29 Skin Resurfacing with Ablative Lasers
Ablative laser resurfacing is one of the most effective therapies available for wrinkle reduction. This is an aggressive method of skin resurfacing whereby water in the skin is heated and vaporized by laser energy, causing a controlled injury to the epidermis and dermis. It is most commonly performed using either carbon dioxide (CO2) or erbium:yttrium aluminum garnet (Er:YAG) lasers. Traditional ablative laser resurfacing deeply penetrates the skin (up to 300 µm), and because the epidermis is fully ablated, it is associated with prolonged recovery times, and may have serious complications of infection, hypopigmentation, and scarring1 and, hence, is rarely performed today. Less aggressive superficial ablative treatments (ranging in depth from 20 to 50 µm) are still commonly performed, particularly for reduction of dyschromia and mild wrinkles.2 Superficial ablative laser resurfacing is also referred to as a laser peel.
In 2004, a novel method of fractional resurfacing, which involves treating only a portion or “fraction” of the skin, was introduced.3 Fractional devices deliver laser energy to the skin in microscopic columns, also called microthermal zones. This delivery method allows for very deep penetration in the skin (up to 1.5 µm). Figure 29-1 shows a comparison between deep fractional microthermal zones and “conventional” horizontal plane resurfacing.
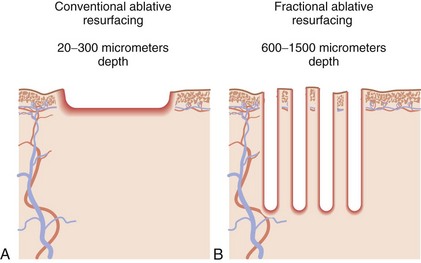
FIGURE 29-1 Ablative laser patterns of injury: (A) conventional “horizontal plane” and (B) fractional.
The untreated adjacent tissue between microthermal zones serves as a reservoir of regenerative cells that migrate into the treatment area and facilitate rapid wound healing. Fractional ablative resurfacing has been shown to effectively reduce wrinkles and improve dyschromia in photoaged skin and has the advantages of reduced recovery time and reduced risks compared to conventional ablative laser resurfacing.4–6
Laser Principles
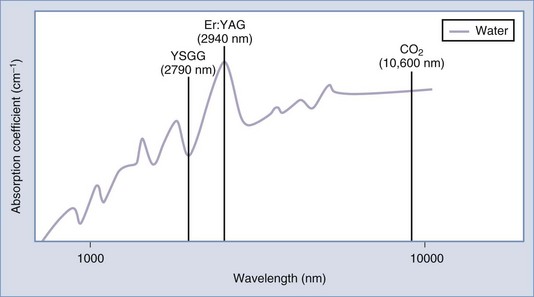
Ablative lasers achieve wrinkle reduction through the use of water as the target chromophore to heat and vaporize tissue. The two main laser wavelengths used for ablative resurfacing, 2940 nm (Er:YAG) and 10,600 nm (carbon dioxide), are well absorbed by water. A third, less frequently used wavelength is 2790 nm (yttrium scandium gallium garnet or YSGG). Figure 29-2 shows the water absorption spectrum and these three ablative resurfacing lasers. Note that the erbium 2940 nm wavelength is at a water absorption peak and is approximately 15 times more highly absorbed by water than CO2.
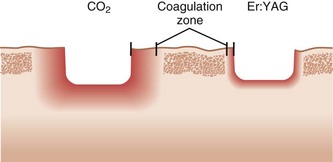
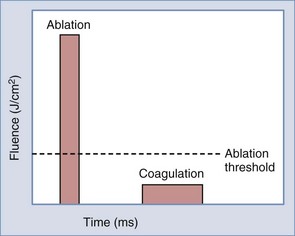
Absorbed laser energy has two main effects on tissue: (1) removal of tissue, called ablation, and (2) heat transference to surrounding tissue, called coagulation. Coagulation clinically results in tissue tightening. A controlled amount of coagulation with treatments is, therefore, desirable but too much thermal injury can be associated with complications such as hypopigmentation and scarring. Due to a greater absorption by water, Er:YAG lasers ablate tissue at lower fluences (approximately 1 J/cm2), compared to CO2 lasers, which require higher fluences to achieve similar ablation (approximately 5 J/cm2). Er:YAG lasers, therefore, cause less thermal damage to the surrounding tissues and have smaller zones of coagulation than CO2 lasers. Figure 29-3 shows the zones of coagulation around a region of ablation with a CO2 versus an erbium laser. The amount of ablation and coagulation is controlled by laser fluence and pulse width (see Chapter 19, Aesthetic Principles and Consultation, for a discussion of laser parameters). Ablation is most effectively achieved with short pulse widths and high fluences, whereas coagulation is achieved with longer pulse widths and lower fluences (Figure 29-4). By varying these two parameters, ablative laser devices can independently control the amounts of ablation and coagulation achieved.
