Chapter contents
6.1 Introduction 72
6.2 The simple pulse parameters 73
6.3 Rate 73
6.4 CM pulses defined by rate 78
6.5 Rhythm 83
6.6 CM pulses defined by rhythm 88
6.7 Depth 91
6.8 CM pulse qualities defined by level of depth 94
6.9 Length (longitude) 100
6.10 CM pulse defined by length 101
6.11 Width (latitude) 103
6.12 CM pulse qualities defined by arterial width 110
6.13 Summary 112
Pulse diagnosis is often complicated in the clinical context because pulse manifestations as they present in the radial artery do not present as nice discrete ‘images’ as posited in the literature. Indeed, expectations of always feeling a classical pulse quality are misplaced and will lead to difficulties and frustration on the part of the pulse taker. Rather, it should be expected that the pulse may ordinarily present as no recognisable traditional pulse quality. This is to be expected, as each person will not always respond the same way to the same illness: a person’s constitution and the relative strength of their Qi and blood means the body responds differently. Other factors such as lifestyle (work, exercise, dietary) and life history only add further variability.
There may be instances when the pulse taker assesses the pulse when the immune system is just responding to a pathogenic agent so the pulse is felt while it is moving from the individual’s normal or healthy pulse to the pulse that reflects the nature of the pathogenic illness and the body’s response to that illness. In this situation, the pulse is not yet fully formed and may also not fit nicely into the distinctive CM pulse qualities described in the literature. Alternatively, the body’s response to the illness is such that the pulse quickly forms a recognisable quality and it is over time as the body’s energies are depleted or the pathogen mutates that the pulse quality may assume a less recognisable form.
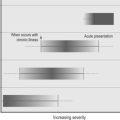
In this sense, the pulse can be thought of in terms of a continuum (Fig. 6.1). The idea of the pulse as a continuum is purposely used to denote that the pulse is not a static sign, nor is the body a static organism. In this sense, there are no ‘absolutes’ as to how the pulse should be, it always just is . It is reflective of the relative degree of the body’s ability to maintain normal healthy function or homeostasis in response to the constant demands of living. In terms of illness or dysfunction, the idea of the continuum refers to the changing flux of the pulse between two points of reference. At one reference point are those pulses reflecting health, usually assumed to be the individual’s usual pulse state; at the other point of reference are those pulses that reflect illness or dysfunction — the potential end manifestation of the pulse flux if no treatment intervention is provided to counter the pathogen/dysfunction.
 |
| Figure 6.1Schematic of the pulse in a continuum. The pulse formation illustrated has aspects of the Firm pulse, Slippery pulse and Floating pulse and so does not discretely fit into any of these pulse categories as they are defined within the literature. |
Sometimes the pulse palpated is in flux on a continuum between two pulse types that both reflect illness or dysfunction; there may be a worsening or improvement in an illness, but not necessarily resolution of the illness. Chronic inflammatory conditions such as arthritis are examples of diseases in which there are acute periods of inflammation interspaced with periods of generalised symptoms. In this respect, certain pulse qualities develop slowly, progressing through stages in response to physiologic changes associated with disease progression or resolution. Such a process is comparable to that described by Katz (2000) in relation to the problems of defining heart failure.
… this condition is not a disease but instead represents the final common pathway by which a number of disorders damage the heart so as to cause disability and premature death. These disorders include coronary disease, hypertension, valvular disorders, and a diverse group of heart muscle diseases referred to as cardiomyopathies. Furthermore, because this syndrome establishes a number of vicious cycles, heart failure begets more heart failure. (p. 7)
The description is particularly pertinent to pulse diagnosis. In this respect, pulses reflecting chronic illness and dysfunction arising from the consumption of vital substances occur over time. Some of the traditional pulse qualities are reflective of this chronological progression of illness and will only occur as an end result of a long disease process. Other pulses occur only in an acute situation. Some other pulse qualities occur only when fundamental substances of Qi, Blood and Fluids are abundant; when these are depleted, then those pulse qualities will not occur.
Potentially there is an immense range of combinations of the pulse parameters; it is the interaction of these and their various manifestations that produces unique pulses that do not fit easily into the discrete pulse images presented in the literature. In such instances, recording and noting the pulse in terms of its constituent parameters allows important diagnostic information to be available for use, rather than lost within an incorrect application of a pulse quality name.
6.1. Introduction
The term pulse parameters refers to the fundamental variable characteristics that contribute to the formation of the radial arterial pulse. The 27 traditional CM pulse qualities form when there are specific changes in these parameters. A traditional pulse quality can form when there is a change in a single parameter only; other traditional pulse qualities form when there are changes in several parameters. In the pulse parameter system of radial pulse diagnosis, we have identified 9 pulse parameters that determine the 27 CM pulse qualities:
• Rate
• Rhythm
• Arterial width
• Depth
• Length
• Arterial tension
• Ease of occlusion
• Force
• Pulse contour.
6.1.1. Parameters and the arrangement of the CM pulse qualities
In Chapter 6 and 7 we present each of the 27 specific CM pulse qualities in conjunction with their relevant defining parameter(s). A pulse’s defining parameter refers to the variable change in the presentation of the pulse that is most apparent. For example, the Rapid pulse is defined by an increase in the frequency of pulsations. Consequently, the Rapid pulse’s defining parameter is pulse rate.
Where distinct changes in two or more parameters are involved in the formation of the CM pulse quality, we have categorised the CM pulse quality by using the parameter that plays the most important role in its formation. For example, the Skipping pulse features interruptions to the pulse’s regular rhythm and is accompanied by an increase in pulse rate. Yet it is the rhythm changes that are its most defining parameter and it is consequently categorised under the rhythm parameter.
However, this categorising of the pulse qualities is by no means the only way to classify them. Some of the more complex CM pulse qualities presented in Chapter 7 could be classified under more than one parameter. Categorising a pulse based on parameters is flexible.
Depending on the number of parameters involved in a pulse’s formation, the traditional CM pulse qualities can be additionally categorised as simple or complex. Simple refers to pulse qualities that are defined by a change in one parameter only, like the Rapid pulse. Complex refers to pulse qualities that are defined by a change in two or more parameters, such as the Firm pulse. The terms ‘simple’ and ‘complex’ can equally apply to the pulse parameters themselves. For example, pulse rate is a simple pulse parameter as it is characterised only by the pulse frequency. In contrast, pulse force is a complex pulse parameter because it depends on a range of variables such as the strength of cardiac contraction, blood volume and the tensile compliance of the arterial wall. It is how these variables combine that determine the force of the pulse.
In addition to presenting the traditional 27 pulse qualities with their relevant defining parameters, we also present the pulses according to the complexity of their defining parameter. Each of the parameters are defined, assessment techniques are detailed and the related CM pulse qualities noted along with their clinical significance. Simple pulse parameters and the related CM pulse qualities are presented in this chapter. Complex pulse parameters and related CM pulse qualities are presented in Chapter 7.
6.2. The simple pulse parameters
The simple pulse parameters covered in this chapter are:
• Rate
• Rhythm
• Depth
• Length
• Width.
Related changes in these five parameters are associated with 12 of the 27 traditional CM pulse qualities. The CM pulse qualities associated with the simple pulse parameters are:
• The Slow, Rapid and Moderate pulses (defined by rate)
• The Skipping, Bound and Intermittent pulses (defined by rhythm and accompanied by changes in rate)
• The Sinking, Floating and Hidden pulses (defined by level of depth)
• The Long and Short pulses (defined by length)
• The Fine pulse (defined by its width).
These pulses can be classified as simple pulse qualities because they are generally defined by a change in a single parameter. Exceptions are the Bound pulse and Skipping pulse, which form as a result of changes in two parameters, rhythm and rate. However, the Bound pulse and Skipping pulse are still considered ‘simple’ pulse qualities as they are defined by two of the most objectively evaluated parameters.
These five parameters are also defined as simple because they are relatively easy to assess in a clinical context. Indeed, these five parameters are deemed the least subjective of the nine parameters, involving the evaluation of distinctive physiological characteristics of the artery and the pulse wave. For example, manual palpation of the radial arterial diameter is assessed for the parameter of width. Pulse length is assessed by the presence or absence of pulsations at Cun, Guan and Chi pulse positions and beyond these positions. The parameter of depth entails an appraisal of the levels of depth where pulsations are relatively strongest. The rate and rhythm of the pulse can be calculated with standardised formulae of beats per minute in the case of rate, and comparison of the length of intervals between beats for rhythm. Pulse rate and rhythm can also be accurately assessed using electronic devices such as electrocardiography, and arterial width can be measured using Doppler ultrasound.
In a biomedical context, the three parameters of rate, rhythm and width are used primarily to provide information about the functional performance of the cardiovascular system, particularly the heart. The parameters of depth and length are not extensively used in the biomedical diagnostic sense, but are used as an indicator of the circulatory system’s integrity. This is best seen in acute traumatic injury of the limbs in which circulation may be compromised through swelling and fractures causing arterial occlusion, and also occurs in chronic conditions in which arteries narrow and blood flow is impeded. Palpating the length of the artery is useful in identifying the point of arterial occlusion, and pulse depth is used to assess the strength of blood flow and pressure in the vessel.
6.3. Rate
Three traditional CM pulse qualities are associated with the pulse rate parameter:
There are clear guidelines in the literature that detail when to interpret pulse rate measures outside the normal stated pulse rate range as healthy. This often depends on a range of variables including gender, age and exercise. Therefore, in clinical practise it is important to record the pulse rate every time you palpate an individual’s pulse, to establish a normal baseline measure for their particular pulse rate.
6.3.1. Pulse rate and its measurement
The pulse wave that we ultimately feel in the radial artery originates in the heart, due to the rhythmic contraction (systole) and relaxation (diastole) of the heart’s left ventricle as it pumps blood throughout the body. Each systole and the following diastole is known as one cardiac cycle . Therefore, pulse rate is an expression of the heart rate, describing the number of times the cardiac cycle occurs each minute.
Assessment of pulse rate involves noting the presence of pulsations and the frequency with which these occur in one minute. Although pulse rate is expressed in beats per minute, it isn’t always necessary to assess the pulse frequency for a full minute. For example, one method for assessing pulse rate involves counting the number of beats for 15 seconds then multiplying this value by 4, or counting the number of beats for 30 seconds, then multiplying this value by 2, to obtain a measure of pulse rate in beats per minute (bpm).
The assessment method used for obtaining a measure of pulse rate should be repeated at least twice and the findings averaged. This is useful in two ways. Firstly, it assists in determining the accuracy of the value obtained for the pulse rate. Secondly, by obtaining a second measure of pulse rate, any transient changes affecting heart rate are more readily identified by noting any large variations between the two measured values. This also increases the reliability of pulse rate assessment. (See Box 6.1 for further considerations when interpreting pulse rate diagnostically.)
Box 6.1
Questions to consider when assessing pulse rate
• Is this a first-time patient?
• Has the patient been hurrying to the appointment?
• Are they nervous or stressed?
• Does the patient exercise regularly? What type of exercise do they do?
• Have they exercised recently before their appointment?
• Have they taken any medications/supplements?
• Has the patient consumed tea or coffee recently? Are there any other dietary sources of caffeine, for example carbonated or energy drinks, herbal supplements?
• Is the pulse wave rising slow, normal or fast?
• Is there aversion to heat or cold?
• Is a fever present?
• What is the weather like?
6.3.1.1. Pulse rate versus heart rate
The terms pulse rate and heart rate are often used interchangeably to mean the same thing. This is based on the assumption that since heart contraction produces the pulse wave, all pulse movements felt at the radial artery should correspond to the same number of heart contractions. However, there are certain biomedical conditions affecting the heart and arterial structures in which two distinct pulse waves can be felt for every heart contraction. Sometimes the heart contraction can be weak and the pulse wave cannot be felt in the radial artery. In other cases the pulse is being occluded, as in thoracic outlet syndrome. It should be noted then that in certain circumstances, the pulse rate and the heart rate do not correspond.
