Chapter 13 Sinus and Escape Rhythms
Please go to expertconsult.com for supplemental chapter material.
Sinus Rhythms
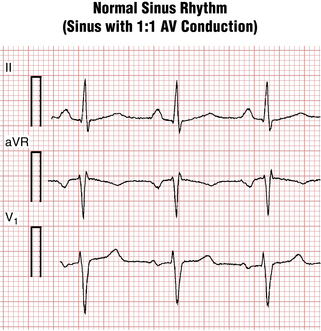
“Normal” Sinus Rhythm
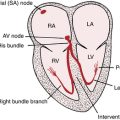
Sinus rhythm is the primary physiologic mechanism of the heartbeat. You diagnose it by finding P waves with a predictable polarity (see Chapter 4). When the sinus (also called the sinoatrial or SA) node is pacing the heart, atrial depolarization spreads from right to left and downward toward the AV junction. An arrow representing this depolarization wave points downward and toward the (patient’s) left. Therefore, with normal sinus rhythm, the P wave is always positive in lead II and negative in lead aVR (see Figs. 4-3 and 13-1).
Key Point
Recall the following from Chapter 4:
 If you state that the rhythm is “normal sinus” and do not mention any AV node conduction abnormalities, listeners will assume that each P wave is followed by a QRS complex and vice versa. The more technical and physiologically unambiguous way of stating this finding is to say: “Sinus rhythm with 1:1 AV conduction.”
If you state that the rhythm is “normal sinus” and do not mention any AV node conduction abnormalities, listeners will assume that each P wave is followed by a QRS complex and vice versa. The more technical and physiologically unambiguous way of stating this finding is to say: “Sinus rhythm with 1:1 AV conduction.”
 However, do not forget that sinus rhythm (i.e., the sinus node is the dominant or sole pacemaker of the atria) can exist not only with normal (1:1) AV conduction but with any degree of AV heart block (including complete or third degree) or even with ventricular tachycardia or asystole.
However, do not forget that sinus rhythm (i.e., the sinus node is the dominant or sole pacemaker of the atria) can exist not only with normal (1:1) AV conduction but with any degree of AV heart block (including complete or third degree) or even with ventricular tachycardia or asystole.
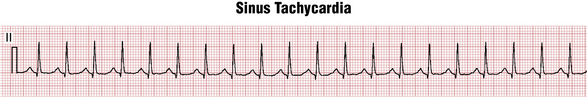
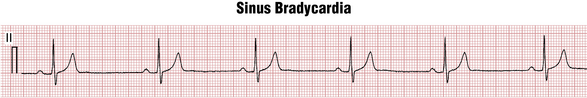
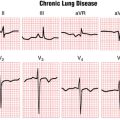
By convention, normal sinus rhythm in a resting subject is usually defined as sinus rhythm with a heart rate between 60 and 100 beats/min. Sinus rhythm with a heart rate greater than 100 beats/min is termed sinus tachycardia (Fig. 13-2). Sinus rhythm with a heart rate of less than 60 beats/min is called sinus bradycardia (Fig. 13-3). Some authors define sinus bradycardia based on a heart rate of less than 50 beats/min.
Regulation of the Heart Rate
The heart, like other organs, has a special nerve supply from the autonomic nervous system, which controls involuntary muscle action. The autonomic nerve supply to the heart (in particular, the SA and AV nodes) consists of fibers with opposing effects: the sympathetic nerves and the parasympathetic nerves. Sympathetic stimulation increases the heart rate and the strength of myocardial contraction. Sympathetic stimulation also occurs by secretion of circulating hormones called catecholamines (especially, norepinephrine and epinephrine), produced by the adrenal glands.
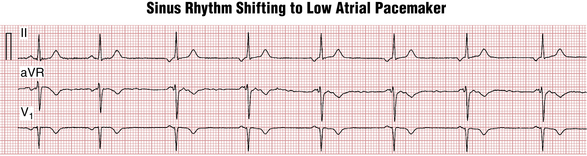
Parasympathetic stimulation (from the vagus nerve) produces slowing of the sinus rate as well as increased conduction time through the AV nodal area. It can also cause a pacemaker “shift” from the SA node to the low right atrial area producing so-called low atrial rhythm with negative P waves in leads II, III, and aVF (Fig. 13-4).
Sinus Tachycardia
Aging decreases the capacity to generate very rapid sinus rates. Elderly individuals (especially those older than 70 years) rarely show sinus tachycardia at rates above 140 to 150 beats/min even during maximal exertion. Indeed, heart rates above this range in the elderly, especially at rest, usually indicate the presence of a nonsinus tachycardia (e.g., atrial fibrillation or flutter, or a paroxysmal supraventricular tachycardia).
Figure 13-2 shows an example of sinus tachycardia. Each sinus P wave is followed by a QRS complex, indicating sinus rhythm with 1:1 AV conduction. Sinus tachycardia (or bradycardia), however, can occur with any degree of AV block. Notice that the P waves are positive in lead II. With sinus tachycardia at very fast rates, the P wave may merge with the preceding T wave and become difficult to distinguish.
In general, sinus tachycardia occurs with any condition that produces an increase in sympathetic tone or a decrease in vagal tone (Box 13-1). Sinus tachycardia may occur with healthy or pathologic states, usually involving increased cardiac output needs or decreased vascular resistance. Recall that systemic cardiac output per minute is the product of stroke volume (how much blood the left ventricle pumps with each beat) multiplied by the heart rate (beats/min).
BOX 13-1 Sinus Tachycardia: Some Major Causes
• Physiologic: excitement; exertion; pregnancy
• Fever, many infections, and septic shock
• Intravascular volume loss due to bleeding, vomiting, diarrhea, acute pancreatitis, or dehydration. Unexplained increases in heart rate may be an early sign of internal bleeding or other volume loss.
• Chronic heart failure (CHF). An increased resting heart rate in a patient with CHF may be the first sign of decompensation and is an adverse prognostic indicator.
• Pulmonary embolism: As noted in Chapter 11, sinus tachycardia is the most common “arrhythmia” seen with acute pulmonary embolism.
• Acute myocardial infarction (MI), which may produce virtually any arrhythmia. Sinus tachycardia persisting after an acute MI is generally a bad prognostic sign and implies extensive heart muscle damage.
Treatment of sinus tachycardia associated with a pathologic condition must be directed at the underlying cause (e.g., infection, sepsis, internal bleeding, pulmonary embolism hyperthyroidism, chronic heart failure [CHF], or alcohol withdrawal). Sometimes, more than one cause is present. In other cases, the cause may not be apparent. For example, inappropriate sinus tachycardia is a rare syndrome of unknown etiology, typically found in young females. The heart rate is more than 100 beats/min at rest without the expected decrease during sleep and with very rapid acceleration to 140 to 150 beats/min with minimal exercise. It is often combined with orthostatic hypotension.
Sinus Bradycardia
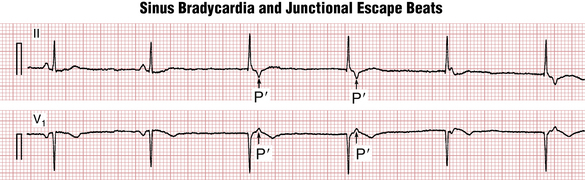
With sinus bradycardia, sinus rhythm is present and the heart rate is less than 60 beats/min (see Fig. 13-3). This arrhythmia commonly occurs in the conditions listed in Box 13-2.
BOX 13-2 Sinus Bradycardia: Some Major Causes
• Physiologic variants: Many, healthy people have a resting pulse rate of less than 60 beats/min, and trained athletes may have a resting or sleeping pulse rate as low as 35 beats/min. Sinus bradycardia is routinely observed during sleep. Obstructive sleep apnea may be associated with more profound sinus bradycardia.
• Acute myocardial infarction (MI). Sinus bradycardia with acute MI may be due to ischemia of the sinoatrial (SA) node itself which is perfused from a branch of the right coronary or the left circumflex artery in most people. Also, inferoposterior infarcts may be associated with enhanced vagal tone, sometimes inducing profound sinus bradycardia.
• Sick sinus syndrome and related causes of sinus node dysfunction: age-related degeneration of SA node; inflammatory processes; cardiac surgical and postsurgical causes
Moderate sinus bradycardia usually produces no symptoms. If the heart rate is very slow (especially, less than 30 to 40 beats/min in the elderly) lightheadedness and even syncope may occur. Treatment may require adjusting medication doses (e.g., beta blockers, calcium channel blockers; lithium carbonate; donezepil). If inappropriate sinus bradycardia causes symptoms of fatigue, lightheadedness, or syncope (as in the symptomatic sick sinus syndrome), or, if severe, symptomatic sinus bradycardia is due to an essential medication, an electronic pacemaker is usually indicated (see Chapter 21).
When evaluating a patient with sinus bradycardia at rest it is also useful to assess the heart rate response to exercise. Some people are unable to appropriately increase the heart rate during exercise, which can cause symptoms of fatigue and shortness of breath. This condition, when not due to a drug or other reversible factor, is called chronotropic incompetence; an electronic pacemaker might be indicated even when the resting heart rate is within the “normal” range (see Chapter 21).
Sinus Arrhythmia
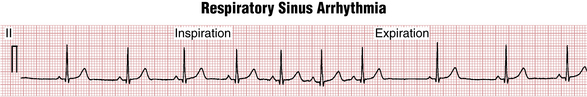
In healthy people, especially younger subjects, the SA node does not pace the heart at a perfectly regular rate. Instead, a slight beat-to-beat variation is present (Fig. 13-5). When this variability is more accentuated, the term sinus arrhythmia is used.