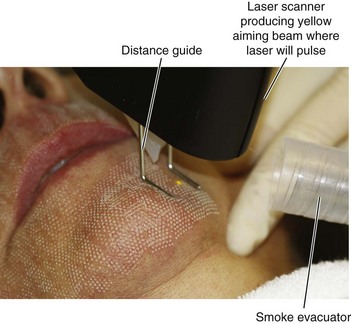
Laser fluence is also a major determinant of the depth of injury with fractional ablative devices, where higher fluences penetrate deeper. Density settings control the percentage of skin that is treated. More aggressive fractional ablative treatments are, therefore, achieved with high fluences and high density parameters. Some fractional devices utilize scanners and computer software to “randomly” deliver pulses within a set pattern so that the pulses are not adjacent to one another. Changing the energy delivery pattern from sequential to nonadjacent pulses allows for high energies to be delivered without the effects of bulk heating.7 This is particularly useful with CO2 devices which cause greater thermal injury.
In summary, fractional ablative laser devices have variable fluences, spot sizes, spot densities, and pulse widths, all of which affect the depth of penetration as well as the degree of ablation and coagulation achieved.8 Because these devices are still relatively new, clinical correlation is required to determine how these different parameters impact results, downtime, and side effects.
Patient Selection
Fitzpatrick skin type classification is an important factor in assessing patients for laser resurfacing (see Chapter 19, Aesthetic Principles and Consultation, for skin type classification). The ideal patient has a fair complexion (Fitzpatrick types I through III) with lesions responsive to laser ablation (see the Indications section below). Patients with darker complexions (Fitzpatrick types IV and V) may be treated as well, but must be informed about their higher risk for pigmentary complications and the need for more cautious treatment parameters, which may limit results. Although patients with Fitzpatrick skin type V may be candidates, in reality these patients rarely present with the facial aging signs that patients with lighter skin types complain of, and one rarely encounters such a patient seeking facial resurfacing. It is advisable for providers getting started with fractional ablative resurfacing to limit treatments to lighter skin types (I through III).
Indications9,10
Ablative laser resurfacing has traditionally been used for patients with more advanced signs of facial aging (Glogau stage IV) including generalized static wrinkles, keratoses, severe dyschromia, sallow color, and coarse pores (see Chapter 19 for a discussion of the Glogau photoaging scale). With the advent of fractional technologies that have more rapid recovery times and fewer risks, ablative laser procedures are being performed in patients with less severe photoaging. Nonetheless, the most common indication today for fractional ablative laser resurfacing is still moderate to severe wrinkles as well as scars.
Alternative Therapies
Skin resurfacing can also be accomplished by mechanical exfoliation procedures such as microdermabrasion and chemical peeling treatments which typically penetrate to the epidermis or upper reticular dermis (see Chapter 22, Chemical Peels and Chapter 23, Microdermabrasion). Dermabrasion is a mechanical, “cold steel” method of removing epidermis, papillary, or upper reticular dermis. Dermabrasion and chemical peeling have the advantage of being less expensive than laser resurfacing. However, extensive hands-on experience in a preceptor environment is required in order to learn the art of dermabrasion.11
Products Currently Available
See the Resources section at the end of the chapter for a list of manufacturers of devices that have these wavelengths.
Contraindications
See the General Laser Contraindications section in Chapter 26, Hair Reduction with Lasers. Additional contraindications include the following:
Disadvantages of Laser Resurfacing
Equipment
Anesthesia—Intraoral Nerve Blocks
Anesthesia—Assistive External Device
See Chapter 20, Anesthesia for Cosmetic Procedures, and Chapter 3, Anesthesia, for more information.
Procedure Preparation
One Month Prior
Preprocedure Skin Care Products
Preprocedure products typically contain retinoids, alpha hydroxy acids, antioxidants such as vitamin C, sunscreens, and, for patients prone to hyperpigmentation, skin lightening agents such as hydroquinone or a cosmeceutical such as kojic acid, arbutin, niacinamide, or azelaic acid are also used.13 The goal for using these products is to condition the skin and create a healthier pretreatment epidermis and dermis, thereby promoting more rapid healing postprocedure. Although prescription-strength retinoids have traditionally been used preprocedure,14 some physicians recommend using less irritating retinoids such as retinol or retinaldehyde.15
Preprocedure skin care for ablative laser treatments should be started 1 month prior to the procedure and discontinued 1 week prior to the procedure to ensure a fully intact epidermis at the time of treatment. In darker Fitzpatrick skin types (III or higher), topical lightening agents, such as hydroquinone 4% to 8%, are commonly used pretreatment (see Chapter 24, Skin Care Products, for preprocedure treatment regimes).
One Week Prior
Fractional Ablative Laser Resurfacing: Steps and Principles
General Treatment Technique
Planning and Designing
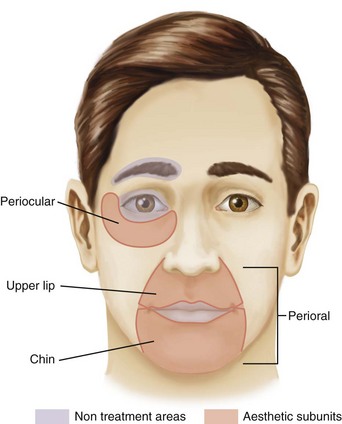
Ablative laser resurfacing may be performed to a region of the face or to the entire face. Figure 29-5 shows three of the most commonly treated facial aesthetic subunits (modified from Gonzales-Ulloa16). The periocular subunit is bounded inferiorly by the crest of the zygoma and superiorly by the orbital rim. The upper lip subunit extends laterally to the nasolabial folds and superiorly to the nose. The chin subunit extends along the line of the nasolabial fold inferiorly, below the jaw line. The perioral subunit includes the upper lip and chin subunits.
Anesthesia
Types of anesthesia used for fractional ablative resurfacing include:
See Chapter 20, Anesthesia for Cosmetic Procedures, for more information.
Safety Zone
The Fractional Ablative Laser Safety Zone for treatments on the face includes the entire face apart from the area within the orbital rims, eyebrows, and the lips (Figure 29-5). Providers with advanced ablative laser skills may choose to treat over the eyelids with conservative settings using intraocular lead eye shields. However, it is recommended that providers getting started with this procedure restrict their treatment to the area outside of the orbital rim.
Performing Fractional Ablative Laser Resurfacing

FIGURE 29-7 Clinical endpoints for fractional ablative resurfacing of pinpoint bleeding and erythema.
(Copyright Rebecca Small, MD.)
TIP: Lasers used with pure ablation and no coagulation are more likely to cause bleeding.
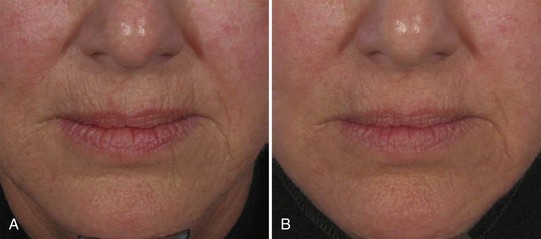
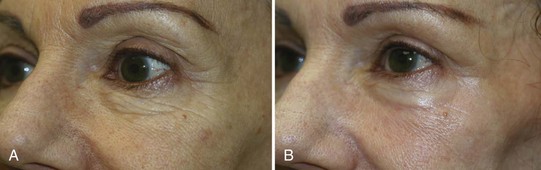
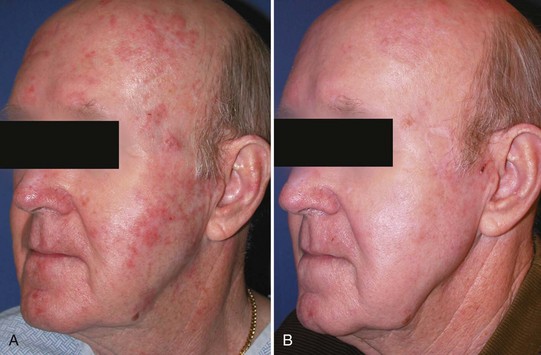
Results
Fractional ablative lasers (CO2 and Er:YAG) can significantly improve wrinkles and hyperpigmentation in photoaged skin.4,5,18–20 Wrinkle reduction can be seen in the immediate post-treatment period, once re-epithelialization occurs, and continues to improve up to 6 months after treatment. The presumed mechanism for textural improvement is through thermally induced collagen denaturation and shrinkage immediately after treatment, with delayed fibroblast proliferation and synthesis of new collagen, also called dermal collagen remodeling.21
