Skin cancer – Squamous cell carcinoma
Squamous cell carcinoma (SCC) is a heterogeneous disease comprising clinically distinct but histologically similar entities with differing risk factors implicated in their aetiopathogenesis.
Aetiopathogenesis
 chronic actinic damage, accumulating over a lifetime of sun exposure (p. 106); psoralen with ultraviolet A (PUVA) treatment can predispose
chronic actinic damage, accumulating over a lifetime of sun exposure (p. 106); psoralen with ultraviolet A (PUVA) treatment can predispose
 immunosuppression, e.g. in renal transplant patients (p. 57)
immunosuppression, e.g. in renal transplant patients (p. 57)
 X-rays or other ionizing radiation; radiant heat (e.g. from a fire; see erythema ab igne, p. 70)
X-rays or other ionizing radiation; radiant heat (e.g. from a fire; see erythema ab igne, p. 70)
 chronic ulceration and scarring (e.g. a burn, lupus vulgaris or discoid lupus erythematosus, genetic blistering diseases)
chronic ulceration and scarring (e.g. a burn, lupus vulgaris or discoid lupus erythematosus, genetic blistering diseases)
 smoking pipes and cigars (relevant for lip lesions)
smoking pipes and cigars (relevant for lip lesions)
 industrial carcinogens (e.g. coal tars, oils)
industrial carcinogens (e.g. coal tars, oils)
 genetic factors (e.g. albinos, xeroderma pigmentosum, p. 92).
genetic factors (e.g. albinos, xeroderma pigmentosum, p. 92).
Bowen’s disease (in situ squamous cell carcinoma)
Pink or lightly pigmented scaly plaques, up to several centimetres in size, are found on the lower leg or trunk (Fig. 1). Transformation into invasive squamous cell carcinoma is infrequent. Bowen’s disease may resemble discoid eczema, psoriasis or superficial basal cell carcinoma. Histologically, the epidermis is thickened and the keratinocytes are atypical, but not invasive. Small biopsy samples may not be representative of the entire lesion and if there is clinical doubt then larger or excisional biopsies should be undertaken.
Bowen’s disease is treated by cryotherapy, curettage, excision, topical 5-fluorouracil or imiquimod, or photodynamic therapy (p. 113).
Keratoacanthoma
A keratoacanthoma is a rapidly growing tumour usually arising in the sun-exposed skin of the face or arms (Fig. 2). A keratoacanthoma is now generally considered a low-risk SCC, but was previously not regarded as malignant and may resolve spontaneously leaving a prominent scar. The tumour grows rapidly over a few weeks into a dome-shaped nodule up to 2 cm in diameter. There is often a keratin plug, which may fall out to leave a crater.
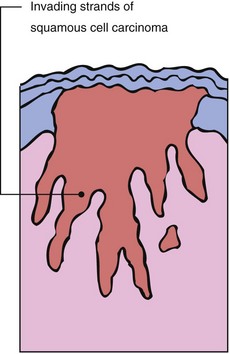
Squamous cell carcinoma
Clinical presentation
Squamous cell carcinomas usually develop in sun-exposed sites such as the face, neck, forearm or hand (Fig. 3). Commonly other signs of photodamage will be evident in adjacent skin: solar elastosis, hyperkeratosis, mottled pigmentation and telangiectasia. Premalignant changes such as actinic keratoses and Bowen’s disease as well as other skin cancers may also be present. On mucous membranes, leukokeratosis and fissuring or actinic chelosis are frequent. Lesions present in a variety of ways:
 A hyperkeratotic papule, plaque or cutaneous horn with an indurated base.
A hyperkeratotic papule, plaque or cutaneous horn with an indurated base.
 A small ulcer that refuses to heal.
A small ulcer that refuses to heal.

Fig. 4 Squamous cell carcinoma.
The cancer is seen here on the upper pinna in a patient with actinically damaged skin.
The tumour may start within an actinic keratosis as a small papule that, if left, progresses to ulcerate and form a crust. This type of SCC does not commonly metastasize. Ulcerating forms of SCC which develop at the edge of ulcers (Fig. 5), in scars and at sites of radiation damage are frequently more aggressive. Metastasis is found in 10% or more of these cancers. An important clinical marker of SCC is its rapidity of growth. Most patients will report a lesion that grows over several months, in contrast to a BCC which would frequently develop slowly over 6 or more months. Tenderness is also an important symptom identified in SCCs and is thought to represent the extension of the SCC around nerves.
Management
Squamous cell carcinoma
 Bowen’s disease is in situ squamous carcinoma and follows a less aggressive course. Treatment is with cryotherapy, topical, surgical or photodynamic therapy.
Bowen’s disease is in situ squamous carcinoma and follows a less aggressive course. Treatment is with cryotherapy, topical, surgical or photodynamic therapy.
 Keratoacanthoma is a spontaneously resolving lesion that bears clinical and histological resemblance to SCC. Excision is recommended.
Keratoacanthoma is a spontaneously resolving lesion that bears clinical and histological resemblance to SCC. Excision is recommended.
 Squamous cell carcinoma is often seen in the sun-exposed skin of white people in association with signs of actinic damage. A more aggressive form of the tumour is found with chronic scarring. All types are treated by surgical excision.
Squamous cell carcinoma is often seen in the sun-exposed skin of white people in association with signs of actinic damage. A more aggressive form of the tumour is found with chronic scarring. All types are treated by surgical excision.
 Squamous cell carcinomas with a worse prognosis (high risk) include:
Squamous cell carcinomas with a worse prognosis (high risk) include: