53 Simulation in Pediatric Anesthesia
THE FIELD OF PEDIATRIC anesthesia has become increasingly subspecialized, with unique challenges that demand high-quality teaching and training. Pediatric anesthesia is a subspecialty that has become increasingly refined and technically advanced, with the advancement of complex surgical techniques and patients with a low tolerance for error.1 Radiologic progress and interventions have revolutionized the field to include caring for children in remote sites outside of the operating theaters. In many countries, tertiary pediatric services are becoming increasingly centralized, whereas medical working hours have been reduced, leading to a situation where there is a decline in exposure to difficult pediatric cases and emergencies for those who are not pediatric specialists. There is an inverse correlation between the level of specialization and perioperative morbidity and mortality associated with pediatric anesthesia.2 Furthermore, a significant proportion of pediatric surgical procedures will continue to be performed outside tertiary centers, at community hospitals or outpatient surgical centers where the volume-to-outcome relationship may not be favorable.3 The growth and increased sophistication of pediatric anesthesia, as well as the regionalization of specialty care, has profound implications for the ability to train anesthesiologists in the safe and effective delivery of routine and emergency pediatric anesthesia. Early portions of a trainee’s learning curve are inconsistent with the demands of safe and efficient patient care, thereby posing challenges for the medical education infrastructure. Advancements in simulation education techniques and technology have led to a new paradigm in training and assessment. These advances provide opportunities to improve diagnostic and decision-making skills for common as well as rare events.
Current medical training emphasizes basic science knowledge and leaves most of the clinical practice to an apprenticeship model. The focus has been on individual knowledge and skills rather than on performance or clinical team dynamics. Once a clinician has completed training, the required level of continued education declines, both in structure and formality. Within the past decade, there has been rapid progress in simulation in health care training for purposes of improving patient safety and quality of care. Interest in simulation in health care derived from the historical utility of simulation for training purposes in nonmedical industries, such as commercial aviation, nuclear power production, and the military.4 Similar to health care, these industries are known to be associated with hazards and complexities that benefit from simulation training. Many of the concepts in health care simulators, including systematic training, rehearsal, performance assessment, situational awareness, and team interactions, have been adopted from aviation flight simulators. Given that crises in pediatric anesthesia are rare, difficult to predict, and that trainees are expected to be able to successfully manage these situations, simulation technology can fill important gaps in many curricula. In this chapter, we review how simulation is applied in pediatric anesthesiology by describing its use for learning and practicing basic and advanced skills, and by defining key types of technologies and teaching approaches with illustrative videos.
Simulation-Based Training in Anesthesia
In 1987, Gaba and colleagues identified gaps in decision making and crisis management in anesthesia training. They noted that diagnostic decisions tended to be relatively static.5–7 However, in the complex, rapidly changing, time-pressured environment of the operating room (OR), anesthesiologists are challenged beyond static decision making, especially when identifying and resolving crises and leading interdisciplinary teams. As a result, the term anesthesia crisis resource management (ACRM), modeled after the Crew Resource Management of commercial aviation,5–7 was developed. These investigators established a framework and curriculum to teach individual and team leadership skills, along with effective communication styles. ACRM provided anesthesia trainees with tools that were similar to those that made the complex dynamic world of aviation safer in the areas of decision making and crisis resource management. These skills were not systematically taught during anesthesia residency training.
ACRM was an outgrowth of the patient safety movement that began in anesthesia in the early 1980s in America. In the late 1980s, research grant funding from the Anesthesia Patient Safety Foundation (APSF) supported the early development of several forms of human patient simulators (HPS). Further publicity and advocacy from APSF propelled anesthesiology to the forefront of specialties in the application and adoption of simulators, with strong patient safety implications through education (residents attempting new skills for the first time on a manikin), training (teamwork, critical event management, and situational awareness), and research (human performance).8 Today, simulation in anesthesiology is global, with emphasis not only on medical knowledge and skills training, but also on ACRM, disaster training, debriefing, and patient safety. The American Board of Anesthesiology now requires at least one simulation-based course to satisfy its Maintenance of Certification in Anesthesia requirement.9 In some institutions, such training is required as a condition of credentialing for practice and insurance coverage.
