79. Sjögren Syndrome
Definition
Sjögren syndrome is a complex disorder in which exocrine organs are infiltrated by lymphocytes. It is characterized by sicca symptoms and is frequently associated with systemic lupus erythematosus, rheumatoid arthritis, or scleroderma.
Incidence
The estimated incidence of Sjögren syndrome is 0.1% to 3%, with the wide estimated range being the result of absence of uniform diagnostic criteria. Females are affected more often than males by a 9:1 ratio.
Etiology
The etiology of Sjögren syndrome is not truly known. Theoretically there appear to be interactions between major histocompatibility complex (MHC) genetic factors and non-MHC genetic factors, along with still-undelineated environmental factors. Sex hormones are theorized to play a role because of the overwhelming tendency of this disease to affect women.
Signs and Symptoms
Sicca symptoms
• Parotid enlargement
• Xerophthalmia
• Xerostomia
• Xerotrachea
Other
• Anemia
• Arthralgia
• Arthritis
• Dementia
• Fatigue
• Gastrointestinal disease
• Interstitial lung disease
• Leukopenia
• Lymphadenopathy
• Lymphoma
• Myalgia
• Neuropathy
• Palpable purpura
• Pneumonitis
• Pulmonary disease
• Raynaud phenomenon
• Recurrent bronchitis
• Renal tubular acidosis
• Seizures
• Vasculitis
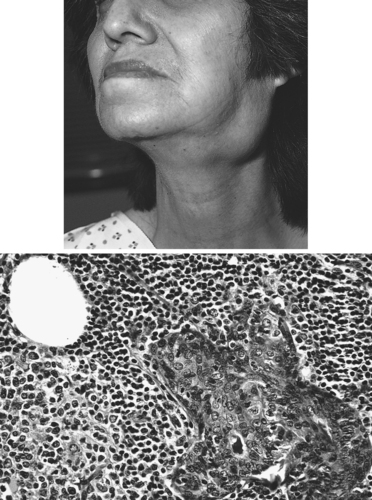 |
| Sjögren Syndrome. Enlargement of the salivary gland. |
Medical Management
Treatment interventions for the patient with Sjögren syn-drome are dictated by the symptoms the patient experiences. Sicca symptoms are treated by moisturizing interventions (e.g., xerophthalmia is treated with artificial tears; xerostomia is treated with liberal sips of water or sugar-free lemon drops to stimulate saliva production). More detailed interventions may be required that are dictated by the presence of an associated rheumatic disease such as systemic lupus erythematosus (see p. 335), rheumatoid arthritis, or scleroderma (see p. 305).
Complications
• Antiphospholipid syndrome
• Emergence of pseudolymphomas
• Emergence of systemic lupus erythematosus, rheumatoid arthritis, or scleroderma
• Parotid gland infection
• Parotid gland tumor
Anesthesia Implications
The anesthetist should continue interventions aimed at alleviation of sicca symptoms. The patient is particularly prone to corneal injury. Instilling eye lubricant and taping the eyelids closed during anesthesia are imperative for the patient with Sjögren syndrome. It is appropriate for the anesthetist to swab the patient’s mouth with some type of moisturizer perioperatively. To combat the patient’s xerotrachea, the anesthetist should use warmed, humidified gases throughout the duration of the anesthetic, whether general anesthesia, regional anesthesia, or monitored anesthesia care.
The anesthetist should anticipate that the patient with Sjögren syndrome may present with a difficult airway. Mask fit may be difficult to obtain because of enlargement of submandibular and/or parotid glands. Enlargement of these glands may hinder the anesthetist’s ability to visualize the patient’s vocal cords to intubate the patient. For more specific information regarding anesthesia implications, refer to the discussions of rheumatoid arthritis, systemic lupus erythematosus (p. 335), and scleroderma (p. 305).







