditions of normal mobility and maintains a crucial distance between collagen fibers. The ground substance also is a medium for the diffusion of nutrients and waste products and acts as a mechanical barrier for invading microorganisms. It has a much shorter half-life than collagen and, as will be discussed, is much more quickly affected by immobilization than collagen.4,10
Three Types of Connective Tissue
Connective tissue is classified according to fiber density and orientation. The three types of connective tissue found in the human body are (1) dense regular, (2) dense irregular, and (3) loose irregular (Table 2-1).11,12
TABLE 2-1
Classification of Connective Tissue
| Tissue Type | Specific Structures | Characteristics of the Tissue |
| Dense regular | Ligaments, tendons | Dense, parallel arrangement of collagen fibers; proportionally less ground substance |
| Dense irregular | Aponeurosis, periosteum, joint capsules, dermis of skin, areas of high mechanical stress | Dense, multidirectional arrangement of collagen fibers; able to resist multidirectional stress |
| Loose irregular | Superficial fascial sheaths, muscle and nerve sheaths, support sheaths of internal organs | Sparse, multidirectional arrangement of collagen fibers; greater amounts of elastin present |
From Cantu R, Grodin A: Myofascial manipulation: Theory and clinical application, Gaithersburg, Md, 1992, Aspen.
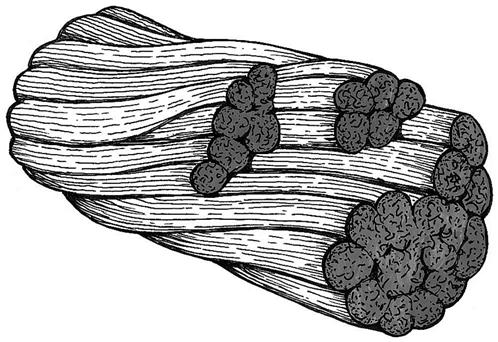
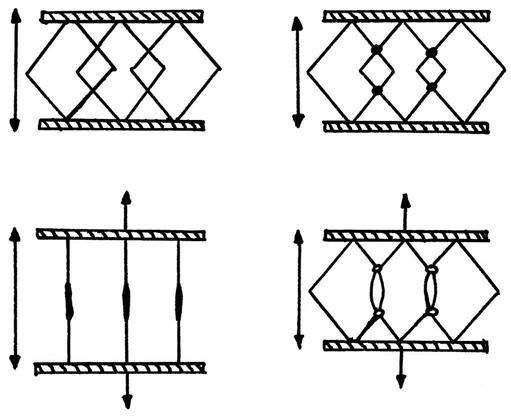
Dense regular connective tissue includes ligaments and tendons (Fig. 2-1).5 The fiber orientation is unidirectional for the purpose of attenuating unidirectional forces. The high density of collagen fibers accounts for the high degree of tensile strength and lack of extensibility in these tissue. Relatively low vascularity and water content account for the slow diffusion of nutrients and the resulting slower healing times. Dense regular connective tissue is the most tensile and least extensible of the connective tissue types.
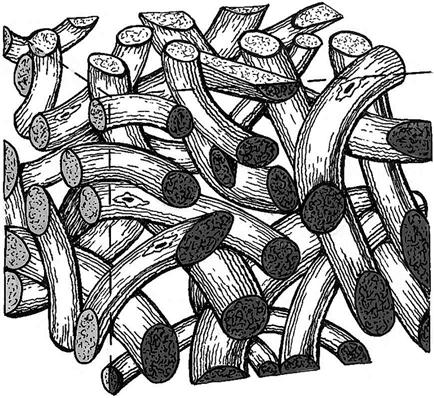
Dense irregular connective tissue includes joint capsules, periosteum, and aponeuroses. The primary difference between dense regular and dense irregular connective tissue is that dense irregular connective tissue has a multidimensional fiber orientation (Fig. 2-2). This multidimensional orientation allows the tissue to attenuate forces in numerous directions. The density of collagen fibers is high, producing a high degree of tensile strength and a low degree of extensibility. Dense irregular connective tissue also has low vascularity and water content, resulting in slow diffusion of nutrients and slower healing times.5
Loose irregular connective tissue includes, but is not limited to, the superficial fascial sheath of the body directly under the skin, the muscle and nerve sheaths, and the bed and framework of the internal organs. Similarly to dense irregular connective tissue, loose irregular connective tissue has a multidimensional tissue orientation. However, the density of collagen fibers is much less than that of dense irregular connective tissue. The relative vascularity and water content of loose irregular connective tissue is much greater than dense regular and dense irregular connective tissue. Therefore, it is much more pliable and extensible, and exhibits faster healing times after trauma. Loose irregular connective tissue also is the easiest to mobilize.5
Normal Biomechanics of Connective Tissue
Connective tissues have unique deformation characteristics that enable them to be effective shock attenuators. This is termed the viscoelastic nature of connective tissue.1–3,13 This viscoelasticity is the very characteristic that makes connective tissue able to change based on the stresses applied to it. The ability of connective tissue to thicken or become more extensible based on outside stresses is the basic premise to be understood by the manual therapist seeking to increase mobility.