Laser resurfacing also plays an important role in reduction of scars. Blending scar borders with the surrounding skin, and improving pigment changes in the scar can help achieve excellent camouflage. Fractional ablative lasers have showed success with scar reduction, primarily atrophic acne scars.22,23
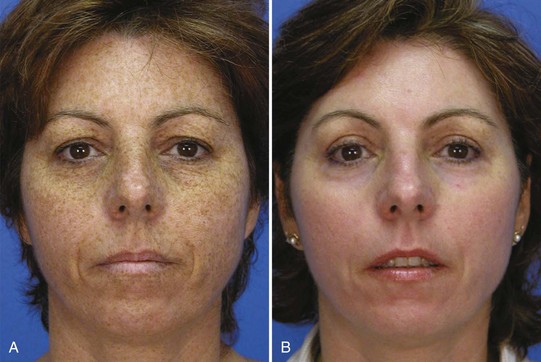
Figure 29-9 shows the results of deep ablative laser resurfacing for facial wrinkles (A) before and (B) after one treatment using an erbium laser to a 120 µm depth (Sciton Contour TRL™).
Figure 29-10 shows the results of fractional ablative laser resurfacing for facial wrinkles (A) before and (B) after one treatment using a carbon dioxide laser (Fraxel Re:pair™).
Figure 29-11 shows the results of fractional ablative laser resurfacing for facial wrinkles and pigmentation (A) before and (B) after one treatment using a carbon dioxide laser (Fraxel Re:pair™).
Figure 29-12 shows the results of fractional ablative laser resurfacing for perioral wrinkles (A) before and (B) after one treatment using a carbon dioxide laser (Lumenis TotalFX™).
Figure 29-13 shows the results of fractional ablative laser resurfacing for facial wrinkles (A) before and (B) after one treatment using an erbium laser (Sciton Profractional-XC™).
Figure 29-14 shows the results of fractional ablative laser resurfacing for periocular wrinkles (A) before and (B) after one treatment using an erbium laser (Palomar Lux2940™).
Figure 29-15 shows the results of fractional ablative laser resurfacing for acne scarring (A) before and (B) after five treatments using an erbium laser (Sciton Profractional-XC™).
Figure 29-16 shows the results of fractional ablative laser resurfacing for actinic keratoses (A) before and (B) after two treatments using an erbium laser (Sciton Profractional™).
Figure 29-17 shows the results of superficial ablative laser resurfacing for solar lentigines (A) before and (B) after one treatment using an erbium laser to a 50-µm depth (Sciton Contour TRL™ MicroLaserPeel™).
Figure 29-18 shows the results of precision ablative laser resurfacing for seborrheic keratoses (A) before and (B) after one treatment using an erbium laser (HOYA ConBio Dermasculpt™ Chisel Touch™).
Aftercare
Fractional ablative laser treatments have two distinct phases of healing:
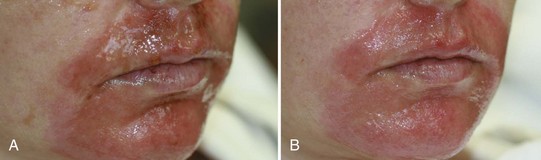
The open wound stage starts from the time of treatment and persists until full re-epithelialization takes place. This typically takes 4 to 7 days, with erbium lasers trending toward shorter recovery times.24 Figure 29-19 shows the recovery process for a fractional ablative erbium laser resurfacing treatment on the face of a 41-year-old woman 1 day postprocedure (Figure 29-19A), where the treatment area is an open wound with intense erythema, some serous oozing, crusting, and pinpoint bleeding. By the fourth postprocedure day (Figure 29-19B), the treatment area is almost fully re-epithelialized, showing mild erythema with a few open areas. On day 5, this patient had fully re-epithelialized.