What is Simulation?
Simulation is a technique to replace or amplify real experiences with guided experiences that evoke or replicate aspects of the real world. Simulation is enabled by a diverse set of emergent technologies.4 The application of simulation in the health care field is focused on education and training of clinicians. Education emphasizes knowledge, skills, and introduction to the actual work. Training emphasizes the actual tasks and work to be performed.4 The term “simulator” is used in the health care field to refer to a device that represents a simulated patient, and interacts appropriately in response to the actions of the simulation participant. In aviation, pilots are seated in the cockpit of a flight simulator whereas in health care, clinicians are in a simulated OR, emergency ward, or patient floor in simulated clinical scenarios, caring for a simulated “patient” experiencing a critical or otherwise challenging event.
Participants in a simulation are “immersed” into a task or setting to the extent necessary to achieve the learning objectives. This may be conducted in a normal classroom or in an environment that extensively replicates the real world. In the latter case, participants are asked to “suspend disbelief” and to interact and speak as they would do in their everyday jobs.4 Most importantly, it is incumbent on those who create and implement the simulation to create sufficient realism to enable the learner to feel the reality of the situation and respond accordingly. Thus the participant agrees to accept the “fiction contract” with their instructors.10,11
Participants in a simulation scenario experience realism in three distinct domains: physical, conceptual, and emotional.10 Simulations that address all three domains are more likely to instill the intended learning objectives. A high degree of realism appropriate for the specific learning objectives is central to ensure that the learners become mentally and physically engaged. The physical properties of the simulator (the patient) and the clinical environment (the simulation room, center, or OR), such as weight, flexibility, tensile strength, and color, are important for developing kinesthetic awareness and muscle memory. For example, the weight of the head and force required to effectively perform laryngoscopy are important for teaching tracheal intubation, whereas the rubbery feel of the manikin skin is not. Conceptual realism refers to the causal relationships observed in the scenario, such as a decrease in oxygen saturation during a period of apnea or the resolution of hypotension after an appropriate intravenous fluid bolus. High conceptual reality enhances clinical reasoning and decision making. Finally, emotional and experiential fidelity is achieved when participants experience familiar and authentic feelings, such as “emotional activation,” anxiety, stress, fear, or excitement. Ultimately, realism in simulation is perceived as “an exciting simulation that captures the imagination, triggering physiological responses and execution of ingrained clinical algorithms.”10 Although realism is important, investigators emphasize that, “when learning is the focus, the flawless recreation of the real world is less important.” It is necessary to find circumstances that help participants learn, rather than circumstances that exactly mimic a clinical situation.11 The degree of realism desired for a successful simulation education program is an amount sufficient to achieve the intended learning outcomes.
Technologies Used in Simulation
Partial Task Trainers
Partial task trainers are manikins or models (e.g., suturing board, IV arm, airway head, etc.) designed to allow participants to practice clinical skills and tasks (Fig. 53-1). They should be reliable, robust, and medically meaningful. Usually they represent a portion of a person rather than the whole. Although many are simple devices designed for learning or practicing a specific procedure (e.g., suturing, IV insertion, laryngoscopy, or intraosseous access), some are coupled with computers, robotic interphases, and digital graphics to provide sophisticated partial task simulators designed for learning or practicing more involved procedures (e.g., bronchoscopy and endoscopy, endovascular catheterization, or laparoscopic skills). These models are particularly useful for teaching invasive, risky, and rare procedures (e.g., emergency cricothyrotomy, transvenous pacing, or pericardiocentesis), complex psychomotor skills requiring repetitive training (e.g., ultrasound guided central venous catheterization or awake fiberoptic intubation), or those that are safe, but create increased anxiety for either the learner or the patient and their family (e.g., urethral catheterization, IV insertion, or arterial puncture), where coaching and deliberate practice can be done in a simulated environment.12 Curricula that use these types of training devices focus on skills training at varying levels of skill goals, rather than a particular situation. For example, cricothyrotomy training on a partial task simulator aims to teach the procedure, regardless of the indication (e.g., angioedema, burns, obstructing mass, or hemorrhage). Specific partial task trainers for simulating aspects of children include products to learn or practice lumbar puncture, peripheral IV insertion, intraosseous needle insertion, laryngoscopy and intubation, umbilical vein and artery catheterization, and cardiopulmonary resuscitation (Video 53-1)![]() .