6.3.2. Normal pulse rate
The average resting pulse rate in a healthy adult is about 70–80 bpm, but this ‘normal’ range is usually extended to 60–90 bpm. Normal pulse rate will also vary depending on the level of physical activity. In a healthy adult, it can decrease to 40 bpm during sleep. At the other extreme, pulse rates of up to 180 bpm may occur during intense exercise (Epstein et al 1992: p. 7.9).
6.3.3. Variables affecting pulse rate
Of all the pulse parameters, pulse rate is the most variable. It is easily affected by several factors, including:
• Gender
• Age
• Exercise
• Medications
• Body temperature
• Emotions.
6.3.3.1. Gender and pulse rate
Estes (2006: p. 253) asserts that women have a slightly faster resting pulse rate than men:
• Women: 72–80 bpm (average 75)
• Men: 64–72 bpm (average 68)
Gender-related pulse rate differences are thought to result from the relative size of the heart. Men have relatively larger hearts than women resulting in a greater proportion of blood being pumped through the arterial system with each cardiac contraction. In women, if the heart is relatively smaller, to maintain the same blood volume movement as men the heart rate needs to increase. (This gender difference is a generalisation, as commonly both men and women will have normal resting heart rates greater than or less than the ranges listed.)
6.3.3.2. Age and heart rate
There is an inverse relationship between heart rate and age; heart rate decreases slightly with increasing age. This is a result of decreasing responsiveness of the β-adrenergic receptors in the cardiac cells to chemical stimulus, combined with decreasing sinoatrial node automaticity (McCance & Huether 2006) (see the description of the intrinsic conduction system in section 6.4.5).
From a CM perspective this correlates to Yang Qi decreasing with age. Children and infants, considered to have more Yang Qi intrinsically, have a significantly higher heart rate, with newborns likely to have a heart rate of 140 bpm. Resting heart rate for a fetus can be as high as 140–160 bpm (Marieb 2001: p. 708). Table 6.1 lists a range of normal heart rate ranges for different age groups.
| Age (years) | Range (bpm) | Average (bpm) |
|---|---|---|
| Newborn | 100–170 | 140 |
| 1 | 80–160 | 120 |
| 3 | 80–120 | 110 |
| 6 | 70–115 | 100 |
| 10 | 70–110 | 90 |
| 14 | 60–110 | 85–90 |
| Adult | 60–100 | 72 |
| Adult men | 64–72 | 68 |
| Adult women | 72–80 | 75 |
The relationship between age and heart rate is clinically reflected in the diagnostic interpretation of the resting heart rate. For example, a slow heart rate occurring in a younger person, when not associated with any form of aerobic training, is seen as a poor sign of health. In older people, Perk et al (2003) found a strong correlation between heart rate and all-cause mortality in elderly women in a study examining the relationship between heart rate and mortality in the elderly (average age of subjects was 70 years). Although there was a similar trend for elderly men, this was not statistically significant. Perk et al (2003) found that women with a heart rate greater than 77 bpm had three times the mortality rate of those whose heart rates were less than 77 bpm (r = 0.25, P = 0.0003). This means that a relatively fast resting heart rate (that is, on the higher side of the normal range) in an older person is a mortality risk sign and can be viewed as a sign of poor health (Perk et al 2003). In a CM context, this probably reflects vacuity of the heart associated with depletion of essential substances, notably Qi.
6.3.3.3. Exercise and heart rate
Like any other muscle in the body, the more exercise the heart receives the better toned it becomes and therefore the more efficient in moving blood. This is particularly noticeable in individuals who undertake endurance training and consequently have a slower than normal resting heart rate (50–60 bpm) with elite athletes resting heart capable of falling below 50 bpm (McCance & Huether 2006: p. 1048). A slower heart rate in this situation results from:
• Increased vagal stimulation (which slows the heart) and decreased sympathetic stimulation
• Increase venous return of blood to the heart due to lowered peripheral resistance leading to increased stroke volume.
Stroke volume (SV) is the amount of blood pumped out by a ventricle with each heartbeat. As the heart rate (HR) slows down, this allows longer ventricular filling, which in turn increases stroke volume. The relationship between SV and HR is termed cardiac output (CO), defined as the amount of blood that is pumped out by each ventricle in one minute and dependent on the heart rate and stroke volume:
Therefore, increased SV helps to compensate for a slower rate to maintain CO.
When cardiac fitness is poor, the heart functions less efficiently and so SV is diminished, with less blood being ejected from the heart with each cardiac contraction. In this situation, the HR increases to maintain CO. In individuals who exercise little, or whose cardiac muscle tone is poor, their normal resting heart rate is consequently raised.
6.3.3.4. Medication, herbal supplements and heart rate
There are many medications and herbal supplements that affect heart rate, and appropriate texts should be referenced for further information. Many of the routinely used over-the-counter medications such as cold and flu medications contain compounds such as pseudoephedrine (a decongestant) that may cause heart and pulse rate to increase. Common asthma-relieving medications such as salbutamol, found in bronchodilators, are β-adrenergic agonists which may cause an increased heart rate or tachycardia in some patients. Many herbal medicines and supplements such as guarana (Paullinia cupana), aconite (Fu zi, Aconitum carmichaeli) and ephedra (Ma Huang, Ephedra sinica) have stimulant effects on the heart and pulse rate. Nicotine also has a stimulatory effect on pulse rate (while cannabis has a primary effect on the pulse contour). Digitalis and other drugs such as beta-blockers, which block the β-adrenoreceptors and prevent stimulating chemicals from attaching, may slow down the heart rate.
6.3.3.5. Body temperature and heart rate
An increase in body temperature results in increased heart rate because of a rise in the metabolic rate of cardiac cells. This is commonly seen with fever. Conversely, a decrease in body temperature can slow down heart rate and contractility. Individuals exposed to cold and suffering hypothermia routinely present with slowed heart rates. In a CM context, cold is seen as retarding the body’s Yang Qi and so the pulse slows.
Generally, environmental conditions associated with the seasons similarly affect the pulse. In summer, the pulse is felt strong, relatively superficial and slightly fast, and this is seen as a ‘normal’ response to the environment rather than a pulse representing pathology. Cold weather or seasonal conditions can cause the arterial tension to increase, and pulse width may decrease in an attempt to maintain body warmth. The classical CM literature also described the pulse as being deeper in winter.
6.3.3.6. Emotions such as fear, excitement, anxiety or stress
Extremes of emotion may cause changes in heart rate. Anxiety may cause tachycardia, commonly experienced as a ‘panic attack’. Depression may affect the Shen, thereby affecting the heart’s control of blood and the vessels. Stress stimulates the sympathetic nervous system increasing production of epinephrine (adrenaline) and elevating body heat as a consequence of increased metabolic activity (Estes 2006: p. 255). As noted previously, increase in body temperature can increase heart rate.
6.3.3.7. Pregnancy and heart rate
Early in the first trimester of pregnancy a number of hemodynamic changes take place in order to meet the demands of the growing foetus. Increased cardiac output is due to an increase in both heart rate and stroke volume. The increase in heart rate occurs as early as 4 weeks after conception and increases on average by about 15 bpm (Stables & Rankin 2005: p. 233).
6.3.3.8. Other causes affecting heart rate
There are a number of factors additionally associated with changes in the pulse rate parameter and which are always seen as a pathological response. These include (but are not limited to):
• Decreased potassium (hypokalemia), which delays ventricular repolarisation and may have varying effects on rate; bradycardia — a slow pulse, atrioventricular block or paroxysmal atrial tachycardia (McCance & Huether 2006: p. 105).
• Inhibition of the vagus nerve can cause tachycardia (McCance & Huether 2006: p. 1049).
• Shock and hypovolemia (low blood pressure) due to blood loss, plasma loss or interstitial fluid loss. Initial compensatory mechanisms include increases in heart rate and systemic vascular resistance to elevate cardiac output, by release of catecholamines by the adrenals (McCance & Huether 2006: p. 1628).
• Thyroid hormones cause changes in heart rate. Hyperactivity or hypoactivity of the thyroid affects metabolism and core body temperature (McCance & Huether 2006: pp. 692-5).
6.3.4. Regulation of heart rate: CM perspective
The rate of the pulse provides a general indication of the functional activity of Yang Qi in the body (Box 6.2). Yang Qi is seen as a motive force, giving rise to and ensuring the regularity of the movement of both Qi and blood:
Box 6.2
Traditional CM method of pulse rate assessment
The objective evaluation of heart rate with a timepiece such as a watch was not available at the time the CM classics were written. Instead, a method was devised for the purpose of evaluating whether the pulse rate was faster or slower than it should be. This method was based on the number of beats per complete respiration cycle of the patient (one inhalation and one exhalation) or the respiratory rate of the practitioner, depending on the CM literature reviewed. The following quote from the Su Wen Nei Jing describes this approach:
In man,
during one exhalation, the vessels exhibit two movements.
During one inhalation, the vessels exhibit two movements too.
Exhalation and inhalation constitute one standard breathing period.
If the vessels exhibit five movements,
this is an intercalation [of a fifth movement] because of a deep breathing.
That is called a ‘normal person’.
Su Wen
From the pulse literature, the normal pulse rate per complete respiration cycle breath should be 4–5 pulse beats (see Table 6.2 for age-related respiratory rates). A later expansion of the Su Wen passage by a commentator suggested that a patient’s condition should be assessed by making a comparison with the pulse frequency of someone who is not ill, such as the healthy physician.
Disadvantages of the traditional method of pulse assessment
The obvious disadvantages of the respiratory method include:
• The assumption that the practitioner is in good health and therefore has a ‘normal’ rate of respiration to provide a reliable baseline comparison. This is not always the case.
• Lack of agreement between literature sources relating to the use of the respiratory rate of the practitioner or the patient as the baseline comparison.
• If using the patient’s respiratory rate, it may be difficult to observe the complete respiratory cycle, as it is not always easy to see inspiration and expiration clearly, particularly if the patient’s breathing is shallow or irregular.
That which is quiet is Yin; that which moves is Yang
That which is retarded is Yin; that which is accelerated is Yang.
Su Wen 7
The pulse rate is affected when the Yang Qi is affected. In this context, changes in pulse rate occur when Yang Qi is affected by:
• External factors causing heart rate to increase or decrease depending on whether the cause is of a hot or cold nature. External factors include dietary and pathogenic causes.
• Internal factors causing heart rate to become hyperactive (often due to Yin vacuity so the Yang is no longer controlled) or hypoactive (through Yang Qi vacuity, in which the Yang Qi is no longer sufficient to move the heart and blood) at its customary rate.
Additional changes in the pulse parameters of force (generally increased in replete patterns and decreased in a vacuous patterns) and depth are used to further differentiate the pulse rate changes and the causes. Information obtained from assessment of the pulse rate parameter is always used with information obtained from the assessment of other pulse parameters. Pulse rate assessment alone does not supply sufficient information to identify the location (internal or external) or the nature (vacuity or replete) of disease/dysfunction.
6.3.5. Regulation of heart rate: biomedical perspective
From a biomedical perspective, there are three regulatory mechanisms which control heart rate (the following information is from McCance & Huether 2006):
• Intrinsic conduction system: The fundamental rhythm of the heart is set by the sinoatrial (SA) node, a small area of cells that function as a pacemaker due to their spontaneous electrical nature. They continuously depolarise and initiate action potentials that spread to the rest of the heart, via a conduction system, causing it to contract. The conduction system includes the atrioventricular (AV) node, the AV bundle (bundle of His), the right and left bundle branches and the Purkinje fibres (conduction myofibres).