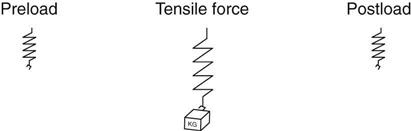
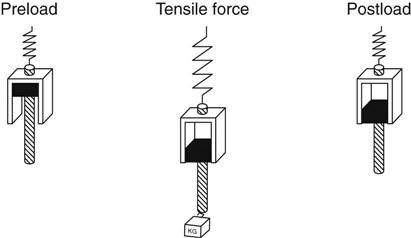
In the viscoelastic model, two components combine to give connective tissue its dynamic deformation attributes. The first is the elastic component, which represents a temporary change in the length of connective tissue subjected to stress (Fig. 2-3). A spring, which elongates when loaded and returns to its original position when unloaded, illustrates this. This elastic component is the “slack” in connective tissue.1–3
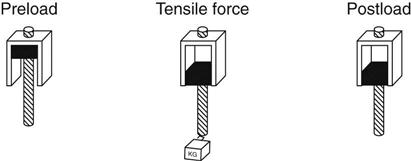
The viscous, or plastic, component of the model represents the permanent change in connective tissue subjected to outside forces. A hydraulic cylinder and piston illustrates this (Fig. 2-4). When a force is placed on the piston, the piston slowly moves out of the cylinder. When the force is removed, the piston does not recoil but remains at the new length, indicating permanent change. These permanent changes result from the breaking of intermolecular and intramolecular bonds between collagen molecules, fibers, and cross-links.1–3
The viscoelastic model combines the elastic and plastic components just described (Fig. 2-5). When subjected to a mild force in the midrange of the tissue, the tissue elongates in the elastic component and then returns to its original length. If, however, the stress pushes the tissue to the end range, then the elastic component is depleted and plastic deformation occurs. When the stress is released, some permanent deformation has occurred. It should be noted that not all the elongation (only a portion) is permanently retained.1–3
Clinically, this phenomenon occurs frequently. For example, a client with a frozen shoulder that has only 90° of elevation is mobilized to reach a range of motion (ROM) of 110° by the end of the treatment session. When the client returns in a few days, the ROM of that shoulder is less than 110° but more than 90°. Some degree of elongation is lost and some is retained.