.
Human Patient Simulators
An HPS is a representation of the human body constructed on a manikin, typically made of plastic and metal, without a bony skeletal frame. Although popularized in the 1990s, the first manikin-based simulator (SimOne) was developed at University of Southern California in the 1960s and was intended to facilitate medical education and training.13 Adult HPSs became commercially available in the early 1990s; the first high-fidelity pediatric simulator was introduced in 1999. The METI PediaSIM (Medical Education Technologies, Inc., Sarasota, Fla.) represented a child between 5 and 7 years of age. Two models of integrated infant HPS became available in 2005: the METI BabySIM and the Laerdal SimBaby (Laerdal Medical, Stavanger, Norway) (Fig. 53-2). Both models exhibited standard vital signs and variable airway features (e.g., tongue swelling and laryngospasm), breathing patterns and sounds (e.g., retractions to illustrate upper airway obstruction, breath sounds [wheezing], and pneumothorax), cardiovascular features (e.g., heart sounds and peripheral pulses [diminished or absent]), and others (e.g., abdominal sounds and distension, and fontanelle bulging). Both infant simulators produce a variety of monitor signals and allow extensive treatment interventions (e.g., intubation, laryngeal mask and nasogastric tube insertion, intravenous and intraosseous cannulation, and thoracocentesis).14 Incorporated into the clinical setting or in a simulation room outfitted with biomedical equipment and teams of health care providers, the HPS can provide a high degree of clinical authenticity and realism to facilitate participants to fully engage in the care of the simulated patient. Typically, participants in simulation scenarios reflect on their performance during the simulation, for the purpose of sustaining and improving their practice with an instructor, in the process termed debriefing15 (see Video 53-1).
Standardized Patient
In some facilities, actors who are trained to represent a patient’s condition (e.g., symptoms or social situation) and who are very reliable raters of clinicians’ behaviors are used as standardized patients. It is common practice to use standardized patients when a simulation session focuses on interviewing, counseling, and examining a patient. Now a required part of the medical licensing exam in the United States (USMLE Step II Clinical Skills), Objective Structured Clinical Exams (OSCEs) are common in many undergraduate and graduate medical education programs. The OSCEs have been incorporated into the national board certification exams for anesthesiology in Israel.16 In pediatrics, actors are more likely to play the role of a parent (e.g., a standardized parent) and team members (e.g., a standardized nurse), although child actors have also been reported, as well as the use of youthful appearing actors who role-play adolescents.17 Going beyond standardized patients, actors can be employed as standardized nurses, surgeons, even residents for the purpose of teaching supervision skills (see Video 53-1).
Screen-Based Simulator: Virtual Patients and Immersive Environments
Virtual patients are generally two-dimensional avatars on the computer screen that serve to help learners maneuver through clinical situations or perform a task, such as the proper technique for taking a patient’s medical history. They can also be incorporated into OSCE training when standardized patients are not available. For example, the American Heart Association uses a screen-based simulation to teach and assess knowledge from advanced cardiac life support and pediatric advanced life support courses.18
Immersive environments, such as Second Life (Linden Lab, San Francisco), Advanced Disaster Management Simulator (Environmental Tectonics Corp., Orlando) and multi-user virtual environments, have been used to teach disaster management using interactive virtual simulation systems.19–21 Other examples include Gas Man (Med Man Simulations, Inc., Boston) for teaching, simulating, and experimenting with the uptake and distribution of inhalational anesthetics,22 and a virtual reality simulator for training in regional anesthesia.23 Although virtual reality has been used in advanced cardiac life support and pediatric advanced life support education,18 the use of virtual reality simulators in anesthesia is novel and not yet widely incorporated into curricula (see Video 53-1).