• Autonomic nervous system (ANS): The ANS (parasympathetic and sympathetic divisions) helps to modify the heart rate according to the needs of the body. The sympathetic nervous system is activated in times of stress, excitement and exercise, the ‘fright, flight or fight’ response. It increases heart rate by stimulating the release of norepinephrine (noradrenaline), making the pacemaker fire more quickly.
• Chemical factors: Hormones such as epinephrine (adrenaline) and norepinephrine (noradrenaline), from the adrenal medulla, increase both heart rate and contractility. Thyroid hormones have a similar effect. Growth hormone and pancreatic hormones may also affect heart rate (McCance & Huether 2006). Changes in concentrations of potassium (K+), calcium (Ca2+) and sodium (Na+) ions affect heart rate through affecting the depolarisation threshold of nerves and muscle contractility. (Refer to appropriate physiology texts for further information.)
6.4. CM pulses defined by rate
6.4.1. Slow pulse (Chí mài) 

6.4.1.1. Requisite parameters
The Slow pulse is a simple pulse quality defined solely by the pulse rate.
It is characterised by a decrease in pulse rate to below the normal range of 60–90 bpm.
6.4.1.2. Clinical definition
The Slow pulse has a rate that is less than or equal to 60 bpm.
6.4.1.3. Classical Description from Mai Jing
The Slow pulse is a pulse that beats three times for one respiration, very slow in coming and going
‘Three beats for one respiration’ refers to the number of pulsations per one inhalation and one exhalation or one respiratory cycle (Table 6.2).
| aCaused by barbiturates, alcohol, narcotics, head injury depressing respiratory centre. |
|||
| bCaused by hypoxia, metabolic acidosis, stress, anxiety-respiratory rate is elevated due to the release of catecholamines. Modified from Estes (2006: pp. 250–251). |
|||
| Age (years) | Range | Average | Equivalent bpm using CM theory of 4 beats/breath |
|---|---|---|---|
| Newborn | 30–50 | 40 | 40 |
| 1 | 20–40 | 30 | 120 |
| 3 | 20–30 | 25 | 100 |
| 6 | 16–22 | 19 | 76 |
| 10 | 16–20 | 18 | 72 |
| 14 | 14–20 | 17 | 68 |
| Adult | 12–20 | 18 | 72 |
| Bradypneaa | <12/minute | <48-60 | |
| Tachypneab | >20/minute | >80–100 | |
6.4.1.4. CM indications for the Slow pulse
The Slow pulse can be considered a sign of either good health or pathology.
Slow pulse indicating health
The Slow pulse may be a ‘healthy’ pulse, often observed in athletes, denoting cardiac fitness. In elite individuals, the resting normal heart rate may be below 50 bpm. From a CM perspective, this is seen as clear and unobstructed flow of Qi and blood. A healthy slow pulse would form when Heart Qi is strong and Blood is abundant.
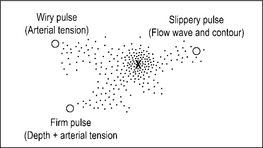
A healthy slow pulse can be differentiated from an unhealthy slow pulse by two factors (Fig. 6.2, Table 6.3):
• Length of interval between beats
• Duration of systole, also known as ejection duration.
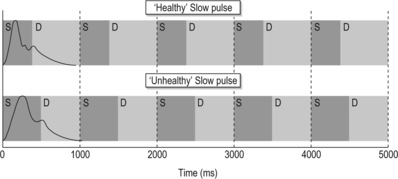 |
| Figure 6.2Variation between the systolic (S) and diastolic (D) components of the pulse wave between the formation of a healthy slow pulse and an unhealthy slow pulse. |
| Pulse presentation | Signs and Symptoms | Physiological response | |
|---|---|---|---|
| Yang vacuity | Slow and forceless | Desire for warmth, no thirst, bright-pale face, cold limbs | Long systole, small pulse amplitude |
| Pathogenic cold | Slow and forceful | Pain, thirst for warm drinks, pale face, cold limbs | Normal systole, increased amplitude, increased arterial tension |
| Pathogenic heat | Slow and forceful | Heat signs such as fever, abdominal pain | Normal systole, increased amplitude |
| Health | Slow and forceful | No cold or heat signs. No aversion to cold or heat | Short systole, long diastole |
There is also a third differential factor, but this is more subjective or sensory dependent. Constant (1999: p. 32) describes this as the sense of a ‘tap’ against the fingers. When the heart contracts strongly and quickly, the pulse wave also expands quickly to its peak and this is felt as a ‘tap’ against the fingers. When the heart contraction is slower, the pulse may rise or lift against the finger but there is no tap.
Slow pulse indicating pathology
According to CM theory, ‘When Qi moves, blood moves’ (Flaws 1994: p. 58). Therefore decreased movement of Qi leads to decreased flow rate of blood. This occurs in two ways:
• The presence of strong pathogenic Cold may result in a decrease in pulse rate. ‘Cold leads to the contraction of Qi’ (Flaws 1994: p. 59) and this retards the movement of Qi and blood.
• A vacuity of Yang Qi may result in a pulse rate slower than normal, as there is insufficient Yang Qi to propel the blood normally.
As a pathological pulse type, the Slow pulse may indicate three possible patterns:
Invasion of external pathogenic cold (Slow and forceful)
Cold has a contracting nature, causing contraction of both blood vessels and muscles and resulting in constrained flow of Qi and blood. It acts as a counter to the Yang’s warming and expansive nature and constrains the movement of Qi, contributing to a slowing of the heart rate. The presence of an external pathogenic factor will be felt as an increase in the force of the pulsation. (See the Floating pulse and the Tight pulse for specifics on the pulse in the presence of an external pathogenic agent (EPA) of Cold).
Vacuity of Yang Qi (Slow and forceless)
Yang Qi provides the motive force to move blood. ‘When Qi moves, blood moves’ (Flaws 1994: p. 58). Consequently, deficient Yang Qi will lead to impaired flow of blood. The Nei Jing notes in Chapter 18 that, compared to that of a ‘normal’ pulse, a pulse that beats only twice per complete respiration signifies a deficiency of Qi.
When man exhales once and his vessels exhibit one movement and when he inhales once and his vessels exhibit one movement, that is called ‘short of Qi’.
Pathogenic heat
Lu (1996) describes an occurrence of the Slow pulse in the presence of pathogenic Heat in the intestines causing obstruction. Heat causes fluids to congeal, so obstruction of Yang Qi leads to a Slow pulse, but the pulse is forceful and accompanied by signs and symptoms associated with heat rather than cold signs.
6.4.1.5. Biomedical perspective
Termed bradycardia, the pathological Slow pulse is defined as having a heart rate slower than 60 bpm which is accompanied by a systole that is slower (or longer) than normal. This can be due to a number of factors including low body temperature, medication such as digitalis, hypothyroidism, heart problems and electrolyte imbalances (Ca2+, Na+, K+). Carotid sinus syndrome can result in bradycardia due to hypersensitivity of the carotid artery walls to pressure. Mild external pressure triggers a strong baroreceptor reflex which results in vagal stimulation that has a parasympathetic effect, thus slowing the heart rate (Guyton & Hall 2006: p. 148).
Pathologically, an extremely slow pulse may be due to heart block, where there is impairment of the normal electrical conduction pathway through the heart that causes normal cardiac contraction. (In CM this is viewed as Heart Yuan Qi vacuity.) There are different degrees of heart block, linked to the level of impairment of the heart’s conduction system. Signs range from delayed heart contraction through to compromised circulation and eventual heart failure. Treatment protocols also vary, ranging from medications to physical insertion of an artificial pacemaker to replace the heart’s own natural pacemaker (SA node: see section 6.3.5).
6.4.2. Rapid pulse (Shuò mài)

6.4.2.1. Requisite parameters
The Rapid pulse is a simple pulse quality defined only by changes in the pulse rate parameter. There is an increase in pulse rate above that of the normal heart rate range, 60–90 bpm.
6.4.2.2. Clinical definition
The rate of the Rapid pulse is greater than or equal to 90 bpm.
Note that the rate of 90 bpm for classifying a rapid pulse is different from the biomedical definition of a rapid pulse or tachycardia, commonly listed as 100 bpm. See 6.4.2.5 Biomedical Perspective, below, for further information. Also see Box 6.3, Racing pulse.
Box 6.3
Racing pilse 

There is a subcategory of the Rapid pulse called the Racing pulse. The Racing pulse is defined by a pulse rate greater than 120 bpm, or seven or more beats per respiration cycle. According to Deng (1999: p. 113), the pulse was first described in the Zhen Jia Shu Yao around 1000 ce, and expanded on in the Ming dynasty text Zhen Jia Zheng Yan . The Racing pulse is similar to the biomedical definition of tachycardia, with a similar description of aetiology and conditions in which it manifests such as thyrotoxicosis and high fevers reflecting an increased metabolic rate. It may be associated with some forms of compromised cardiac function.
6.4.2.3. Classical description from the Mai Jing and Nei Jing
The rapid pulse is a pulse coming and going abruptly and urgently [beating 6–7 times in one respiration in another version; named an advancing (pulse) in yet another]
(Mai Jing; (Wang, Yang (trans) 1997: p. 3).
Rapid is defined as more than five beats per breath of the doctor
(Nei Jing;Ni (trans) 1995: p. 31).
6.4.2.4. CM indications for the Rapid pulse
The Rapid pulse may indicate health or pathology depending on the age of the individual.
Health
In children, a rapid pulse is considered ‘auspicious’ or favourable (Li, Flaws (trans) 1998: p. 75), as children’s pulses are usually more rapid than those of adults. This is attributable to their Yang nature and so a rapid pulse is an appropriate pulse to manifest. The Mai Jing notes specifically that ‘In children between four and five years, the pulse is fast, beating 8 times per respiration’ (Wang, Yang (trans) 1997: p. 10). The normal pulse rate for adults is described as 4–5 beats per respiration, which means that the normal children’s pulse rate is twice that of adults when using the old respiration method.
Pathology
In an adult, the Rapid pulse always indicates pathology involving heat or hyperactivity of Yang. Any hyperactivity of Yang Qi may augment pulse movement of Qi and blood, resulting in an increased heart rate. This may indicate the presence of pathogenic Heat or Fire, as seen in febrile diseases. Alternatively, a rapid pulse may also result from an inability of Yin to control Yang, allowing Yang to move without its usual constraints:
When the Yin fails to contain the Yang, the flow in the channels will become rapid, causing the Yang Qi to become excessive and reckless.
(Wei Jing Su Wen)
This may be due to a deficiency of Yin fluids such as blood or body fluids arising from blood loss in haemorrhage, or depletion of Yin fluids following febrile disease, through excessive sweating or diarrhoea. Accordingly, two main patterns are associated with a pathological Rapid pulse:
An increase in Yang supplements the body’s Yang Qi in moving Qi and blood. Consequently, the pulse rate increases (changes in other parameters such as contour and possibly arterial width and length may also be present). Repletion of Yang is often attributable to external variables, such as the presence of an external pathogenic factor producing fever. Dietary factors such as alcohol, herbs and spices may also supplement the body’s Yang. In this situation the pulse will be Rapid and forceful (see section 6.8.1 for further information).
Yin vacuity producing heat (rapid and forceless)
Yin vacuity may occur as the result of loss of Yin fluids through excessive sweating, vomiting, diarrhoea or blood loss. As the relative amount of Yin (in the form of fluids) has decreased then there is a relatively excessive amount of Yang producing heat. As such, the term, ‘Yin vacuity producing heat’ refers to the creation of heat in the body because Yin is vacuous. Poor sleep and overwork are lifestyle factors which have an cumulative affect over time of depleting Yin.