Open wound care consists of gentle rinsing of the treatment area with dilute acetic acid (vinegar) soaks several times a day (see the patient information handout titled Fractional Ablative Laser Resurfacing in Appendix A). Some providers alternatively use gentle facial rinsing with warm soapy water several times a day. Figure 29-20 shows a patient the day after fractional ablative erbium resurfacing (A) prior to and (B) immediately after a vinegar cleanse. Note the devitalized, brown tissue and crusting has been removed to reveal healthy pink tissue after cleansing. Pinpoint bleeding may occur during the cleansing process, which is not undesirable. Cleansing is followed by application of an occlusive ointment such as Aquaphor, Crisco,25 or Primacy to promote moist wound healing. Some providers use nonocclusive products that promote wound healing, such as Biafine, during this phase.26 Excessive or prolonged use of occlusive topical products may increase the risk of milia, folliculitis, acne, and bacterial or candidal infections, whereas too little product may result in crusting and delayed re-epithelialization. During the open wound phase, no sunscreen or makeup is worn and strict sun avoidance is imperative to reduce the risk of hyperpigmentation.
See the Preprocedure and Postprocedure Products section in Chapter 24, Skin Care Products, for more information about postprocedure skin care.
Follow-Up
Regular, frequent follow-up is advised initially to monitor the healing progress as well as to identify any early complications.27 During the open wound phase in the first week, it is recommended that the patient be seen on postprocedure day 1 or 2, to evaluate the wound and ensure adherence to proper home care. A visit at 1 week is recommended to assess for full re-epithelialization, and once this is observed, the postepithelialization stage has begun and the patient may be transitioned to nonocclusive postcare topical products. If recovery is uneventful, the follow-up schedule may be 1 month and 3 months postprocedure. Any concerns or problems warrant more frequent visits.
Complications
Despite the advances of fractional technologies that have increased safety and shortened recovery with ablative lasers, clinicians must remember that fractional ablative lasers can be associated with complications. An open wound is created with these treatments and complications such as infection and scarring can and do occur. Most of the complications with fractional ablative lasers to date have been reported in thin-skinned areas, such as under the eye, and in nonfacial areas, such as the neck.27 Early recognition of complications allows the physician to initiate appropriate treatments that can help reduce the risk of permanent damage. The following discussion reviews complications and management of complications reported with ablative laser treatments, with fractional and nonfractional devices.
Erythema and edema are normal signs after laser resurfacing and are considered abnormal if they persist longer than the expected period. Postprocedure erythema after re-epithelialization is usually mild in intensity and is resolved by 1 month. By comparison, nonfractional deep ablative lasers routinely resulted in prolonged erythema for 3 to 6 months after treatment. In general, postoperative erythema following CO2 laser treatments lasts longer than with erbium lasers, due to the greater thermal damage from CO2. Prolonged erythema lasting past 1 month and intense erythema lasting past 1 week should be considered unusual and addressed. Persistent erythema may indicate impending scar formation or may be due to contact dermatitis to topical compounds used during the recovery phase. If an impending scar is suspected, a strong class I topical corticosteroid should be applied12 (see the discussion of hypertrophic scarring later in this section for additional scar therapies). If contact dermatitis is suspected, all topical medications should be discontinued and topical corticosteroids used. A history of rosacea may predispose to persistent postoperative erythema.12,28
Postoperative contact dermatitis is usually irritant in nature.31–33 Newly resurfaced skin is vulnerable to irritation from various substances found in topically prescribed ointments, preservatives, sunscreens, and fragrances. In addition, topical antibiotics such as bacitracin, Neosporin (bacitracin zinc, neomycin sulfate, and polymyxin B sulfate), and Polysporin (bacitracin zinc and polymyxin B combinations) are common sources of irritation after laser resurfacing. Thus, their use should be avoided in the immediate postoperative period. Finally, many patients may self-prescribe various over-the-counter herbal and vitamin remedies, including vitamin E or aloe products, which can contribute to the problem. Contact dermatitis should be suspected if a patient develops worsening erythema or pruritus after treatment. To decrease this risk, moisturizers without active ingredients should be used during the first postoperative month. If contact dermatitis is suspected, all topical agents should be stopped and mild topical corticosteroids and cool, wet compresses applied regularly. In severe cases, oral antihistamines or short courses of oral corticosteroids may be necessary to control inflammation and reduce fibrosis risk.
Acne flare-ups are relatively common after laser resurfacing due to application of occlusive ointments, especially in patients who are acne prone.29–31 These usually develop within the first few weeks in patients with a strong history of acne, and in other patients may be delayed. Often, no treatment is necessary since the flare-ups are usually mild and resolve once ointments are discontinued. If acne persists despite the discontinuation of occlusive ointments, an oral antibiotic such as doxycycline or minocycline may be used or topical antibiotics such as clindamycin may be used with fully re-epithelialized skin.