Sites for Simulation
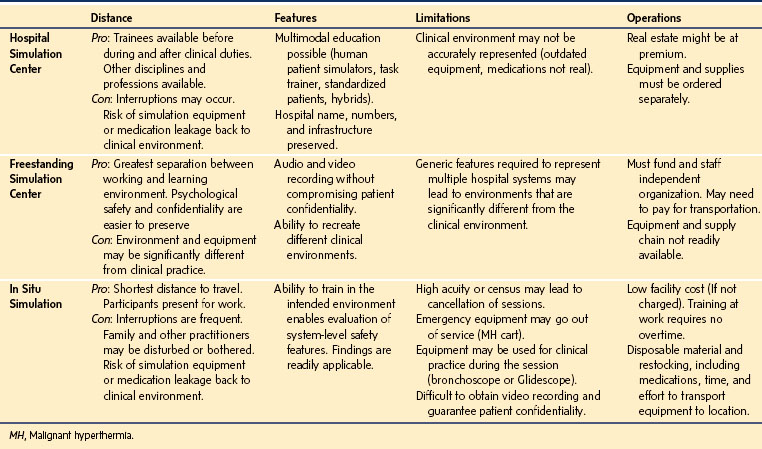
The growth of simulation education centers has been exponential from the mid-1990s through the first decade of this century. There is no exact count, but there are at least 1000 centers worldwide incorporated within medical schools and residency training programs in hospital settings, as well as nursing schools and allied health professions colleges.24 Different settings of simulation education centers include: hospital-based or medical school-based simulation centers, freestanding simulation facilities, and in situ simulation located within the actual clinical work environment (Fig. 53-3). Dedicated simulation facilities, either within an existing medical institution or a freestanding center, have been constructed throughout the industrialized world to house high-technology simulator equipment, such as manikins, laparoscopic surgical equipment, robotics, and audiovisual laboratories. For example, the Treadwell Library at Massachusetts General Hospital has a dedicated simulation learning lab that houses simulation equipment, high-fidelity manikins, partial task trainers, and simulators for students, residents, and faculty training. Although simulation education centers are expensive and require significant manpower to operate, they may serve to replace some traditional forms of clinical education for many of the reasons that simulation is generally becoming more accepted (e.g., patient safety, clinical production efficiency, and lack of standardized curricula in the apprenticeship mode). An in situ simulation location involves setting up the simulator equipment, trainers, and trainees within the actual work environment, such as the OR, emergency room, or intensive care unit. The benefits of an in situ simulation include imitation of the work environment with equipment, personnel and surroundings that are real and familiar to the trainee. Disadvantages of in situ simulation involve availability of the location, impromptu setup of equipment to operate in different locations, and increased manpower to help with set up and relocation (Table 53-1).
Applications of Simulation in Anesthesia
Concern for patient safety has been growing since the Institute of Medicine of the U.S. National Academies of Sciences published a report, To Err is Human, which publicized medical errors in patient care.25 Since then, numerous efforts and interventions have been implemented to mitigate medical hazards and improve patient safety.26 The demand for pediatric simulation curricula is substantial, presumably driven by the perceived imbalance between the potential difficulties of incidents and emergencies, and the everyday clinical routine, particularly for anesthetizing infants and neonates. Simulator-based courses can effectively supplement bedside teaching in pediatric anesthesia for trainees, non–tertiary-center anesthetists, and pediatric anesthesiologists alike. Newer infant simulators can generate a wide range of pediatric case scenarios and have the advantage of being mobile for in situ simulation in the OR, intensive care unit, or emergency department setting. Training and managing low-frequency, high-risk cases (e.g., malignant hyperthermia, difficult airway, venous air embolism, or neonatal resuscitation) can be effectively performed on these manikins.27 In addition, evaluation of new procedures and technology or simulation of new hospital environments can be safely performed on these manikins before involving humans. For example, the anesthesia residents at Massachusetts General Hospital are taught basic pediatric anesthesia skills and airway management during a simulation orientation at the beginning of their dedicated pediatric month. This in situ simulation curriculum occurs monthly in the Massachusetts General Hospital ORs for residents new to the rotation, before they care for children. A combination of partial task trainers, standardized “parents,” and high-fidelity HPS infant manikins are used to orient and teach residents about the typical flow of a pediatric anesthesia case.