From a biomedical perspective Yin vacuity can be associated with a relative increase in the sympathetic nervous system due to an inability of the parasympathetic nervous system to maintain appropriate control over these aspects. For example, stress can cause palpitations (see section 6.5.4) and digestive disturbances (Wood attacking the Earth); conditions such as irritable bowel syndrome (IBS) are affected by stress, producing bouts of either constipation or diarrhoea. Additionally, Guyton & Hall (2000) note that the ‘contractile strength of the heart often is enhanced temporarily by a moderate increase in temperature, but prolonged elevation of the temperature exhausts the metabolic systems of the heart and eventually causes weakness’ (p. 106).
There are two possible effects on the pulse wave when Yin becomes vacuous. These are:
– If Yin is vacuous then it is no longer able to control (or constrain) the movement and function of Yang. Therefore the flow rate of Qi and Blood in the arteries increases, manifesting as an increase in heart rate.
– As Yin’s function of anchoring Yang may be affected, the pulse could also present relatively stronger (but overall is not actually forceful) at the superficial level as Yang ‘floats’, moving upwards and outwards, in addition to an increase in heart rate.
6.4.2.5. Biomedical perspective
Tachycardia or tachyarrythmia is defined as an abnormally fast heart rate (>100 bpm) that may be transient or ongoing. When heart rate increases there is inefficient filling of the left ventricle during diastole and stroke volume is diminished. Whether due to poor refill during diastole or shortened ejection duration with systole, the result of tachycardia is often a compromised circulation of blood affecting tissue perfusion, especially over the longer term (Box 6.3).
Guyton & Hall (2006: p. 147) note three general causes of tachycardia:
• Increased body temperature
• Sympathetic nervous system stimulation of the heart
• Toxic conditions of the heart.
Tachycardia may also result from acute emotional stress such as anxiety, increased body temperature associated with fever or exercise (Box 6.4), blood loss and anaemia reducing effective blood volume or medication stimulating the pacemaker, or as a reflexive response from heart disease in an attempt to maintain normal circulation. Box 6.5 lists some conditions associated with tachycardia.
Box 6.4
Heart rate and temperature
Guyton & Hall (2006: p. 197) assert that heart rate increases by 18 bpm for each °Celsius increase in body temperature to 40.5 °Celsius. Beyond this the heart weakens and so pulse rate may slow. HR increases with fever because the increased temperature stimulates the SA node’s metabolic rate, excitability rate of rhythm.
Box 6.5
Conditions associated with tachycardia
• Sinus tachycardia
• Atrial and ventricular fibrillation (heart Qi or Blood stagnation; heart shock)
• Hyperthyroidism (which may equate to Yin vacuity)
• Febrile diseases (Yang excess)
• Haemorrhage
• Pregnancy. In the third trimester normal resting heart rate increases by 10 bpm and cardiac output increases by 40% due to increased stroke volume (Braunwald et al 2001: p. 25)
• Chronic rheumatic heart disease may result in damage to the heart structure such as heart valves, as well as conduction defects leading to atrial fibrillation
From both CM and biomedical perspectives, the conditions listed above are accompanied by changes in other pulse parameters, not just pulse rate alone.
The body’s response to stress is a common cause of tachycardia. Stress initiates neuroendocrine processes, leading to the release of epinephrine (adrenaline) and norepinephrine (noradrenaline), as well as other hormones from the pituitary and adrenal glands (‘fright, flight or fight’ response). Norepinephrine (noradrenaline) constricts smooth muscle in all blood vessels and therefore plays a major role in peripheral vasoconstriction. Epinephrine (adrenaline) is responsible for increasing heart rate and also for the force of myocardial contraction.
Atrial fibrillation is a form of tachycardia, involving increased impulses affecting the contraction of the atria. (A number of the CM pulse qualities are due to atrial fibrillation.) As atrial fibrillation can also result in irregular rhythm, it is discussed in section 6.5 on Rhythm.
Hyperthyroidism increases heart rate considerably because the thyroid hormone appears to directly cause heart excitation. Thyroid hormone may also increase cardiac output and blood flow (Guyton & Hall 2006: p. 937).
Haemorrhage may also cause an increase in heart rate, as part of a cardiovascular compensatory mechanism to increase circulating volume by pulling fluids from the interstitium. This dilutes the viscosity of blood, resulting in faster blood flow. In addition, hypoxia results in vasodilatation of blood vessels, also increasing blood flow. As a result venous blood return is increased and the heart needs to pump faster and harder to get oxygenated blood to the body and prevent cardiopulmonary congestion (McCance & Huether 2006: p. 929).
6.4.3. Moderate pulse (Hûan mài) 

6.4.3.1. Alternative names
Leisurely, Slowed Down, Relaxed, Retarded or Languid pulse.
6.4.3.2. Requisite parameters
The Moderate pulse is a simple pulse that has changes in two pulse parameters:
• Rate: There may be either an increase or decrease in rate dependent on the individual’s ‘normal’ resting heart rate.
• Contour: The pulse shape is rounded (see Slippery pulse, section 7.9.1).
The Moderate pulse is initially identified by the pulse rate (Table 6.4) and further differentiated from the standard Slow pulse by the shape of the pulse contour.
| Pulse rate (bpm) | Pulse quality/category | Biomedical | Possible indications | Traditional (Beats per respiration) |
|---|---|---|---|---|
| <60 | Slow pulse | Bradycardia | Health | 3 |
| Cold EPA Heath Damp | ||||
| Heath Damp | ||||
| 60 | Moderate pulse Slow pulse | Yang vacuity | 4 | |
| 61–80 | Normal pulse rate | Normal pulse rate | Health | 4-5 |
| 81–89 | Borderline normal to rapid | Health | 5–6 | |
| Unhealthy heart | ||||
| Blood vacuity | ||||
| Recovery phase | ||||
| Progression of illness | ||||
| 90–119 | Rapid pulse | Tachycardia | EPA Heat | 7-8 |
| Vacuity Heat | ||||
| >120 | Racing pulse | Heat/Fire | ≥8 | |
| Infections | ||||
| Dehydration | ||||
| Extreme fevers |
6.4.3.3. Clinical definition
The Moderate pulse has a pulse rate of 60 bpm, with a distinctly rounded contour felt under the palpating fingers.
6.4.3.4. Classical descriptions from the Nei Jing and Mai Jing
A pulse that is neither too strong nor too weak, that comes and goes in a rhythmic fashion, flowing like a stream … (Nei Jing)
The moderate pulse is also a pulse slow in coming and going but a little faster than the slow pulse …’ (Mai Jing)
6.4.3.5. CM indications
The Moderate pulse can be either healthy pulse or pathological, depending on the signs and symptoms accompanying it.
Health
It is a normal pulse rate in a healthy person if no other change in pulse characteristics accompany it, or when there are no other presenting pathological signs and symptoms. In this situation it is a sign of a strong constitution. When this occurs, it could be classified both as a Slow pulse, due to the rate, but also a Slippery pulse, and would be a sign of sufficient Qi and blood.
Pathology
The Moderate pulse is often associated with the presence of Damp or vacuity of the Stomach and Spleen, especially Spleen Yang Qi deficiency. Therefore, it would occur in conjunction with signs and symptoms associated with such patterns. This could include digestive symptoms such as loose stools, fatigue and tiredness, cold limbs, fluid retention and an aversion to cold.
Pathogenic damp is broadly seen as a Yin condition and tends to injure Yang. In addition, damp is heavy, slowing down and impeding the flow and circulation of Qi and blood. ‘Phlegm and Dampness lead to Qi obstruction; Qi obstruction leads to Qi stagnation’ (Flaws 1994: p. 79).
6.5. Rhythm
Pulse rhythm is an expression of the heart’s functional capacity to contract and relax in a consistent fashion. Rhythm as such is not how frequently the heart contracts — this is pulse rate — rather, it is whether the heart is sufficiently contracting at all.
A normal pulse has a regular rhythm, with a consistently even interval between each pulsation. When the intervals between pulsations vary in length or there appears to be ‘missing’ beats or an interruption, this is said to be an irregular rhythm. Any pulse occurring with an irregular rhythm is termed an arrhythmia or dysrhythmia, or simply a pulse lacking a regular rhythm.
Arrhythmic pulses may have an interruption to their normal rhythm occurring at irregular or regular intervals. Interruptions range from pulses with occasional ‘missed’ beats or rapid beats, to serious rhythmic disturbances that impair the pumping action of the heart.
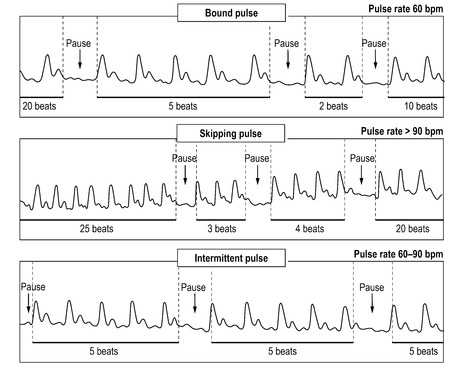
Three specific CM pulse qualities are associated with the rhythm parameter:
• Skipping pulse (section 6.6.1)
• Bound pulse (section 6.6.2)
• Intermittent pulse (section 6.6.3).
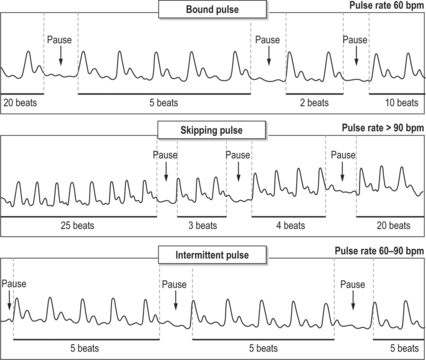
The Skipping pulse and Bound pulses have irregular interruptions to their normal rhythms and are further differentiated by pulse rate. The Intermittent pulse has regularly spaced interruptions to the normal rhythm and is defined only by the rhythm parameter.
6.5.1. Pulse rhythm and its assessment
The method for assessing pulse rhythm requires the pulse to be felt for an interval of at least 60 seconds. This is because irregularly interrupted pulses, with only occasional interruptions to normal heart rhythm, may not be detected in any shorter time frame. With the fingers placed on the artery, the practitioner notes the presence of pulsations and whether these are occurring at regularly spaced intervals.
When an irregularity in rhythm is detected, such as a ‘missed’ beat, the practitioner next needs to determine the nature and frequency of the interruption to normal pulse rhythm:
• Is the interruption to heart rhythm occuring regularly (that is, is it occurring at a consistent interval between each beat?)
• If so, how often does this occur? (number of rhythmic beats between each interruption to heart rhythm)
• Or, is the interruption to heart rhythm occurring only at irregularly spaced intervals: is there a missed beat only occasionally (no regular interval or specific number of beats between each missed beat)?
When assessing pulse rhythm, it is also important to inquire if the patient is aware of any irregularity in their heart rate, as this may not be apparent at the time of consultation (Box 6.6). Changes in heart rhythm may include palpitations and this will be discussed in 6.5.4.
Box 6.6
Clinical questions to ask your patient
• Are you aware of what your normal heart rate is?
• Are you aware that it is slower or faster than usual?
• If you have noticed changes to your HR does this occur suddenly or gradually?
• How long has this been happening?
• Is this happening all the time?
• Does this occur with any other symptoms?
• Is it better when you rest?
Sometimes an interruption to the pulse rhythm can be due to a blockage in the conduction of the pulse wave from the heart to the periphery (Box 6.7). It is therefore also important to compare the left and right radial pulses. Differences in rhythm between the two sides may indicate some type of problem with the arterial system, such as arterial blockage or aortic coarctation, rather than specific heart-related pathology (Constant 1999).
Box 6.7
Sinus arrhythmia
• Sinus arrhythmia is a normal occurrence often seen in young adults where the heart rate slightly speeds up during inspiration due to activation of neural input to the brain when the lungs are expanded (for example, deep breathing), and then slows down during expiration.