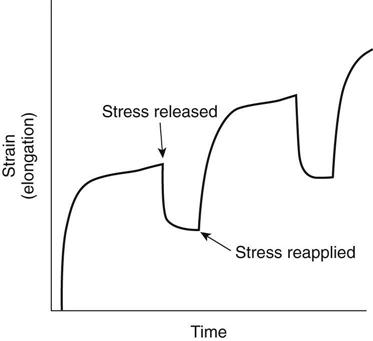
This viscoelastic phenomenon can be further illustrated by the use of stress-strain curves. By definition, stress is the force applied per unit area, and strain is the percent change in the length of the tissue. When connective tissue is initially stressed or loaded, very little force is required to elongate the tissue. However, as more stress is applied and the slack or spring is taken up, more force is required and less change occurs in the tissue (Fig. 2-6). When the tissue is subjected to repeated stresses, the curve shows that after each stress the tissue elongates and then only partially returns to its original length. Some length is gained each time the tissue is taken into the plastic range. This phenomenon is seen clinically in repeated sessions of therapy. ROM is gained during a session, with some of the gain being lost between sessions.1–3
New Developments—Connective Tissue Is Contractile and Dynamic
The older model of connective tissue does not explain completely the quick changes that can occur in connective tissue during manual therapy. Several theories have emerged to explain these quick changes. The most substantial body of literature suggests that connective tissues have a limited contractile ability resulting from the presence of myofibroblasts. Myofibroblasts are differentiated fibroblasts that not only synthesize collagen and ground substance, but also retain the ability to contract. These specialized cells were first recognized to be present in immature scar tissue, and were believed to be responsible for scar tissue shrinkage and contracture.6,7,14–16
More recent literature has documented the presence of both myofibroblasts and smooth muscle fibers in normal connective tissue, including the fascia cruris and the lumbodorsal fascia.16,17 Myofibroblasts contain smooth muscle of type actin and myosin in the cytoplasm of the cell, and therefore respond to the same stimuli that affect smooth muscle.20 Schleip and associates have described several autonomic mechanisms by which connective tissue “tone” can possibly be affected.14,15,18,19
First, manual stimulation of interstitial and Ruffini mechanoreceptors present in connective tissue affect the autonomic nervous system in a way that creates changes in local fluid dynamics through vasodilation of local blood vessels and movement of fresh fluids into the interstitial tissue. Second, stimulation of the autonomic system through tissue mechanoreceptors has the effect of “hypothalamic tuning,” which results in a global decrease of muscle tone. Lastly, autonomic effects from manual work create a localized autonomic response that inhibits smooth muscle cells present in connective tissue and relaxes actin/myosin activity in myofibroblasts that are also present in connective tissue. All three of these basic mechanisms can better explain the relatively immediate changes that are palpable after manual therapy.
As an example, consider the patient who is referred for therapy 4 weeks after rotator cuff repair, who has developed significant capsular tightness of the shoulder, and who is reactive and guarded with passive range of motion. Gentle soft tissue work in the shoulder girdle, including the scapula-thoracic area, lateral scapula, upper trapezius, and the pectoralis major and minor usually result in immediate increases in range of motion and less reactivity from the patient. Mechanical changes in the joint capsule are not likely to have occurred in such a short time to explain the increased range of motion. A more plausible explanation would be that gentle manual work around the shoulder complex created an autonomic response, which in turn relaxed the contractile elements present in the connective tissue.
Effects Of Immobilization, Remobilization, And Trauma On Connective Tissue
Immobilization
Immobilization and trauma significantly change the histology and normal mechanics of connective tissue. A majority of the historic studies in the area of immobilization follow the same basic experimental mode.13,20–27 Laboratory animals are fixated internally for varying periods. The fixation is removed and the animals are then sacrificed. Histochemical and biomechanical analyses are performed to determine changes in the tissue. In some studies, the fixation is removed and the animals are allowed to move the fixated joint for a period before performance of the analysis. This is done to determine the reversibility of the effects of immobilization.28
Macroscopically, fibrofatty infiltrate is evident in the recesses of the immobilized tissue. With prolonged immobilization, the infiltrates develop a more fibrotic appearance, creating adhesions in the recesses. These fibrotic changes occur in the absence of trauma. Histologic and histochemical analyses show significant changes primarily in the ground substance, with no significant loss of collagen. The changes in the ground substance consist of substantial losses of glycosaminoglycans and water. Because a primary function of ground substance is binding water to assist in hydration, the loss of ground substance results in a related loss of water.
Another purpose of ground substance is to lubricate adjacent collagen fibers and maintain a crucial interfiber distance. If collagen fibers approximate too closely, then the fibers will adhere to one another. These cross-links create a series of microscopic adhesions that limit the pliability and extensibility of the tissue (Fig. 2-7). ![]() In addition, collagen that has been immobilized for extended periods of time demonstrates less tissue strength and quicker failure during stress-strain studies and load-to-failure studies.10,25,27,29–33
In addition, collagen that has been immobilized for extended periods of time demonstrates less tissue strength and quicker failure during stress-strain studies and load-to-failure studies.10,25,27,29–33
Furthermore, because movement affects the orientation of newly synthesized collagen, the collagen in the immobilized joints studied was laid down in a more haphazard, “haystack” arrangement. This orientation restricts tissue mobility further by adhering to existing collagen fibers (Fig. 2-8).