Sinus Pauses, Sinus Arrest, and Sinoatrial Block
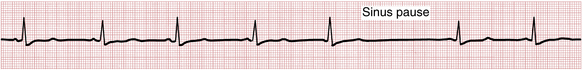
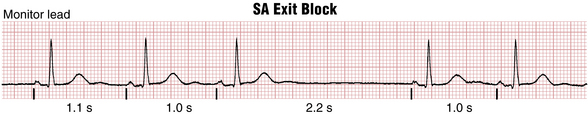
In addition to sustained sinus bradycardia, sinus node dysfunction may occur intermittently, ranging from a delayed beat (sinus pause; see Fig. 13-4) to long periods of asystole (sinus arrest). Two distinct mechanisms of sinus node dysfunction may be responsible for either sinus pauses or frank sinus arrest: sinus pacemaker failure and SA exit block The former is due to an actual failure of the SA node to fire for one or more beats. The latter happens when the SA impulse is blocked from exiting the node and stimulating the atria (Fig. 13-6). SA exit block may produce a pause that equals two or more PP intervals. From the ECG and clinical standpoint there is no significant difference between sinus node exit block or pacemaker failure. Always look for reversible causes of SA node dysfunction: drugs, hyperkalemia, etc. (see Box 13-2).
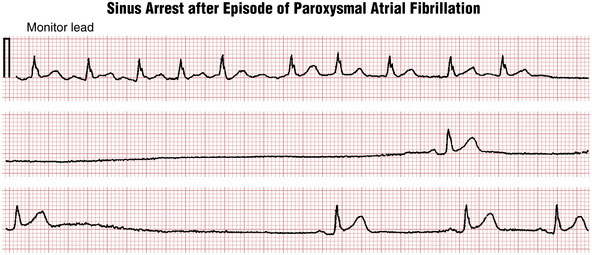
Sinus node dysfunction can happen spontaneously (sinus exit block; Fig. 13-7) or be induced by overdrive suppression of the sinus node by atrial fibrillation or flutter resulting in a prolonged postconversion pause when the arrhythmia abruptly terminates or “breaks” (Fig. 13-8). Such pauses are among the most common cause of syncope in patients with paroxysmal atrial arrhythmias (and are often exacerbated by rate-controlling medications such as beta blockers or calcium channel blockers) resulting in a type of brady-tachy syndrome requiring a pacemaker (see Chapter 21).
Secondary Pacemakers and Escape Rhythms
Why isn’t a sinus pause or sinus arrest leading to syncope and sudden cardiac arrest even more prevalent? Recall that sinus node cells undergo spontaneous rhythmic depolarization (firing), making the SA node the primary physiologic pacemaker of the heart. However, almost any heart cell (e.g., atrial and ventricular myocytes, AV node cells, Purkinje fibers) is capable of generating spontaneous depolarizations and, therefore, initiating or maintaining the heartbeat.
Atrial escape rhythms are characterized by regular P waves, slower than underlying sinus rhythm, with nonsinus P wave morphology (so-called “low atrial rhythm;” see Fig 13-4).
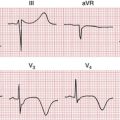
In junctional escape rhythm (terms AV junctional, junctional, AV nodal, and nodal are essentially synonymous), the atria are activated in a retrograde fashion, from bottom to top, producing negative P waves in leads II, III, and AVF, and a positive P wave in lead aVR (see Fig. 4-5).
With an AV junctional escape, the QRS complex will be normal (of “narrow” duration) because the ventricles are depolarized normally (unless a bundle branch block is also present). Furthermore, because the atria and ventricles are activated simultaneously during an AV junctional rhythm (not sequentially as with sinus rhythm), the QRS and P waves will occur at nearly the same time. As the result, an inverted P wave in lead II may appear: 1) just before QRS complex (with a very short PR interval), 2) inside the QRS (where the P wave is invisible), or 3) just after the QRS (producing “pseudo-S waves” in leads II, III, and aVF and “pseudo-R′” waves in leads V1 and aVR (Fig. 13-9).
Escape rhythms may also originate below the AV junction. Fascicular and idioventricular escape rhythms (Fig. 13-10) are slow wide QRS rhythms that usually indicate a life-threatening situation. They are associated with low blood pressure, are unstable, and can transition abruptly into pulseless electrical activity or asystole with cardiac arrest (see Chapter 19). Emergency treatment of underlying reversible conditions (such as hyperkalemia, digitalis toxicity, or other drug toxicity) is essential and temporary pacing is usually indicated.

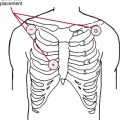
Figure 13-10 Idioventricular escape rhythm recorded during a cardiac arrest during attempted rescuscitation. The waveforms marked “X” are chest compression artifacts. The underlying atrial mechanism, if any, cannot be determined. (See also Chapter 19, “Basic ECG Patterns in Cardiac Arrest.”) Note also that the current recommended rate of chest compressions in adults is 100/min.