• Sinus arrhythmia often results from alteration of the strength of the nerve signal to the heart sinus node affecting the heart rate (Guyton & Hall 2000: pp. 134-135). Specifically, the mechanism affecting heart rate occurs during deep breathing when neural receptors in the lungs are activated.
•McCance & Huether (2006) state that the increase in heart rate during inspiration is caused by the stretching (activation) of vagal fibres in the lungs that cause heart rate to speed up by inhibiting the cardioinhibitory centre of the medulla. Inhibition of this centre allows unopposed sympathetic acceleration of heart rate (p. 1049).
• Sinus arrhythmia needs to be carefully differentiated from arrhythmia or dysrhythmia. A pulse is described as arrhythmic when there are pauses in the heart’s normal conduction system resulting in a perceived missed beat. With sinus arrhythmia there are no missed beats but rather a change in the length of time between beats. This is not deemed a pathological occurrence.
• The phenomenon of sinus arrhythmia was likely clinically observed by the authors of the Nei Jing, as evidenced by the following lines of text.
If the vessels exhibit five movements,
this is an intercalation [of a fifth movement] because of a deep breathing.
That is called a ‘normal person’.
(Su Wen)
This partial description of the normal pulse appears be an early reference to sinus arrhythmia and was clearly viewed as a variation of the normal healthy pulse rate.
6.5.2. Regulation of pulse rhythm: CM perspective
In CM the Heart governs the movement of blood. Heart Qi maintains the functional ability of the heart to contract. Rhythm is affected when Heart Qi is affected. In this context, changes in pulse rhythm occur when the heart Qi is exhausted or obstructed.
Changes in heart rhythm, especially rhythm changes associated with cardiovascular damage, can be the final common pathway for a number of diseases (AtCor Medical 2006: pp. 1-31). These include:
• Hypertension
• Left ventricular hypertrophy and failure
• Diabetes mellitus
• Renal disease
• Hyperlipidaemia.
Differentiation of the cause and aetiology are further elucidated on other presenting signs and symptoms and medical history. In a pulse diagnosis context, the parameter of pulse rate is used to identify aetiological factors of heat and cold affecting heart rhythm. This includes internal aetiologies arising from vacuities of Yin and Yang, and external pathogenic factors of heat and cold.
In CM terms, the Heart also governs the Mind or Shen. Physical heart damage will, theoretically, affect the clear expression of the Shen and be associated with Blood stagnation. The relationship is seen in the incidence of depression and heart disease. Severe shock or pain, anxiety and stress also affect the Shen, which in turn can affect heart rhythm.
The ability of the heart to contract rhythmically is due to both an intrinsic conduction system and extrinsic innervation of the autonomic nervous system, as noted in section 6.3.5. The sinoatrial (SA) node is the pacemaker of the heart, whose rhythm determines the heart rate. It initiates action potentials that spread throughout the heart muscle, causing it to contract in a coordinated manner (see section 6.3.5).
The pulse rhythm will be affected if cardiac function is impaired. Abnormal heart rhythm may be due to problems with the electrical conduction system through the heart, affecting both the rate of the pulse and the intervals between each pulsation. For example, ‘heart block’ refers to problems with the AV node, affecting the transmission of impulses to the ventricles from the atria. Although the ventricles have their own pacemaker, it is too slow to maintain sufficient circulation and arrhythmias may develop (Table 6.5). This is a chronic cause of arrhythmias. Transient functional irregularities, arising from stimulants and emotions can similarly affect heart rhythm (see section 6.5.5).
| Type of heart block | Effect on heart activity | Cause | Manual palpation |
|---|---|---|---|
| First degree | Atrial depolarisation becomes prolonged, there is a delay in the in normal conduction from atria to the ventricle but no ‘dropped beats’ | Local hypoxia, damage to heart conduction pathways, digitalis toxicity, Rheumatic fever, electrolyte imbalances such as hypo- or hyperkalaemia | No change to normal rhythm or rate |
| Second degree | Atrial depolarisation becomes prolonged or occasional loss of atrial depolarisation, and corresponding loss of ventricular depolarisation, i.e. ‘dropped beats’ | Problems with AV node, complications of endocarditis, hypokalemia, digoxin toxicity, coronary artery disease, myocardial infarction (MI), diabetes, antidys rhythmics, cyclic antidepressants | Interrupted rhythm. Occasional missed beat followed by larger beat-ectopic beats. Some transient variation in pulse force. Severity increases as HR increases |
| Third degree | Complete block of the normal signal in the heart: atrial depolarisation not coordinated with ventricular systole. Pacemaker cells in the ventricles take over but at a much slower rate | Hypokalaemia, myocardial infarction, problems with conduction pathway (bundle of His) | Decreased cardiac output, decreased (slow) heart rate 41–59 bpm, consistent decrease in pulse force. Electrocardiogram records the atrial contraction at 100 bpm and the ventricle at only 40 bpm |
6.5.4. Palpitations
Palpitations are defined as an abnormal awareness of the heart beating, which may be momentarily stronger, faster or irregular in rhythm (Box 6.8). Palpitations can be an indicator of interruption to normal heart rhythm, an arrhythmia, but not all palpitations are necessarily arrhythmic or cardiac related. For example, palpitations can be a prominent symptom in fever, hypoglycaemia or thyrotoxicosis (Lee 2001: p. 64).
Box 6.8
Clinical questions to ask your patient
• Are you aware of any palpitations?
• Is arrhythmia occurring on a regular basis (that is, is the patient aware that this is occurring or is this the first time that they’ve been made aware of this)?
• Is it old or new; if old, is it worsening in regards to duration and/ or frequency?
• How often is it occurring: daily, weekly, occasionally, no pattern to occurrence?
• What type of sensation does the subject experience?
• Previous history or family history of heart disease?
• Are the palpitations associated with stress, anxiety, exercise, fever, caffeine or nicotine intake, medication, alcohol or chocolate? Or do they occur at rest?
• What medication are you taking, including vitamin and herbal supplements?
• Do palpitations occur during the day or at night?
Additionally, always note the onset, duration, associated symptoms and circumstances in which arrhythmias/palpitations occur. Also ask the patient to tap out the rhythm of the arrhythmia or palpitations that they are feeling.
Palpitations are a subjective feeling that may occur as:
• The heart beating abnormally fast or irregularly
• The heart momentarily beating more forcefully than normal
• Ectopic beats (extra beats or extra systoles).
In CM, palpitations are normally associated with the Heart. They can occur in any pattern involving Heart disharmonies, whether physiological, psychological or emotionally based. This includes patterns ranging from vacuity patterns of Yin, Yang, Qi or Blood, to repletion patterns involving Heat or Phlegm. In addition to palpitations, pathology is further differentiated by:
• Additional changes in other pulse parameters.
Patients who report experiencing palpitations and have a psychiatric disorder are known to report longer-lasting periods of palpitations and ancillary symptoms than patients without a psychiatric disorder (Lee 2001: p. 64). In CM this is seen to be associated with conditions affecting clear expression of the Shen. The Shen or Mind resides in the Heart; disturbance of the Shen can disturb Heart function (Box 6.9).
Box 6.9
CM patterns associated with the occurrence of palpitations
CM Zang Fu patterns associated with palpitations usually involve the Heart:
• Heart Yin vacuity
• Heart blood vacuity
• Heart Yang vacuity
• Heart fire
• Phlegm heat misting the heart
• Heart blood stasis
6.5.4.1. Ectopic beats
Ectopic beats are a premature contraction of the heart due to an impulse generated outside the SA node or abnormally generated by the SA node, interrupting the normal cardiac rhythm. They can occur regularly or irregularly.
Ectopic beats can be relatively benign and occur in healthy individuals with no apparent cause. They also occur when the heart is excessively irritated through either metabolic or chemical stimulus (see section 6.5.5 for further details).
6.5.4.2. Ectopic beats — pulse presentation
Because the heart contracts prematurely there is incomplete filling of the left ventricle, resulting in less blood volume being ejected than would normally occur if the left ventricle had completely filled (Box 6.10). Consequently a pulse wave arising from an ectopic beat is felt weaker or absent than other pulsations, sometimes mistaken for a ‘missed beat’ (Guyton & Hall 2006).
Box 6.10
Flutters and fibrillations
Fibrillations and flutters occur when segments of the heart contract far more than normal. Because the contraction is associated with only a certain area of the heart, or because the contraction is not complete, this is a situation in which the pulse rate will not correlate with what’s occurring in the heart. Instead there will be changes in other pulse parameters such as pulse force which is decreased, reflecting incomplete filling of blood in the ventricles and subsequent volume of blood ejected into circulation.
• Atrial flutter: Rapid atrial contractions (240–360 bpm) occur in conjunction with 2nd degree atrioventricular (AV) block resulting in some missing beats due to the electrical impulses not always reaching the ventricles.
• Atrial fibrillation: Asynchronous contraction of atrial muscle fibres, leading to cessation of atrial contraction. Regardless, blood can still flow from the atria into the ventricles, so cardiac output continues but is decreased by 20–30 percent. This can occur for a number of reasons such as myocardial infarction, hyperthyroidism or rheumatic heart disease (Tortora & Grabowski 1996).
• Ventricular fibrillation: Associated with heart rate of >300 bpm, as different areas of the ventricles are stimulated. The ventricles do not contract properly, which quickly leads to unconsciousness and likely death if the fibrillation is not stopped within 2–3 minutes (Information from Guyton & Hall 2006: pp. 152-6).
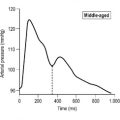
Following an ectopic beat, there is a compensatory pause or a longer interval before the heart contracts again. This can result in a stronger pulse beat because there is an increased filling of the left ventricle; a greater volume of blood is expelled into circulation when ventricular contraction next occurs (Fig. 6.3).
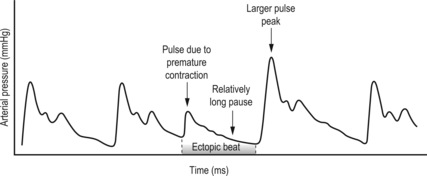 |
| Figure 6.3Schematic of the variation in pulse amplitude and regular rhythm as occurs with an ectopic beat. |
On a more serious note, ectopic beats may indicate some type of metabolic damage leading to excessive irritability of the heart muscle. This can occur as a result of viral or bacterial infection affecting the heart such as rheumatic fever, or may result from damage due to myocardial infarction (Epstein et al 1992: p. 7.30).
6.5.5. Pulse rhythm: Clinical perspective
Arrhythmias, palpitations and ectopic beats can be signs of a serious heart condition involving the conduction system in the heart; Heart Qi and Yang maybe seriously impaired (Box 6.11).
Box 6.11
Arrhythmia: summary
• Palpitation: A subjective abnormal awareness of heart beating, reported by the patient
• Arrhythmia: A general term to describe any irregularity in the heart rhythm, also called dysrhythmia
• Arrhythmias range in severity from occasional missed beats (which may be normal in the absence of any other symptoms), to changes in speed (rapid beats), extra beats (ectopic), to extremely irregular with no rhythm (e.g. atrial fibrillation — 240–360 bpm)
• From a CM perspective, arrhythmias are associated with primary exhaustion of heart Qi, Yin or Yang in nature. This has secondary effects on circulation
• From a biomedical perspective, arrhythmias are due to abnormal rate of impulse generation or the abnormal conduction of impulses
• Possible causes of arrhythmias include stress, anxiety, exercise, fever, caffeine or nicotine intake, medication and herbs, alcohol, chocolate, hyperthyroidism, potassium deficiency and certain heart diseases.