Biomechanical analysis reveals that as much as 10 times more torque is necessary to mobilize fixated joints than normal joints. After repeated mobilizations, these joints gradually return to normal. The authors of these studies implicate both fibrofatty microadhesions and increased microscopic cross-linking of collagen fibers in the decreased extensibility of connective tissue.13,20–27
Remobilization
The classic research seems to suggest that mobility and remobilization prevent the haystack development of collagen fibers within ligaments and tendons, as well as stimulate the production of ground substance. When connective tissue is stressed with movement, the tissue rehydrates, collagen cross-links are diminished, and new collagen is laid down in a more orderly fashion.13,20–28,34
Also, the collagen tends to be laid down in the direction of the forces applied and in an appropriate length. In addition, early mobilization leads to enhanced ligament and tendon strength, resistance to tensile forces, greater joint stability, and improved resistance of the ligament to avulsion.4,9,10,25–27,29,31,34–36
Additionally, macroadhesions formed during the immobilization period partially elongate and partially rupture during the remobilization process, increasing the overall mobility of the tissue. Both passive mobilization and active ROM produce similar results.
Trauma
The previously described studies have limited application because they involve the immobilization of normal, healthy joints. To complete this discussion, we must superimpose the effects of trauma and scar tissue on immobilization.
Scar
Scar tissue mechanics differ somewhat from normal connective tissue mechanics. Normal connective tissue is mature and stable, with limited pliability. Immature scar tissue is much more dynamic and pliable. Scar tissue formation occurs in four distinct phases. Each of these phases shows characteristic differences during phases of immobilization and mobilization.1–3
The first phase of scar tissue formation is the inflammatory phase. This phase occurs immediately after trauma. Blood clotting begins almost instantly and is followed by migration of macrophages and histiocytes to start débriding the area. This phase usually lasts 24 to 48 hours, and immobilization is usually important because of the potential for further damage with movement. Some exceptions to routine immobilization exist. For example, in an anterior cruciate ligament (ACL) reconstruction, in which the graft is safely fixated and damage from gentle movement is unlikely, there may be a great advantage in moving the tissue as early as the first day after surgery. Research indicates that early mobilization leads to more rapid ligament regeneration and ultimate load to failure strength in surgically repaired ACLs.32
The second phase of scar tissue formation is the granulation phase. This phase is characterized by an uncharacteristic increase in the relative vascularity of the tissue. Increased vascularity is essential to ensure proper nutrition to meet the metabolic needs of the healing tissue. The granulation phase varies greatly depending on the type of tissue and the extent of the damage. Generally speaking, the entire process of scar tissue formation is lengthened if the damaged tissue is less vascular in its nontraumatized state. For example, tendons and ligaments require more time for scar tissue formation than muscle or epithelial tissue. Movement is helpful in this phase, although the scar tissue can be easily damaged. The physician and therapist need to work closely to determine the extent of movement relative to the risk.
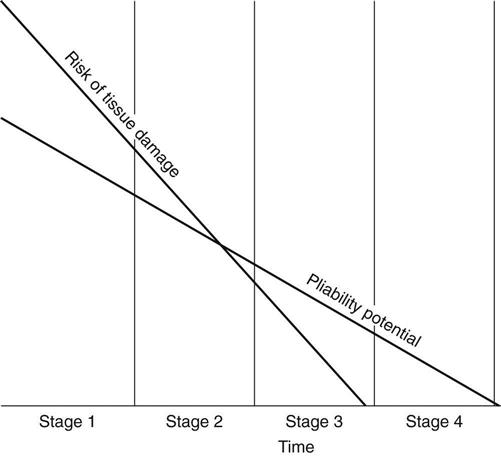
The third phase of scar tissue formation is the fibroplastic stage. In this stage the number of fibroblasts increases, as does the rate of production of collagen fibers and ground substance. Collagen is laid down at an accelerated rate and binds to itself with weak hydrostatic bonds, making tissue elongation much easier. This stage presents an excellent window of opportunity for the reshaping and molding of scar tissue without great risk of tissue reinjury. This stage lasts 3 to 8 weeks, depending on the histologic makeup and relative vascularity of the damaged tissue. Scar tissue at this phase is less likely to be injured but is still easily remodeled with stresses applied (Fig. 2-9). Additionally, myofibroblasts are the most active in the last two phases of scar tissue maturation. Myofibroblasts are believed to be responsible for the scar tissue shrinkage that occurs in this and the next phase of scar tissue healing.1,3,6–8,37
The final phase of scar tissue formation is the maturation phase. Collagen matures, solidifies, and shrinks during this phase. Maximal stress can be placed on the tissue without risk of tissue failure. Because collagen synthesis is still accelerated, significant remodeling can take place when appropriate mobilizations are performed. Conversely, if they are left unchecked, then the collagen fibers can cross-link and the tissue can shrink significantly. At the end of the maturation phase, tissue remodeling becomes significantly more difficult because the tissue reverts to a more mature, inactive, and nonpliable status.