Comparing Traditional Learning with Simulation-Based Learning
The medical learner at each level of higher education (i.e., undergraduate, graduate, or postgraduate) is an adult learner. An adult learner is one who learns by several methods for different reasons at various stages in his or her education.28 Adult learning theory teaches that active learning (with simulation) is an effective way to prepare for the dynamic clinical environment.29 Five adult learning principles to help guide medical learners have been described28–30 (Table 53-2).
TABLE 53-2 Five Adult Learning Principles That Apply to the Medical Learner
1. Adult learners need to know why they are learning
2. Adult learners are motivated by the need to solve problems
3. The previous experiences of adult learners must be respected and built upon
4. The educational approach should match the diversity and background of adult learners
5. Adult learners need to be involved actively in the process
Modified from Okuda Y, Bryson E, Demaria S. The utility of simulation in medical education: what is the evidence? Mt Sinai J Med 2009;76:330-43, and Bryan R, Kreuter M, Brownson R. Integrating adult learning principles into training for public health practice. Health Promot Pract 2009;10:557-63.
Aspects of a High-Fidelity Simulation
High-fidelity simulation requires considerable manpower and preparation. A typical team consists of the following: a team leader, actors, high-fidelity manikin, simulation room, audiovisual equipment, participants and learners, a facilitator, and a debriefer.31 The team leader may be compared with a director of a film production. He or she is responsible for the smooth execution of the case scenario, from assigning and delegating roles to team members and directing the evolving scenario in the console room, to handling unexpected problems and situations that may arise during the simulation. This position may be the same or different from an “operator” who is responsible for operating the manikin behind the scenes in the console room. Actors, otherwise known as “confederate actors,” are responsible for creating the realism of the case scenario by effectively performing impromptu in a case scenario. They may take roles, such as nurses, surgeons, technicians, or administrative staff, to help guide the participants in a way that is clinically familiar. The challenge for actors is to maintain their simulated character and to interact with participants to guide them, but without overt interference with the clinical decisions and management. Communication between confederate actors and control room personnel using wireless audio devices is helpful to maintain the smooth flow of the scenario.
The simulation room is ideally a flexible setting that can be converted into a range of patient care environments, such as the OR, emergency department, obstetric ward, a cafeteria or other public place—anywhere an anesthesia team might be called to respond. Elaborate scenery, anesthesia and surgical equipment used in everyday work, and moulage (e.g., fake blood and vomitus) may create very realistic scenarios. The rooms should be equipped with medical air, oxygen, and vacuum suction capabilities to run the high-fidelity manikins and to provide for their use in the scenario.31 Audiovisual equipment, such as cameras and microphones, are strategically placed so as to not be obvious to the participants, whose actions are followed in the simulation for debriefing and feedback. The facilitator is responsible for observing the simulation scenario, and after the event to stimulate learning and discussion in a nonthreatening and organized way. The facilitator’s role is to identify elements of the simulation that possess educational value pertinent to the learning objectives of the course, and to facilitate discussion of these learning nuggets (e.g., point out where communication broke down or where situational awareness was lost) (Video 53-2)![]() .
.
What is a Debriefing?
A debriefing is a “conversation between two or more people to review a real or simulated event in which participants analyze their actions and interactions, and reflect on the roles of thought processes, psychomotor skills, and emotional states, to improve or sustain performance in the future.”32 It is generally thought that the debriefing is the most important component of simulation-based education, the time when learning is embedded. Many consider the scenario an excuse for the opportunity for debriefing. Facilitated by the debriefer, the debriefing usually follows the simulation. “Pause and discuss” style debriefing, where the faculty interjects during pauses in a scenario has been shown to be an effective teaching method.33 Video review of portions of the scenario can be helpful during a debriefing, especially when used to observe key moments, clarify recall discrepancies among participants and faculty, and to offer a global view of the room to participants who might have been focused on a task or fixated on a portion of the action. This guided reflection of the scenario allows participants to bridge the gap between experiencing an event and making sense of it.