The presence of arrhythmia is seen as part of a pathological process; however, the regularity of interruptions to normal heart rhythm can indicate the severity of the process. The increasing regularity of missed beats indicates a worsening of the condition, and a decreasing occurrence of missing beats indicates a continuing resolution of the condition. The timing of the commencement of missed beats also has prognostic value. If they start with the onset of a new illness then the prognosis is better than if arrhythmia occurs during a chronic or critical disease.
The same factors that affect heart rate may also cause arrhythmias, palpitations and ectopic beats, including:
• Excessive intake of stimulants such as nicotine, coffee and other beverages containing caffeine
• Alcohol
• Acute periods of stress, tension, anxiety and panic attacks
• Hypoxia (resulting in less oxygen supply to the body)
• Lack of sleep
• Increased basal body temperature (Prolonged increase in the basal body temperature eventually weakens the heart)
• Medications such as epinephrine, ephedrine, aminophylline, and atropine which are responsible for palpitations (Lee 2001: p. 65)
• Toxic reactions to some drugs and herbs which have cardiostimulatory affects and can cause palpitations and arrhythmias
6.6.1. Skipping pulse (Cù mài)

6.6.1.1. Alternative names
Hasty, Abrupt, Hurried, Running, Agitated, Accelerated or Rapidly Irregularly Interrupted pulse.
6.6.1.2. Requisite parameters
The Skipping pulse is a simple pulse quality with changes in two pulse parameters:
• Rhythm: The Skipping pulse has irregular pauses in heart rhythm
• Rate: The pulse rate is greater than normal (>90 bpm).
6.6.1.3. Clinical definition
The Skipping pulse has irregular pauses or interruptions in normal heart rhythm, accompanied by a pulse rate of more than 90 bpm (Box 6.12). The pauses or interruptions may occur with any interval of pulse beats. However, the more often (that is, closer together) they occur, the more severe the condition.
Box 6.12
Irregular pauses without changes in pulse rate
Irregular pauses in the rhythm occur in healthy people without changes in the rate. This is often seen in individuals with high levels of tensions/stress. In these situations the irregular pauses are transient and often resolve when the stressor has been removed. From a CM perspective, irregular pauses accompanying stress or anxiety are often associated with a stagnation of the Liver’s physiological function of maintaining the free flow of Qi and Blood.
6.6.1.4. Classical description from the Mai Jing
The skipping pulse is a pulse coming and going rapidly with occasional interruptions but having the ability to recover
6.6.1.5. CM Indications
The Skipping pulse always indicates disharmony involving heat-related conditions affecting the maintainence of the regular rhythm by Heart Qi, or Heart dysfunction.
There are three main CM patterns associated with the formation of the Skipping pulse:
Internal heat
Internal heat from EPAs producing fever agitate Qi and blood, supplementing Yang Qi and increasing pulse rate. The heat agitation of the Qi and blood also obstructs the smooth flow of these to the heart. The heart function becomes arrhythmic. Prolonged incidence of internal heat may give rise to consumption of Yin fluids and weaken the Heart Qi (see below).
Consumption of Yin fluids
With internal heat, over time this may be complicated by the consumption of Yin fluids — the fluids are consumed and thus cannot flow continuously. This situation is associated with febrile conditions such as rheumatic fever, consumed Yin resulting in heart damage. An increase in heart rate caused by heat, if prolonged, eventually exhausts the heart and arrhythmias can result.
Exhausted heart Qi and blood
The pulse is usually seen in critical diseases such as organic heart disease that is due to exhausted Heart Qi and Blood. This can arise as a complication of internal heat and Yin fluid consumption. The pattern refers primarily to the heart’s inability to maintain a rhythmic contraction required for appropriate circulation, or is representative of the body’s attempt to maintain circulatory integrity of blood and fluids when it is no longer capable of doing so. Prognosis is poor, and indicates end-stage aetiology involving heart failure.
6.6.1.6. Biomedical perspective
The Skipping pulse may be associated with:
• Hyperthyroidism (thyrotoxicosis)
• Heart valve problems (damage from rheumatic fever)
• Hypertension.
6.6.2. Bound pulse (Jié mài)

6.6.2.1. Alternative names
Knotted, Nodular, Adherent or Hesitant pulse.
6.6.2.2. Requisite parameters
The Bound pulse is a simple pulse quality with changes in two pulse parameters:
• Rhythm: There are irregular pauses in heart rhythm resulting in varying intervals between subsequent beats.
• Rate: The pulse rate is less than normal (<60 bpm).
6.6.2.3. Clinical definition
The Bound pulse has irregular pauses in heart rhythm accompanied by a pulse rate of less than 60 bpm.
6.6.2.4. Classical description from the Mai Jing
The bound pulse is a pulse slow in coming and going with occasional interruption but the ability to recover
6.6.2.5. CM indications
The Bound pulse always indicates pathogenesis involving the Heart. Three patterns are associated with the Bound pulse:
• Pathogenic Cold obstructing the smooth flow of Qi and blood to the heart
• Obstruction of Qi and Blood
• Yang vacuity and Vital (Yuan) Qi vacuity.
Pathogenic cold
The Bound pulse as a result of pathogenic Cold is probably a relatively acute onset associated with exposure of the previously healthy individual to environmental Cold. This is described as a Cold pathogen invasion. In a biomedical context this is termed hypothermia. The description of the pulse type in the classical literature was probably a direct reflection of the environmental conditions in the Chinese winter, and thus a relatively common presentation in traditional clinical practice in China. Hypothermia is still a relatively common occurrence at high latitudes, with children and the elderly particularly susceptible.
Physiological changes occurring with hypothermia depend on the severity of exposure to cold and also on the individual’s core body temperature. In terms of the Bound pulse, arrhythmic changes occur when the core body temperature decreases to 32.2–28 °C (or 90–82.4 °F) (Danzl 2001: p. 108). This is considered moderate hypothermia.
Moderate hypothermia is associated with both atrial and ventricular arrhythmias. Additionally, the decrease in body temperature causes decreased contractility of the cardiac muscles, so there are accompanying changes in the strength of cardiac output as well as decreases in heart rate. In a CM context this is the Cold’s constraining effect on the Heart Qi and Yang, associated with secondary obstructions in the normal Qi and blood flow in the vessels.
Obstruction of Qi and Blood
A number of authors (Lu 1996, Deng 1999, Guangzhou College notes 1991) note that the Bound pulse may be associated with phlegm, food retention or masses (concretions). These pathogenic factors impede both Qi and blood circulation. In these cases the pulse would also be forceful, however there may also be additional parameter changes. For example, in phlegm conditions the pulse may also have a rounded contour (the Slippery pulse).
Yang vacuity and vital (Yuan) Qi vacuity
The Bound pulse may also arise due to the vacuity of Yang Qi, which can be the result of constitutional factors or damage caused by lifestyle, emotional disturbance or dietary habits. As noted by Lyttleton (2004: p. 17) an invasion of pathogenic Cold (albeit a milder form than the hypothermia described above) may happen readily in the Western lifestyle, via the ingestion of overly cold foods and drinks or excessive consumption of raw food, living or working in a cold damp environment or as a result of overwork and insufficient sleep. Although this may not cause significant problems in the short term, prolonged damage to Yang will have inevitable effects on the normal functioning of the organs. In particular, the heart’s ability to contract sufficiently is affected by Heart Yang Qi vacuity, so heart contraction is weak. This results in a pulsation that is forceless.
The significance of the Bound pulse occurring with Cold is not in diagnosing Cold as a causal agent but rather that the body’s Qi and Yang were weak to have allowed Cold penetration in the first instance, and in particular, for it to have affected the heart function at all. Irrespective of the cause, there are a considerable number of processes involved in the underlying pathogenesis in the formation of this pulse. Lifestyle, genetic and dietary factors all predicate towards the formation of the pulse once the appropriate causal agent activates the triggers. As such, although the pulse can present in an acute situation, it is nearly always preceded by other aetiologies.
6.6.2.6. Biomedical perspective
The Bound pulse may indicate problems with normal heart function such as pacemaker dysfunction, for example second- and/or third-degree heart block or more seriously, it may indicate heart failure (see Table 6.5).
6.6.3. Intermittent pulse (Dài mài)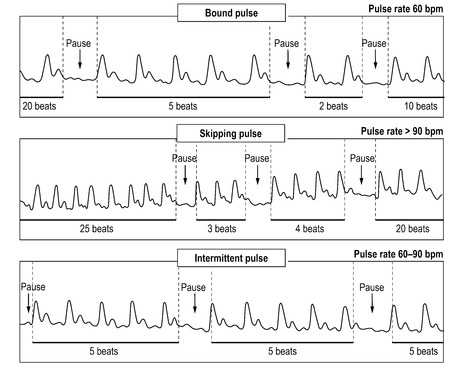
6.6.3.1. Alternative names
Regularly interrupted, Replacement or Changing pulse.
6.6.3.2. Requisite parameters
The Intermittent pulse is a simple pulse quality defined solely by pulse rhythm: there are regular pauses in the heart rhythm.
6.6.3.3. Clinical definition
The Intermittent pulse has an interruption to heart rhythm occurring at regular intervals. This may occur every few beats (indicating a more severe illness) or less frequently. There is no accompanying change in heart rate from normal (60–90 bpm)
6.6.3.4. Classical description from the Mai Jing
The interrupted pulse is a pulse with regular interruption and inability to recover itself, resuming to beat (only after a long pause). The bound pulse is prognosticative of survival but the interrupted one of death.
6.6.3.5. CM indications
The Intermittent pulse is almost always a sign of pathogenesis, usually involving the heart and other vital organs. A footnote in The Lakeside Master’s Study of the Pulse (Li, Flaws (trans) 1998: pp. 122-123) states that this pulse is associated with serious heart disease. How frequently the interruptions occur is used to indicate the relative severity of the condition. The more often pauses occur with the Intermittent pulse, the more severe the condition.
An Intermittent pulse can occur in individuals without accompaniment of other apparent signs and symptoms. In such cases, the regular interruptions to rhythm are probably more widely spaced (Table 6.6).
| Specific CM pulse quality | Rhythm | Heart rate |
|---|---|---|
| Bound | Irregular: occasional irregular interruption to rhythm | Slow: ≤60 bpm |
| Skipping | Irregular: occasional irregular interruption to rhythm | Rapid: ≥90 bpm |
| Intermittent | Regular interruption: a interruption to rhythm between a consistent number of beats | Normal: 60–90 bpm |
 |
||
Three patterns are associated with the Intermittent pulse:
This is a primary pattern specifically relating to the Heart and its physiological function. It may be associated with congenital defects in the heart’s conduction system or organic disease of the heart muscle such as dystrophies, or may develop as a result of damage associated with fevers and infarction.
Severe vacuity of essential substances
The Intermittent pulse occurs in response to vacuity of Yuan Qi and Jing Qi. This is a pattern with systemic origins rather than originating solely from the heart, even though the heart is eventually affected. For example, Yuan Qi and Jing Qi are essential components in the production of Qi and blood, therefore affecting the supply of both Qi and blood to the organs.
In a sick person the Intermittent pulse is considered serious but can be treated. The logic being that since the person is already sick then an arrhythmic pulse is a ‘natural’ progression of prolonged illness consuming Yuan Qi and Jing Qi and so affecting visceral Qi.
Pain
The traditional pulse literature lists this pulse occurring in conditions of severe pain, usually the result of obstruction of blood and Qi, thus affecting circulation. In light of the involvement of the heart in the formation of this pulse, severe pain may incorporate angina as a related cause.
6.6.3.6. Biomedical perspective
The Intermittent pulse usually occurs as a result of heart disease, severe pain or severe traumatic injury. If it occurs in the elderly or develops during chronic disease, it is viewed as a critical situation. From a CM perspective this would be viewed as a severe depletion of Heart Qi.