Surgical Perspective
Surgery has been defined in this chapter as controlled trauma produced by a trained professional to correct uncontrolled trauma. Postsurgical cases are subject to the effects of immobilization, trauma, and scar formation. However, they have the advantage of resulting from controlled trauma. The scar tissue formed by surgery is usually more manageable than scar tissue formed by uncontrolled trauma or overuse.
When dealing with scar tissue after surgery, the physical therapist should remember the following guidelines:
• Whenever possible, early movement is helpful in controlling the direction and length of the scar tissue. ![]() Communicate with the referring physician regarding the amount of movement that is appropriate. In a study performed by Flowers and Pheasant,38 casted joints regained mobility much faster than fixated joints. This is probably because a cast does not provide the same immobilization as rigid fixation. The small amounts of movement allowed in casted joints may be enough to prevent some of the changes caused by rigid fixation.
Communicate with the referring physician regarding the amount of movement that is appropriate. In a study performed by Flowers and Pheasant,38 casted joints regained mobility much faster than fixated joints. This is probably because a cast does not provide the same immobilization as rigid fixation. The small amounts of movement allowed in casted joints may be enough to prevent some of the changes caused by rigid fixation.
• Recognize the window of opportunity to stress scar tissue, and keep in mind the associated risk of tissue injury or microtrauma (see Fig. 2-9). Although the potential to change scar tissue may be greater in earlier stages, the risk of damage is higher. The third stage appears to be the stage at which the reward of mobility work exceeds the risk.
• Recognize that even the gentlest and soothing of soft tissue mobilizations can positively affect the autonomic nervous system,39 and can relax the contractile element present in these tissues. This gentle, autonomic effect has minimal risk and great potential reward. Touch your patients!
Goals Of Mobility Work
In 1945 John Mennell wrote, “There are only two possible effects of any movement or massage: they are reflex (autonomic) and mechanical.”36 The following summary emphasizes the goals of the mechanical and autonomic changes of mobility work:
• Mobility work causes the breaking and subsequent prevention of cross-links in collagen fibers.
• Mobility work allows for the breaking and prevention of macroadhesions.
• Mobility work allows for the plastic deformation and permanent elongation of connective tissue.
• Mobility work prevents scar tissue shrinkage through both mechanical and autonomic mechanisms.
Principles For Mobilization Of Connective Tissues
This section attempts to integrate the principles of basic scientific research and years of clinical experience into a series of techniques useful for the physical therapist in treating immobilized tissue.
Three-Dimensionality of Connective Tissue
Connective tissue is three-dimensional. Especially after trauma and immobilization, the scar tissue can follow lines of development not consistent with the kinesiology or arthrokinematics of the area. Therefore the ability to feel the location and direction of the restriction becomes important in the mobilization of scar tissue.