Debriefing can be approached in three phases: reactions, understanding, and summary.15,32,34 The reactions phase asks participants to share how they felt, allowing the participants to vent and deactivate from the heightened emotional state that participating in a simulation provokes. The debriefer leads the group through a description of the facts of the case, to ensure that everyone understands the clinical scenario before tackling the learning objectives. The understanding phase is the richest and longest phase, and is intended to help participants analyze and apply what happened and explore deeper meaning of the interactions. Discussion and teachings are involved in this phase to help simulation participants gain new perspectives and insights into group dynamics and communication. Lessons learned during the simulation can be generalized and applied to the real world, preparing participants to transfer new knowledge into their clinical practice. In the summary phase, participants share lessons learned, including individual and group behaviors, skills, and thinking patterns that they wish to improve, as well as those that were productive and they wish to retain for future performance.15,32,34 Becoming an effective debriefer requires training and practice to acquire new skills that are not taught in traditional health care educational programs. Instructors and facilitators are encouraged to learn about the principles of effective debriefing via the literature, formal courses, and mentoring. The Debriefing Assessment for Simulation in Healthcare (DASH) is an example of a testing instrument that was developed to assess and improve debriefing skills.35
Using Simulation for Evaluation
Although patient simulators are well accepted as a core component of crisis resource management and other clinical training, their acceptance and validity as assessment tools for clinical performance has not yet been widely established or validated. In particular, a number of senior professionals are reluctant to be assessed in a simulator environment (e.g., in the process of their recertification). However, some scoring systems for simulator-based performance assessments have been developed, such as the Anaesthetists’ Non-Technical Skills (ANTS) system.14,36 Although validity is not yet rigorous (e.g., based on correlation of training with consistent transfer of skills into clinical use or improvement of patient care), there is increasing evidence that simulation-based assessment can be done with sufficient reliability to be used for testing (e.g., reproducible scenarios can be created and implemented, raters can be trained to assign reproducible scores of performance, and critical clinical skills can be simulated).37 Multiscenario, simulation-based assessment has the potential to assess performance of pediatric anesthesia skills in anesthesia residents and pediatric anesthesia fellows; however, further measures of validity, including correlations with direct measures of clinical performance, are needed to establish the true utility and validity of these simulations as assessment tools.27
Simulation is widely thought to be effective in improving clinical skills in a way that is safer than the traditional apprentice model of training. Although there is not yet a large body of evidence regarding the effectiveness of simulation or the cost relative to its benefit, there is substantial literature that documents its utility. A meta-analysis has established the overall effectiveness of simulation-based training.38 Furthermore, a study of simulation-based training showed improved outcomes, specifically in survival of children after cardiopulmonary resuscitation.39
Challenges in Using Simulation
Although simulation centers are increasingly popular worldwide, there are many challenges in establishing and maintaining a simulation program. Trained educators in simulation are few and apprenticeship models require extensive time and effort. There are now several simulation programs that offer various types of courses for educators and instructors. Popular centers that consistently offer courses are the Center for Medical Simulation in Cambridge, Mass. (http://harvardmedsim.org/), the Multidisciplinary Simulation Center in Rochester, Minn. (http://www.mayo.edu/simulationcenter/), the Center for Immersive and Simulation-Based Learning in Palo Alto, Calif. (http://cisl.stanford.edu/), the Michael S. Gordon Center for Research in Medical Education in Miami (http://www.gcrme.miami.edu/), the Danish Institute for Medical Simulation in Herlev, Denmark (http://www.regionh.dk/dims-eng/menu/), and the Tübingen Center for Patient Safety and Simulation in Tübingen, Germany (http://www.tupass.de/). Fellowships in medical simulation are also becoming more widespread across the U.S., located within anesthesia, emergency medicine, and other departments, or at interdisciplinary centers, such as the Neil and Elise Wallace STRATUS Center for Medical Simulation in Boston (http://www.stratus.partners.org). However, availability of faculty members to develop curricula and routinely run simulation case scenarios has been a challenge due to operational costs and the high demands of clinical practice and patient care. Technical staff and support to help run a simulation center are also important factors that affect the overall cost of operating a center. Simulation equipment, computers, partial task trainers, and high-fidelity manikins are expensive, as is the maintenance of this equipment. In some institutions, funding may not be available to staff and operate a simulation center with a skills training laboratory. Other options may include implementing in situ simulations in existing hospital facilities, remodeling old facilities into a simulation room, or having mobile units that contain simulation equipment. Hence, operating and maintaining a simulation center poses monetary, time availability, and faculty availability concerns.