Infections can be viral, bacterial, or fungal and usually develop during the first postoperative week.34 The appearance of infections in nonintact resurfaced skin does not always have the characteristic signs seen with intact skin. It is advisable for providers to have a low threshold for culturing areas suspected of infection.
The most frequent infectious complication following ablative laser resurfacing is reactivation of herpes simplex virus (HSV), reported in 2% to 7% of patients, even in those who receive antiviral prophylaxis.35,36 Because there is a high incidence of latent HSV infection, many providers use prophylaxis with all patients undergoing facial laser resurfacing with oral antiviral medications. Acyclovir, famciclovir, or valacyclovir is routinely given 2 days before laser treatment and continued for another 3 to 10 days. Symptoms of HSV infection include tingling, burning, or discharge from isolated areas in the treated areas. Characteristic grouped vesicles may be difficult to recognize in the early postoperative period because there is no intact epithelium. Instead, one may see small superficial erosions. If a herpetic outbreak occurs despite prophylaxis, consider switching to a different antiviral medication or increase the dosage to maximal herpes zoster doses (acyclovir 800 mg 5 times a day, or famciclovir/valacyclovir 500 mg 3 times a day).
Bacterial and fungal infections can also occur because the moist environment of resurfaced skin presents an ideal medium for overgrowth of opportunistic pathogens. The most common bacterial infections are streptococcal, staphylococcal, or Pseudomonas aeruginosa. Fungal infections can be difficult to diagnose because they may resemble acne or milia in nonintact skin. Pain, increased erythema, purulent discharge, crusting, or delayed wound healing should alert one to possible bacterial or fungal infections. It is advisable to obtain wound cultures and initiate antibiotics against the common pathogens prior to obtaining culture results. Infections must be treated aggressively since local spread can lead to permanent scarring, significant morbidity and in severe cases can become disseminated infections. Some providers routinely use antibiotics as part of their perioperative regimen. However, there is no evidence supporting this practice, and indiscriminate antibiotic use may favor drug resistance and promote superinfection by other opportunistic pathogens.37
Postinflammatory hyperpigmentation may develop as postprocedure erythema resolves. It is usually seen within the first month postprocedure and spontaneously resolves during the next several months. Various treatments can be initiated to speed this resolution. Topical agents such as retinoic, azelaic, and glycolic acid compounds, hydroquinone preparations, or light glycolic acid peels (e.g., 30% to 40%) can be used after the first postoperative month.12 It is also important to continue application of a broad-spectrum sunscreen (SPF 30 or higher) to help prevent and limit hyperpigmentation worsening.
Delayed onset hypopigmentation is a potentially serious and permanent complication that has been reported with ablative laser resurfacing.38 Figure 29-21 shows a patient with hypopigmentation 20 years after receiving nonfractional deep ablative CO2 resurfacing of the face. Hypopigmentation usually does not present until 6 to 12 months after ablative laser resurfacing. While relative hypopigmentation in certain areas such as the jaw line may be seen infrequently, true hypopigmentation is rare and occurs more often in patients receiving other forms of aggressive resurfacing such as dermabrasion or phenol peeling. To date, there are no reports of isolated hypopigmentation with fractional ablative resurfacing unless scarring has occurred.27

FIGURE 29-21 Hypopigmentation complication 20 years after ablative CO2 resurfacing of the face.
(Copyright Rebecca Small, MD.)
Hypertrophic scarring is an uncommon but serious complication. Factors increasing the risk for hypertrophic scarring include poor technique with overly aggressive laser parameters including high fluences, pulse stacking, excessive pulse overlapping, and high number of passes. Certain locations such as the lower eyelids, mandible, anterior neck, and chest are more susceptible to scarring and should be treated cautiously.27,39 Postoperative contact dermatitis or wound infection can also lead to scarring if not treated appropriately. Finally, recent use of isotretinoin, previous irradiation, and a history of keloid formation can increase scarring risk.40 Scarring is heralded by focal areas of intense erythema and induration. Early intervention is critical to avoid permanent scarring. Strong class I topical corticosteroids should be applied. Intralesional corticosteroid injections, silicone gel sheeting, and use of the pulsed dye lasers (585 nm) are other treatment options.