Creep
Creep is another term for the plastic deformation of connective tissue. Active scar tissue is more “creepy” than normal connective tissue (i.e., it is more easily elongated by external forces).2 Creep occurs when all the “slack” has been let out of the tissue. It is best accomplished with low-load, prolonged stretching but also can be accomplished with other manual techniques. Dynamic splinting is another technique used to elongate connective tissue. The tissue should be elongated along the lines of normal movement; however, at times the restrictive lesion may not follow the line of movement. The therapist must identify the direction of the restriction and mobilize directly into the restriction. The scar may be a transverse or horizontal plane. Mobilizing the scar in the direction of the restriction usually results in more movement along conventional planes.1,3
The Contractile Characteristic of Soft Tissues
As previously mentioned, connective tissues have a contractile element by virtue of the presence of smooth muscle cells and myofibroblasts. Instantaneous “creep” is an autonomic phenomenon.14,15 Gentle manual work, through stimulation of mechanoreceptors, can create the autonomic effect of relaxation, resulting in increased pliability of connective tissue, increased range of motion, and decreased pain.
Principle of Short and Long
The principle of short and long is the idea that tissues mobilized in a shortened range often become more extensible when they are immediately elongated (Fig. 2-10). For example, in a lateral epicondylitis, cross-friction massage may be performed over the lateral epicondyle with the elbow passively flexed and the wrist passively extended. Immediately after the cross-friction in the shortened range, the tissue is stretched into the plastic range. In the shortened range, deeper tissue can be accessed. When tissue is taut, only the more superficial layers can be accessed. When the tissue has some slack, the deeper tissue can be accessed and prepared for stretching.2
The principle of short and long has neuromuscular implications as well. If a muscle is guarded, then shortening the muscle by mobilizing it has an inhibitory effect that makes immediate elongation easier.
Sample Techniques For Mobilization Of Connective Tissues
The following techniques and associated photographs illustrate some examples of simple manual techniques effective in mobilizing soft tissue.
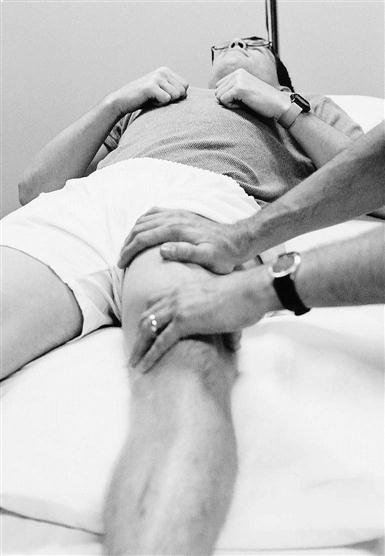
Muscle Splay
Muscle splay is a term that implies a widening or separation of longitudinal fibers of muscle or connective tissue that have adhered to one another (Fig. 2-11). These adhesions limit the ability of the tissue to be lengthened passively or shortened actively. When muscle bundles or connective tissue bundles stick together, the muscle fibers become less efficient in their contractions. For example, muscle splay in the wrist flexors often produces a slightly greater grip strength immediately after soft tissue work. This is not greater strength, but greater muscle efficiency produced by increased soft tissue pliability. The muscle can contract more efficiently within its connective tissue compartments.2
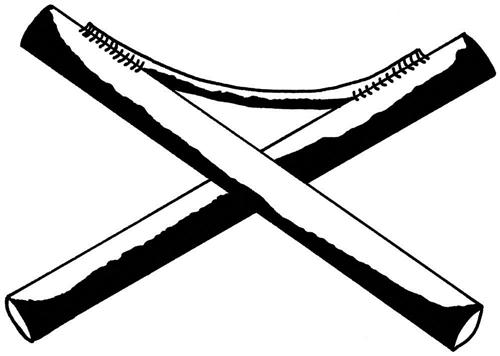
Transverse Muscle Bending