Future of Simulation
Simulation-based education provides many opportunities for curriculum development in anesthesia residency training, with creative strategies to enhance clinical experiences, to practice caring for rare cases, and to improve mass-casualty training. This model will become of greater importance as residency work-hours are reduced. Although the apprenticeship model and patient care experience is unlikely to be replaced, incorporation of simulation-based training can help provide solutions to systems-based problems, improve interdisciplinary team training, ease relocation into facilities, and help adapt to new equipment and technology. Since 2004, the Society for Simulation in Healthcare has represented a growing community of educators and researchers who use simulation techniques for education, testing, and research in health care. This consistently growing international society (over 3000 members in 2012) is a broad-based, multidisciplinary, multispecialty network that ties together physicians, nurses, and allied-health professionals with educators and other social scientists, as well as with industry.40 Other societies, including the Society for Simulation in Healthcare in America and the Society in Europe for Simulation Applied to Medicine, provide technical and political leadership for the simulation community.
The extent of the long-term impact of simulation on health care still remains to be determined; however, what is certain is that a large part of residency training and maintenance of skills will incorporate simulation-based education. The American Board of Anesthesiology now requires simulation-based crisis resource management training as part of its program for recertification. Other specialty medical boards are also considering using simulation as a requirement for certification and recertification. In Israel and the United Kingdom, simulation-based stations are included in the National Anesthesia Board exams and OSCEs in anesthesia, respectively.16,41 Simulation-based education and research will become an integral part of health care. Future research must nonetheless focus on addressing questions of how best to use simulation to improve real-life quality of care, patient safety, and long-term care.
1 Blike GT, Christoffersen K, Cravero JP, Andeweg SK, Jensen J. A method of measuring system safety and latent errors associated with pediatric procedural sedation. Anaesth Analg. 2005;101:48–58.
2 Murat I, Constant I, Maud’huy H. Perioperative anaesthetic morbidity in children: a database of 24,165 anaesthetics over a 30-month period. Pediatr Anaesth. 2004;14:158–166.
3 Jenkins JK, Newburger JW, Lock JE, et al. In-hospital mortality for surgical repair of congenital heart defects: preliminary observations of variation by hospital caseload. Pediatrics. 1995;95:323–330.
4 Gaba D. The future vision of simulation in health care. Qual Saf Health Care. 2004;13:i2–10.
5 Gaba D, Howard S, Fish K, Smith B, Sowb Y. Simulation-based training in anesthesia crisis resource management (ACRM): A decade of experience. Simul Gaming. 2001;32:175–193.
6 Gaba DM, DeAnda A. A comprehensive anesthesia simulation environment: re-creating the operating room for research and training. Anesthesiology. 1988;69:387–394.
7 Gaba D, Fish K, Howard S. Crisis management in anesthesiology. Philadelphia: Churchill Livingstone; 1994.
8 Anesthesia Patient Safety Foundation (APSF). APSF website. Available at http://www.apsf.org/about_history.php
9 The American Board of Anesthesiology. Maintenance of certification in anesthesiology website http://www.theaba.org/Home/anesthesiology_maintenance
10 Rudolph JW, Simon R, Raemer DB. Which reality matters? Questions on the path to high engagement in healthcare simulation. Simul Healthc. 2007;2:161–163.
11 Dieckmann P, Gaba D, Rall M. Deepening the theoretical foundations of patient simulation as social practice. Simul Healthc. 2007;2:183–193.
12 Ericsson KA. Deliberate practice and acquisition of expert performance: a general overview. Acad Emerg Med. 2008;15:988–994.
13 Rall M, Gaba DM. Patient simulators. In: Miller RD, ed. Miller’s anesthesia. 6th ed. Philadelphia: Elsevier; 2005:30–78.
14 Eich C, McFadzean J, Schwarz Sl. Simulator-based training in paediatric anaesthesia and emergency medicine–thrills, skills and attitudes. Br J Anaesth. 2007;98:417–419.
15 Rudolph JW, Simon R, Dufresne RL, Raemer D. There’s no such thing as “non-judgmental” debriefing: a theory and method for debriefing with good judgment. Simul Healthc. 2006;1:49–55.