Ectropion is another serious complication following laser resurfacing. Prior lower blepharoplasty increases this risk, as does lower lid laxity, which must be ruled out with a “snap test” (see the Procedure Preparation section earlier in this chapter) prior to laser resurfacing. If lower lid laxity exists, it is advisable to avoid laser resurfacing near the lower lid. In general, conservative laser settings and fewer laser passes are employed when treating the lower lids due to the thin nature of the skin. Although topical corticosteroid application, massage, and temporary taping may be tried if ectropion results, often surgical correction is required.
Financial Considerations
Ablative laser resurfacing is not reimbursable by insurance. The charges for treatments vary and are mainly determined by local prices. For example, fees for fractional ablative laser resurfacing in the Northern California Bay Area range from $1800 to $4500 for full face and $800 to $1200 for periocular or perioral areas. Box 29-1 lists applicable codes for ablative laser procedures.
1. Alster TS. Cutaneous resurfacing with CO2 and erbium:YAG lasers: preoperative, intraoperative, and postoperative considerations. Plast Reconstr Surg. 1999;103(2):619-632.
2. Hantash BM, De CE, Liu H, et al. Split-face comparison of the erbium micropeel with intense pulsed light. Dermatol Surg. 2008;34(6):763-772.
3. Manstein D, Herron GS, Sink RK. Fractional photothermolysis: a new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med. 2004;34:426-438.
4. Munavalli G. Single pass fractionated CO2 laser resurfacing of lower eyelid rhytides. Presented at American Society for Laser Medicine and Surgery Conference, April 2008.
5. Lapidoth M, Yagima Odo ME, Odo LM. Novel use of erbium:YAG (2,940-nm) laser for fractional ablative photothermolysis in the treatment of photodamaged facial skin: a pilot study. Dermatol Surg. 2008;34(8):1048-1053.
6. Pozner JN, Glanz S, Goldberg DJ. Fractional erbium resurfacing: histologic and early clinical experience. Lasers Surg Med. 2007;39:S19-S73.
7. Clementoni MT, Gilardino P, Muti GF, et al. Non-sequential fractional ultrapulsed CO2 resurfacing of photoaged facial skin: preliminary clinical report. J Cosmet Laser Ther. 2007;9(4):218-225.
8. Trelles MA, Velez M, Mordon S. Correlation of histological findings of single session Er:YAG skin fractional resurfacing with various passes and energies and the possible clinical implications. Lasers Surg Med. 2008;40(3):171-177.
9. Mehregan A. Actinic keratosis and actinic squamous cell carcinoma: a comparative study of 800 cases observed in 1968 and 1988. Cutan Aging Cosmet Dermatol. 1988;2:151.
10. Tierney EP, Kouba DJ, Hanke CW. Review of fractional photothermolysis: treatment indications and efficacy. Dermatol Surg. 2009;35(10):1445-1461.
11. Mandy SH, Monheit GD. Dermabrasion and chemical peels. In: Papel I, editor. Facial Plastic and Reconstructive Surgery. New York: Thieme; 2009:301-320.
12. Alster TS, Lupton JR. Treatment of complications of laser skin resurfacing. Arch Facial Plast Surg. 2000;2(4):279-284.
13. Weinstein GD, Nigra TP, Pochi PE, et al. Topical tretinoin for treatment of photodamaged skin: a multicenter study. Arch Dermatol. 1991;127:659-665.
14. Lowe NJ, Lask G, Griffin ME. Laser skin resurfacing. Pre- and posttreatment guidelines. Dermatol Surg. 1995;21(12):1017-1019.
15. Sachsenberg-Studer EM. Tolerance of topical retinaldehyde in humans. Dermatology. 1999;199(Suppl 1):61-63.
16. Gonzales-Ulloa M. [Selective regional plastic restoration by means of esthetic unities.]. Rev Bras Cir. 1957;33(6):527-533.
17. Eaglstein NF. Chemical injury to the eye from EMLA cream during erbium laser resurfacing. Dermatol Surg. 1999;25(7):590-591.
18. Waibel J, Beer K, Narurkar V, et al. Preliminary observations on fractional ablative resurfacing devices: clinical impressions. J Drugs Dermatol. 2009;8(5):481-485.
19. Weiss R, Weiss M, Beasly KL. Prospective split face trial of a fixed spacing array computed scanned fractional CO2 laser versus hand scanned 1550-nm fractional for rhytides. Abstract presented at American Society for Lasers Medicine and Surgery Conference, April 2008.