Transverse muscle bending takes the contractile unit and mobilizes it perpendicular to the fibers (Fig. 2-12). This perpendicular bending mobilizes connective tissue in a way similar to the bending of a garden hose (Fig. 2-13). The connective tissue sheath surrounding a muscle may be likened to the hose itself, with the muscle being analogous to the water inside it. If the connective tissue sheath is stiff and rigid, then the muscle inside has difficulty contracting. The unforgiving sheath does not allow the muscle to expand transversely, creating a lack of efficiency and a low-grade “compartment syndrome.” By mobilizing these muscle sheaths, overall mobility is enhanced along planes of normal movement.2
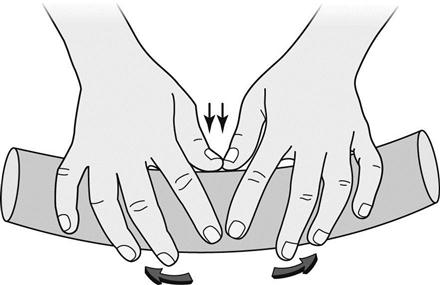
Additionally, muscle bending specifically stimulates the Ruffini type mechanoreceptor. Ruffini endings are particularly sensitive to lateral/transverse type stretching. This type of stretching, therefore, has the autonomic effect of decreasing sympathetic tone in the “garden hose,” creating greater connective tissue pliability.14,15
Bony Clearing
Bony clearing is similar to muscle splay, except the mobilization is applied longitudinally along the soft tissue that borders or attaches to a bony surface (Fig. 2-14). A good example of this is longitudinal stroking of the anterior lateral border of the tibia in conditions such as shin splints. The connective tissue along the border of the tibia thickens and becomes adhered, and the therapist attempts to mobilize the tissue in this plane.2
Cross-Friction
Cross-friction massage, which was developed and advocated by the late James Cyriax, is excellent for mobilizing scar tissue and nonvascular connective tissue. It is an aggressive form of soft tissue mobilization designed to break scar tissue adhesions and temporarily increase the blood flow to nonvascular areas. Ligaments and tendons struggling to heal completely are excellent candidates for cross-friction massage. This technique can be used on scar tissue as well, and it should be performed at many different angles to access fibers in all directions.2
Muscle Balancing
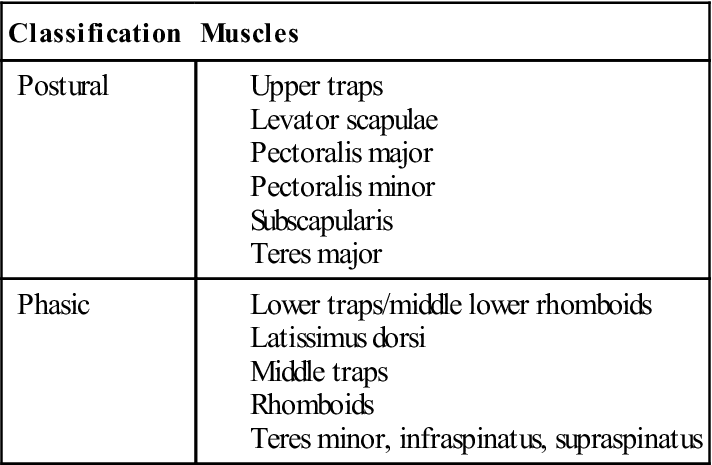
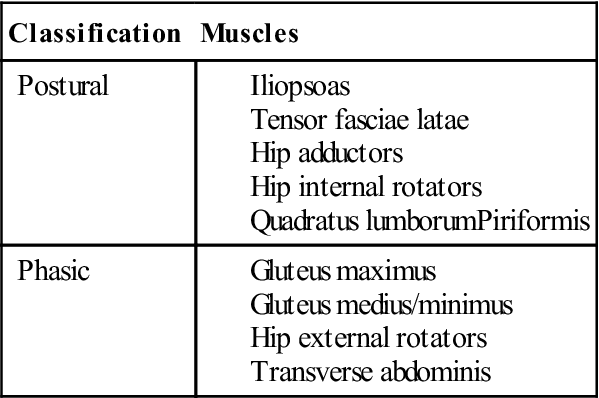
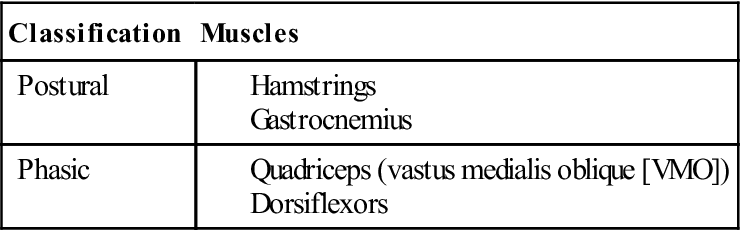
As connective tissue pliability is increasing through manual therapy and passive range of motion, attention is also given to active range of motion and strengthening. Individual muscles surrounding joints can be grouped together according to their response to dysfunction. Typically, postural muscles respond to injury, abnormal stress, and surgery by tightening or becoming facilitated. Phasic muscles tend to respond to injury, abnormal stress, and surgery by weakening or becoming inhibited.2
Each joint complex in the body has groups of muscles that are dedicated to functioning as stabilizers and muscles that function as prime movers. For example, it is well known that the vastus medialis oblique (VMO) at the knee functions to stabilize the patella during knee flexion and extension. It is also well known that the VMO, along with the other three quadricep muscles, responds to dysfunction by weakening, becoming inhibited, and displaying atrophy. Conversely, the hamstring muscle group responds to dysfunction by tightening.2
During postsurgical rehabilitation, the therapist should expect to provide manual treatment for the postural muscles that act on the involved joint and strengthen (when healing constraints permit) the phasic muscles that have invariably weakened. A prime example is the shoulder after rotator cuff surgery. Initially, during the acute and protective phases of rehab, the therapist should treat levator scapulae, trapezius, subscapularis, teres major, and pectoralis minor (all postural muscles that act on the shoulder complex). After the patient enters into the active phase of rehab, efforts should be shifted to strengthening of the external rotators, lower traps, rhomboids, and serratus anterior (all phasic muscles that stabilize the shoulder complex).2