6.7. Depth
The parameter of depth is a simple pulse parameter used to indicate the level of depth at which the pulse is felt as being the strongest. Three levels of depth are used in the Cun Kou system of pulse palpation, each found by using incremental pressure applied to the radial artery by the palpating fingertips. (See Chapter 5 for further information on technique used for finding and assessing the levels of depth.) The three levels of depth are termed the superficial, middle and deep levels of depth.
A great proportion of the traditional 27 pulse qualities are felt strongest at one of the three levels of depth and so are defined as either superficial, middle or deep level of depth pulses (Fig. 6.4, Box 6.13). For example, several CM pulse types are located at the superficial level of depth (which can be felt by resting the fingers on the skin) or are palpated most forcefully at the superficial level of depth. These may be classified as superficial pulses, so this is defining the pulse by its level of depth (Box 6.14).
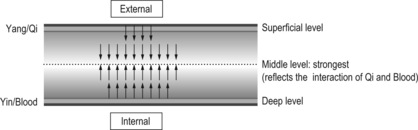 |
| Figure 6.4Diagrammatic representation of a healthy pulse and the relative pulse strength at the three levels of depth. The middle level of depth should be strongest, representing the interaction of Qi and Blood. |
Box 6.13
Normal pulse strength with level of depth
• Superficial level of depth: Often felt as the least strongest in healthy individuals
• Middle level of depth: Often has the most pulse strength
• Deep level of depth: Equal to or slightly less strong than middle level of depth
Box 6.14
Revision of assessment technique for determining pulse depth
• Superficial pulse depth: Found by resting the fingertips lightly on the skin surface without pressure. Superficial level is not the depth at which the pulse is first felt.
• Deep pulse depth: Found by occluding the radial artery (pressing firmly on the artery against the radial bone) and then releasing the pressure gently and slowly until the pulse can be felt again. This pressure should be maintained. This release of pressure creates an initial rush in blood flow; therefore a few seconds should be allowed to enable the pulse to equalise before assessing it.
• Middle pulse depth: Found by applying a moderate pressure to the radial artery (not sufficient to occlude it); somewhere between superficial and deep. The middle depth is examined after palpating the superficial and deep levels to determine the pressure required to reach each level of depth.
The Floating pulse is one such pulse that is commonly defined as a superficial pulse (but it should be noted that not all superficial pulses are classified as Floating). Similarly, there are several CM pulses that can be felt only with heavy pressure, or are felt strongest at the deep level of depth and are consequently termed deep pulses.
There are three simple CM pulse qualities that are solely defined by the parameter of depth alone:
There are other CM pulse qualities that can also be felt strongest at the superficial or deep levels of depth; however, they are accompanied by changes in other pulse parameters and may be more appropriately defined by that pulse parameter. For this reason, pulses found at a particular level of depth are listed in other pulse parameter sections relating to their most defining rubric, and are not listed here under the depth parameter.
6.7.1. Pulse depth and its assessment
As discussed in section 5.6 (locating the pulse depth), the parameter of pulse depth may be interpreted in two ways:
• The level of depth where the radial arterial pulsation is found to be the strongest, regardless of the overall intensity of the pulsation (that is, assessing relative strength)
• The level of depth at which the radial artery is physically located.
Assessing the level of depth requires palpation at each of the three levels of depth and judging at which level of depth the pulse wave is felt most strongly or most distinctly. Sometimes the pulse can only be felt at one level of depth and so defining the pulse by the level of depth is easy. At other times the pulse is felt at more than one level of depth and the practitioner needs to make a decision about the level of depth where it is strongest. Alternatively, the pulse may be felt equally strongly at all three levels of depth, and this is diagnostically relevant too: this is the Replete pulse, which is discussed in section 7.7.1.
Diagnostically, the level of depth may be affected by pathological processes occurring within the body, resulting in either a pulse that can be felt strongest at the superficial or deep level of depth, or perhaps equally strong at all three levels of depth. Other factors affecting where the pulse can be felt include the strength of cardiac contraction (see pulse force, section 7.6). Pathological processes may also result in anatomical structural variations and so vary the perceived level of depth. This arises when there are physiological changes in the subcutaneous layer of tissue overlying the radial artery, or anatomical variations in the musculature and tendinous insertions around the forearm and wrist area. This causes the actual arterial structure to ‘sink’ or ‘float’, altering the level of pulse depth as well.
6.7.2. The normal pulse depth
In order to determine whether the pulse is felt pathologically relatively stronger or weaker at a specific level of depth, it is first necessary to know what the ‘expected’ relative strength of each level of depth should be.
Generally, the radial arterial pulse should be palpable at all the three levels of depth. However, the strength of the pulse at each of the three levels of depth may differ. In terms of relative strength, the pulse will usually be less palpable at the superficial level of depth and most forceful in the middle level of depth. At the deep level of depth, the pulse should be either equally forceful or slightly less forceful than the middle level of depth. This is what would be expected for a healthy pulse. From a CM perspective, as the pulse is formed by the interaction of both Yang (external, movement, function) and Yin (internal, Blood, form), the balance of these two dynamic forces results in a pulse that should be palpable at all levels of depth but felt with most strength in the middle level of depth.
Changes in strength at individual levels of depth are used to identify pathology and provide information about the location of disease and functional status of Yin and Yang . When describing the level of depth with regard to a specific pulse we are talking about the level of depth at which the pulse is felt relatively strongest (meaning that it may still be felt at other levels of depth but it is not as strong.)
6.7.2.1. Physiological response of the circulatory system to climate – when changes in the normal level of depth are appropriate
According to the CM classical pulse literature, seasonal effects impact on the presentation of the pulse in many aspects (see section 5.12.2). With regard to pulse depth, the classical literature notes the level of depth where the pulse is felt strongest varies depending on the season. For example, in summer the pulse is described as more superficial, and in winter the pulse is deeper. The change in the level of depth where the pulse is felt strongest is explained with respect to the body’s Qi, retreating in winter and expanding in summer. This is alternatively viewed as the body’s attempt to maintain a stable core body temperature, varying the degree of exposure the blood vessels have to the environment and so mediating the retention or loss of body heat (Fig. 6.5).
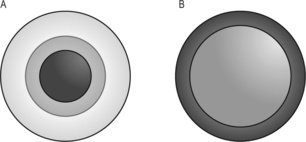 |
| Figure 6.5(a) Cold is associated with cutaneous vasoconstriction and normal or increased blood flow to many organs. The white area represents the skin, which serves as a shell of insulation because it receives almost no flow. The darkest regions (the body core) have the highest blood flows and the stippled regions (e.g. muscle) receive relatively low flows. (b) Hot conditions cause high surface (cutaneous) blood flow (dark region), causing loss of thermal insulation and reduced flow to the body core (stippled region) so that less heat is stored centrally and thermal insulation is lost (no white regions).(After Fig. 5.1 in Rowell LB 1986, Human circulation regulation during physical stress, with permission of Oxofrd University Press.) |
In a clinical context, a deeper located pulse in winter or a more superficial pulse in summer is then viewed as an appropriate response of the body to climatic influences and not necessarily always related to pathology.
6.7.3. Levels of depth and their meaning: CM perspective
The level of depth of the pulse may provide information about:
• Location of disease
• Quality and quantity of Qi, particularly Yang, and its ability to move outwards
• Integrity of Yin and its ability to balance and anchor Yang.
6.7.3.1. Pulse depth and location of disease
In the Mai Jing (Wang, Yang (trans) 1997: p. 26) Wang noted that ‘a floating pulse is ascribed to the exterior, and a sinking one to the interior’. If the pulse is felt relatively strongest at the superficial level of depth, this generally indicates an external condition or a condition that has affected the superficial layers of the body such as the skin, muscles and channel systems. A pulse strongest at the superficial level of depth may also refer to disharmony affecting the Yang organs that are theoretically assigned to the superficial level of depth.
A pulse that is felt relatively strongest at the deep level of depth is usually related to an internal disorder, affecting the interior of the body or the Yin organs. For example, a pulse that can be felt forcefully at the deep level of depth may indicate obstruction or stagnation of Qi and blood. In this situation the pulse cannot be felt at the superficial level of depth because Yang is being obstructed in the interior of the body, unable to move outwards towards the exterior of the body and so the pulse remains in the deep levels of depth (Box 6.15).
Box 6.15
Levels of depth and diagnosis
A specific example of the use of level of depth as a diagnostic tool is the theory of the Eight Principles. The Eight Principles are a foundational framework that is used in diagnosis to determine the location and nature of a disharmony or illness. This thereby assists in formulating a treatment plan (Maciocia 1989: p. 179). There are a myriad of different pattern identification methods, but they are all based on the Eight Principles: Internal, External, Replete, Vacuity, Hot, Cold, Yin and Yang. From this perspective, the level of depth at which the pulse can be felt the strongest informs us simply about the location of disease.
6.7.3.2. Yang Qi
The superficial level of depth of the radial pulse represents the exterior or the Yang aspect of the body. In this respect, the superficial level of the pulse also represents the quality of Qi, in particular Yang. Where the pulse can be palpated may also inform us about the capacity of Yang Qi to motivate the pulse and lift it to a palpable depth. If Yang is vacuous (deficient) this can result in a deeply located pulse, with Yang insufficient to raise the pulse to the surface. Parameters such as pulse force and rate may provide additional information about the quality of Yang. For example, when Yang Qi becomes vacuous, it would be expected that the pulse would present without strength, possibly with a slow rate and an increase in relative strength at the deep level of depth.
If the pulse is strongest at the superficial level of depth, this may indicate that Yang is more active than normal. This may occur when an external pathogenic agent (EPA) such as Wind, Heat, Cold or Damp enters the body and lodges in the skin and muscle layers. In response to this invasion, Wei Qi (the body’s defensive Qi) rushes to the body’s surface to fight this EPA. This is reflected in the radial pulse as a relative increase in strength at the superficial (external) level of depth. (Wei Qi is considered to be the relatively Yang manifestation of Zhen Qi (True Qi) or meridian Qi, circulating outside the channels on the exterior of the body, protecting and warming the body. Ying Qi (Nutritive Qi) is the Yin manifestation of Zhen Qi, circulating in the blood vessels, channels and internal organs.)
Excess Yang, in the form of Heat, which may arise internally or externally, may lead to the pulse being palpated forcefully at the superficial level of depth as occurs with the formation of the Surging pulse (along with notable changes in the pulse contour, force and width. The Surging pulse is discussed in more detail in section 7.9.3.)
6.7.3.3. Yin
In terms of pulse depth, the quality of Yin energy is symbolised by the deep level of depth. Yin has the effect of cooling and nourishing the body. It encompasses the numerous fluids that circulate around the body such as Blood, Body Fluids (Jin-Ye) and Essence (Jing). It also plays a role in helping to control and balance Yang; this is the ‘functional Yin’. If Yin and its various aspects become vacuous, then Yang becomes relatively hyperactive. This results in the pulse being felt relatively stronger at the superficial level of depth because the Yin is no longer able to restrain Yang, so Yang moves outward to the exterior of the body.
Yin vacuity also affects other pulse parameters such as pulse force, width and rate, resulting in a pulse that is decreased in strength and arterial width but with an increase in pulse rate (dependent upon the strength of the deficient heat produced).
Conversely, excessive Yin in the form of pathogenic Cold or Damp (Yin pathogenic factors) may attack the body from the exterior and enter via the skin, muscles and channels or move directly into the interior of the body via certain internal organs such as the stomach, intestines or uterus. In the former case, the pulse would be felt strongest at the superficial level of depth, and in the latter example, the pulse would be strongest at the deep level of depth.
Internal Cold (also Yin in nature) may develop from qi causes such as deficiency of Yang affecting the Yin organs, notably the Spleen, Lung, Kidneys and Heart. This may develop as a consequence of a weak constitution, chronic illness, hypo-functioning metabolism or inappropriate diet. The pulse would be felt relatively stronger at the deep level of depth, indicating both an internal condition and the involvement of the Yin organs.