20. Ross V, Swann M, Barnette D. Use of a micro-fractional 2940-nm laser in the treatment of wrinkles and dyspigmentation. Abstract presented at American Society for Lasers Medicine and Surgery Conference, April 2008.
21. Liu H, Dang Y, Wang Z, et al. Laser induced collagen remodeling: a comparative study in vivo on mouse model. Lasers Surg Med. 2008;40(1):13-19.
22. Ortiz A, Elkeeb L, Truitt A, et al. Evaluation of a novel fractional resurfacing device for the treatment of acne scarring. Abstract presented at American Society for Lasers Medicine and Surgery Conference, April 2008.
23. Chapas AM, Brightman L, Sukal S, et al. Successful treatment of acneiform scarring with CO2 ablative fractional resurfacing. Lasers Surg Med. 2008;40(6):381-386.
24. Lomeo G, Cassuto D, Scrimali L, et al. Er:YAG versus CO2 ablative fractional resurfacing: a split face study. Abstract presented at American Society for Lasers Medicine and Surgery Conference, April 2008.
25. Speyer MT, Reinisch L, Cooper KA, et al. Erythema after cutaneous laser resurfacing using a porcine model. Arch Otolaryngol Head Neck Surg. 1998;124(9):1008-1013.
26. Rendon MI, Cardona L, Benitez A. The safety and efficacy of trolamine/sodium alginate topical emulsion in postlaser resurfacing wounds. J Drugs Dermatol. 2008;7(5):S23-S28.
27. Fife DJ, Fitzpatrick RE, Zachary CB. Complications of fractional CO2 laser resurfacing: four cases. Lasers Surg Med. 2009;41(3):179-184.
28. Ruiz-Esparza J, Barba Gomez JM, Gomez de la Torre OL, et al. Erythema after laser skin resurfacing. Dermatol Surg. 1998;24(1):31-34.
29. Graber EM, Tanzi EL, Alster TS. Side effects and complications of fractional laser photothermolysis: experience with 961 treatments. Dermatol Surg. 2008;34(3):301-305.
30. Nanni C. Handling complications of laser treatment. Dermatol Ther. 2000;13:127-139.
31. Nanni C. Postoperative management and complications of laser dioxide laser resurfacing. In: Alster TS, Apfelberg D, editors. Cosmetic Laser Surgery: A Practitioner’s Guide. New York: Wiley-Liss; 1999:37-55.
32. Nanni CA, Alster TS. Complications of carbon dioxide laser resurfacing. An evaluation of 500 patients. Dermatol Surg. 1998;24(3):315-320.
33. Ratner D, Tse Y, Marchell N, et al. Cutaneous laser resurfacing. J Am Acad Dermatol. 1999;41(3 Pt 1):365-389.
34. Sriprachya-Anunt S, Fitzpatrick RE, Goldman MP, et al. Infections complicating pulsed carbon dioxide laser resurfacing for photoaged facial skin. Dermatol Surg. 1997;23(7):527-535.
35. Alster TS, Nanni CA. Famciclovir prophylaxis of herpes simplex virus reactivation after laser skin resurfacing. Dermatol Surg. 1999;25(3):242-246.
36. Monheit GD. Facial resurfacing may trigger the herpes simplex virus. Cosm Dermatol. 1995;8:9-16.
37. Walia S, Alster TS. Laser resurfacing infection rate with and without prophylactic antibiotics. Dermatol Surg. 1999;25:857-861.
38. Weinstein C. Carbon dioxide laser resurfacing. Long-term follow-up in 2123 patients. Clin Plast Surg. 1998;25(1):109-130.
39. Alster TS. Side effects and complications of laser surgery. In: Alster TS, editor. Manual of Cutaneous Laser Techniques. Philadelphia: Lippincott Williams & Wilkins; 2000:175-187.
40. Katz BE, MacFarlane DF. Atypical facial scarring after isotretinoin therapy in a patient with previous dermabrasion. J Am Acad Dermatol. 1994;30(5 Pt 2):852-853.
Buford G. Lasers and pulsed-light devices: skin resurfacing (Chap 53). In Pfenninger JL, Fowler GC, editors: Pfenninger and Fowler’s Procedures for Primary Care, 3rd ed, Philadelphia: Mosby/Elsevier, 2011.
Small R. Ablative modalities for wrinkles. In: Small R, editor. A Practical Guide to Cosmetic Lasers. Philadelphia: Lippincott, 2012.