Tables 2-2 to 2-4 illustrate and summarize the groupings of postural and phasic muscles by region, and agonist-antagonist relationships.
TABLE 2-2
Classification of Postural and Phasic Muscles of the Shoulder
< ?comst?>
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
From Cantu R, Grodin A: Myofascial manipulation: Theory and clinical application, Gaithersburg, Md, 1992, Aspen.
TABLE 2-3
Classification of Postural and Phasic Muscles of the Hip
< ?comst?>
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
From Cantu R, Grodin A: Myofascial manipulation: theory and clinical application, Gaithersburg, Md, 1992, Aspen.
TABLE 2-4
Classification of Postural and Phasic Muscles of the Knee
< ?comst?>
< ?comen?>< ?comst1?>
< ?comst1?>
< ?comen1?>
From Cantu R, Grodin A: Myofascial manipulation: Theory and clinical application, Gaithersburg, Md, 1992, Aspen.
Summary
This chapter outlines the basic principles and guidelines for soft tissue management after surgery and discusses the stages of scar tissue formation. ![]() The time frames for these stages are variable based on the vascularity of the tissue and the surgical procedure performed. They are delineated in more detail in the following chapters.
The time frames for these stages are variable based on the vascularity of the tissue and the surgical procedure performed. They are delineated in more detail in the following chapters.
The physical therapist must understand connective tissue responses to immobilization, trauma, remobilization, and scar remodeling to treat injured tissue effectively. Additionally, the therapist should be aware of the global and specific autonomic effects of manual therapy that affect tissue contractility. Awareness of both mechanical and autonomic principles of soft tissue management, along with good physician-client communication, ensures consistently effective management of postsurgical rehabilitation.
Clinical Case Review
1 What is the mechanism by which ROM is achieved during a session of manual therapy?
Stimulation of the autonomic nervous system through manual stimulation of interstitial and Ruffini mechanoreceptors has the effect of “hypothalamic tuning,” which results in a global decrease of muscle tone.
2 Why is it important to be respectful of the connective tissue following immobilization?
During immobilization collagen fibers become dehydrated, and if collagen fibers approximate too closely, then the fibers will adhere to one another. These cross-links create a series of microscopic adhesions that limit the pliability and extensibility of the tissue. In addition, collagen that has been immobilized for extended periods of time demonstrates less tissue strength and quicker failure during stress-strain studies and load-to-failure studies.
3 At what point is it advisable to stress scar tissue?
There is a window of opportunity to stress scar tissue. Keep in mind the associated risk of tissue injury or microtrauma if the scar tissue is overstressed in its immature stage. Although the potential to change scar tissue may be greater in earlier stages, the risk of damage is higher. The third stage (fibroplastic) appears to be the stage at which the reward of mobility work exceeds the risk. This stage lasts 3 to 8 weeks depending on the histologic makeup and relative vascularity of the damaged tissue.