16 Berkenstadt H, Ziv A, Gafni N, Sidi A. Incorporating simulation-based objective structured clinical examination into the Israeli National Board Examination in Anesthesiology. Anesth Analg. 2006;102:853–858.
17 Tsai TC. Using children as standardised patients for assessing clinical competence in paediatrics. Arch Dis Child. 2004;89(12):1117–1120.
18 Advanced Cardiac Life Support (ACLS) Training Center. ACLS, PALS & BLS online. Available at http://www.acls.net
19 Wikimedia Foundation, Second Life. Available at http://en.wikipedia.org/wiki/Second_Life
20 Environmental Tectonics Corp. Advanced Disaster Management Simulator website http://trainingfordisastermanagement.com
21 Wikimedia Foundation, MUVE. Available at http://en.wikipedia.org/wiki/MUVE
22 Med Man Simulations, Inc. Gas Man website. Available at http://www.gasmanweb.com
23 Grottke O, Ntoub A, Ullrich S, et al. Virtual reality-based simulator for training in regional anaesthesia. Br J Anaesth. 2009;103:594–600.
24 Okuda Y, Bond W, Bonfante G, et al. National growth in simulation training within emergency medicine residency programs, 2003-2008. Academic emergency medicine: official journal of the Society for. Acad Emerg Med. 2008;15:1113–1116.
25 To err is human: building a safer health system. Kohn, KT, Corrigan, JM, Donaldson, MS, National Academy Press, Washington D.C., 1999.
26 Rodriquez-Paz J, Mark L, Herzer K, et al. A novel process for introducing a new intraoperative program: a multidisciplinary paradigm for mitigating hazards and improving safety. Anesth Analg. 2009;108:202–210.
27 Ferh J, Boulet J, Waldrop W, et al. Simulation-based assessment of pediatric anesthesia skills. Anesthesiology. 2011;115:1308–1315.
28 Okuda Y, Bryson E, Demaria S. The utility of simulation in medical education: what is the evidence? Mt Sinai J Med. 2009;76:330–343.
29 Knowles MS, Holton EF, III., Swanson RA. The adult learner. The definitive classic in adult education and human resource development, 6th ed. Burlington, Mass.: Elsevier; 2005.
30 Bryan R, Kreuter M, Brownson R. Integrating adult learning principles into training for public health practice. Health Promot Pract. 2009;10:557–563.
31 Seropian M. General concepts in full scale simulation: getting started. Anesth Analg. 2003;97:1695–1705.
32 Center for Medical Simulation. Center for Medical Simulation website. Available at http://www.harvardmedsim.org
33 Hogan J, Flanagan B, Marshall S. What facilitation skills are required to assist students’ learning when using a patient simulator in the “pause and discuss” mode? Focus on Health Professional Education: A Multidisciplinary Journal. 2008;10:36–37.
34 Rudolph JW, Simon R, Raemer DB, Eppich W. Debriefing as formative assessment: closing performance gaps in medical education. Acad Emerg Med. 2008;15:1010–1016.
35 Debriefing Assessment for Simulation in Healthcare (DASH), http://www.harvardmedsim.org/debriefing-assesment-simulation-healthcare.php.
36 Boet S, Bould D, Bruppacher H, et al. Looking in the mirror: self-debriefing versus instructor debriefing for simulated crises. Crit Care Med. 2011;39:1377–1381.
37 Murray D, Boulet J, Kras J, McAllister J, Cox T. A simulation-based acute skills performance assessment for anesthesia training. Anesth Analg. 2005;101:1127–1134.
38 Cook DA, Hatala R, Brydges R, et al. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. JAMA. 2011;306:978–988.
39 Andreatta P, Saxton E, Thompson M, Annich G. Simulation-based mock codes significantly correlate with improved pediatric patient cardiopulmonary arrest survival rates. Pediatr Crit Care Med. 2011;12:33–38.
40 Society for Simulation in Healthcare (SSH). SSH website. Available at http://ssih.org
41 Glavin R, Gaba D. Challenges and opportunities in simulation and assessment. Simul Healthc. 2008;3:69–71.