6.7.4. Levels of depth and their meaning: biomedical perspective
The ease with which the radial artery can be palpated may be affected by the person’s constitutional body type. For example, a slim person’s radial artery may be more easily accessible because of the thinner layer of subcutaneous tissue, while someone with a higher proportion of body fat may have an artery that is more difficult to palpate because of the thicker subcutaneous tissue layer. Alternatively, difficulty palpating the pulse may also be due to a pathological process occurring in the body. For example, oedema or accumulation of fluids in the connective tissue layer (in the interstitial spaces between cells and outside the blood vessels) may affect the ease with which the radial artery can be palpated.
Arterial blood pressure and the strength of cardiac contraction equally influence the level of depth at which the pulse is felt strongest. An increase in volume in the pulse is described as ‘full and bounding’ while a decrease in volume is described as ‘weak and thready’ (Funnell et al 2005: p. 267). Full bounding pulses are associated with strong cardiac contraction and are felt more readily at the superficial levels of depth where weak thready pulses may be hard to discern.
6.8. CM pulse qualities defined by level of depth
6.8.1. Floating pulse (Fú mài)

6.8.1.1. Requisite parameters
The Floating pulse is a simple pulse quality defined solely by pulse depth. It is felt most forcefully at the superficial level of depth, with fingers resting lightly on the skin, exerting no pressure except the weight of the fingers.
6.8.1.2. Clinical definition
The Floating pulse is felt relatively strongest at the superficial level of depth, compared to the other levels of depth. With increasing finger pressure there is a decrease of force, the pulsation cannot be felt at the depth deep level of depth. In order to identify the Floating pulse, each level of depth must be examined and the relative strength of each level determined.
6.8.1.3. Identifying whether the Floating pulse is present
Step 1: When the fingers are placed over the radial artery pulsation with only the pressure of the resting fingers exerting pressure, the pulse may be easily palpated (Fig. 6.6).
Step 2: With increasing finger pressure exerted over the radial pulsation, there is a resulting decrease in the pulse force. With increasing finger pressure the pulsation disappears and the pulse at the deep level of depth cannot be felt.
The term ‘floating’ is also used as a general descriptor of any pulse type that can be palpated strongest at the superficial level (the level at which the fingers rest gently on the artery without pressure), regardless of changes in other parameters. This should not be confused with the Floating pulse, a distinct CM pulse quality. Describing a pulse as being felt strongest superficially or at the superficial level of depth should help to prevent such terminological confusion.
6.8.1.4. Classical description from the Shang Han Lun and Mai Jing
A pulse that is felt when light pressure is applied is called ‘Floating’ (Shang Han Lun) (Mitchell et al 1999: p. 34).
The floating pulse is a pulse potent when felt with no pressure applied but impotent when felt with pressure applied
6.8.1.5. CM indications
The Floating pulse is always considered to be indicative of pathogenesis (Box 6.16). There are two primary patterns where the Floating pulse may occur:
• Replete condition, indicating an external pathogenic agent (EPA)
• Vacuous condition, involving vacuity of Yin fluids causing Yang to ‘float’.
Box 6.16
Summary of the Floating pulse
• Floating and forceful = Replete condition externally: EPA
• Floating and forceless = Vacuous condition internally: Vacuity of Yin fluids
• Floating, forceless and narrow arterial diameter: Severe vacuity of Yin → Soggy pulse
• Floating, forceless and wide arterial diameter: Qi and Blood vacuity → Vacuous pulse
They are differentiated by changes in the pulse parameter of force, accompanying signs and symptoms and whether the disharmony is an acute or chronic condition.
The Floating pulse is relatively strongest at the superficial level, with an accompanying increase in the parameter of pulse force. The EPA may take the form of a Yin or Yang type pathogenic factor such as Wind, Heat, Cold or Damp. This pattern could be further differentiated by the accompanying changes in pulse rate or arterial wall tension. For example, an EPA of Heat may also cause an increase in pulse rate, or an EPA of Cold may slow the pulse rate and increase arterial wall tension. In this scenario, the formation of the Floating pulse may be accompanied by a Rapid pulse or Slow pulse (if the rate changes were great enough). Additional signs and symptoms such as body aches, fever, aversion to cold and sudden onset of illness further differentiate the pathogen type.
Mechanism
The EPA enters the body via the skin, nose, and mouth and Wei Qi (defensive Qi), which usually circulates through the skin and muscles to defend the body, rushes to the exterior of the body to fight off the pathogen. Where the Qi goes blood goes. Therefore, the pulse can be felt strongest at the superficial level of depth, reflecting the location of the pathogen. If the Floating pulse also presents with increased pulse force, this signifies the ability of the healthy immune system (also known as the Zheng Qi or Upright Qi in CM terms) to respond strongly to the pathogenic factor.
Clinical relevance
From a clinical perspective, the formation of the Floating pulse in response to an EPA would be associated with the rapid onset of an acute condition such as a cold or flu-type viral infection. Other signs and symptoms such as fever, sore throat, sweating, headache and quesion to cold may accompany this pulse depending upon the nature of the EPA.
Exception
The Floating pulse when forceful may not occur in someone who has an underlying vacuity condition (such as a compromised immune system or chronic illness) as their Wei Qi or Zheng Qi is too deficient to respond strongly to the pathogenic factor. Therefore the Floating pulse may still occur, being relatively stronger at the superficial level, but it may not be accompanied by an increase in pulse force.
Vacuous condition involving vacuity of Yin fluids
In this pattern the formation of the Floating pulse would be accompanied by changes in other parameters such as pulse force. In this case, the Floating pulse is forceless, reflecting the underlying vacuity. This pulse quality may appear as a result of internal disease, manifesting as a vacuity of Yin substances. This may take the form of deficiency of Yin, blood or body fluids. It is the accompanying signs and symptoms that further define the disharmony.
• Mechanism: This pulse is formed when the insufficient Yin is unable to control and anchor the relatively excessive Yang, whose natural inclination is to move outward. Therefore, Yang rises to the surface, resulting in a pulse that is felt strongest at the superficial level of depth. However, because Yin is deficient the pulse is lacking in force and decreases significantly in strength as finger pressure is exerted on the artery.
• Clinical relevance: This may be the result of the consumption of Yin due to lifestyle issues such as overwork, irregular eating patterns and insufficient sleep. The loss of body fluids due to excessive sweating or vomiting may also result in the formation of this pulse type.
6.8.1.6. Further differentiation of the Floating pulse
As noted, the Floating pulse can be further differentiated on the basis of changes in parameters other than level of depth. The parameter of pulse force provides information about whether the Floating pulse is caused by repletion or vacuity. Similarly, changes in pulse width can inform us about the condition of Yin and blood or the hyperactivity or relative hyperactivity of Yang (Lu 1996: p. 33). It is the combination of changes in other pulse parameters, in addition to a pulse that feels strongest at the superficial level of depth, which results in the formation of other CM pulse qualities. For example:
• A forceless, superficial and narrow pulse indicates Yin vacuity: this becomes known as the Soggy pulse rather than the Floating pulse. (The difference is that the Soggy pulse is only felt at the superficial region while the Floating pulse has decreasing levels of strength with increasing finger pressure; that is, it can still be felt in the middle level but not as strongly as the superficial level.)
• A forceless, superficial and wide pulse indicates both Qi and blood vacuity: this then becomes termed the Vacuous pulse.
6.8.2. Sinking pulse (Chén mài)

6.8.2.1. Alternative names
Sunken, Deep or Submerged pulse.
6.8.2.2. Requisite parameters
The Sinking pulse is a simple pulse quality with a change in the pulse parameter of depth. It is felt relatively strongest at the deep level of depth.
6.8.2.3. Clinical definition
The Sinking pulse can be felt relatively strongest at the deep level of depth. With increasing finger pressure over the radial pulsation, there is an increase in pulse force as the deep level of depth is approached (Fig. 6.7). The formation of the Sinking pulse means that the arterial pulsation cannot be felt at the superficial level of depth, but may be felt slightly at the middle level of depth. It is strongest and clearest at the deep level of depth. (The Sinking pulse is considered to be opposite to the Floating pulse. This is based on the depth parameter and their relative opposite locations according to the levels of depth.)
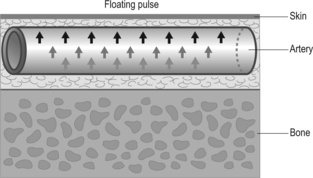 |
| Figure 6.6Floating pulse and relative strength differences within the arterial pulsation relative to pressure applied by the fingers. The pulse wave is felt strongest at the superficial region. The strength of the pressure wave is symbolised by arrows. Note the arrows lessen at the deeper levels of depth reflecting the relative decrease in strength. |
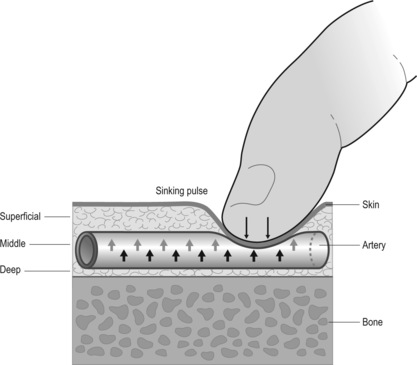 |
| Figure 6.7Sinking pulse and relative strength differences within the arterial pulsation relative to pressure applied by the fingers. The pulse wave is felt strongest at the deep region. The strength of the pressure wave is symbolised by arrows moving up while the pressure of the finger pressure is symbolised by arrows moving in. |
6.8.2.4. Identifying whether the Sinking pulse is present
Step 1: The pulse is best identified by first placing the fingers gently on the skin overlying the radial artery, with only the weight of the palpating fingers exerting downward pressure. At this superficial level of depth, the radial pulsation cannot be felt.
Step 2: The deep level of the pulse is next examined by increasing finger pressure so that the radial artery is occluded for a few seconds and then the finger pressure is slightly eased so that the pulsation can once again be felt. The radial pulsation will appear at its strongest at this level of depth.
Step 3: Once the deep level of the pulse has been located, the middle level of the pulse should then be assessed. The radial pulsation may be able to be palpated at the middle level of depth but will be felt with less intensity than the pulsation felt at the deep level of depth.
Once the three levels of depth are located, the fingers can be gradually moved from the superficial level of depth to the deep level of depth. In doing this the radial pulsation will sequentially increase in relative strength as the fingers move deeper into each level of depth.
A deep pulse is where one must press all the way to the bone to find it (Su Wen)
The deep pulse is a pulse impotent when felt with no pressure applied but potent when felt with pressure applied [said in another version to be absent unless heavy pressure is applied] (Mai Jing)
(Wang, Yang (trans): p. 3).
6.8.2.6. CM indications
Pulse depth provides information pertaining to where disease is located, differentiated further by additional changes in other pulse parameters. The Nei Jing says ‘when there is an imbalance in the body’s interior, one should examine the pulse at the deepest level’. In this sense, the Sinking pulse indicates disharmony in the interior. We have already noted that pulse depth provides information about Yang Qi, characterised by the superficial level of depth. Therefore, if a pulse cannot be palpated at the superficial level it may suggest that either Yang Qi is deficient or that disharmony is occurring internally. The Sinking pulse is always indicative of pathogenesis (Box 6.17).
Box 6.17
Summary of Sinking pulses
• Sinking and forceful: Internal pathogenic factor or obstruction of Qi and blood
• Sinking and forceless: Vacuity of Qi and blood, especially Yang
The Sinking pulse can indicate two primary patterns that are further differentiated by changes in the parameter of pulse force:
• Internal replete condition
• Internal vacuous condition.
Internal replete condition
The Sinking pulse due to repletion (excess) in the interior will be forceful at the deep level of depth. It indicates the presence of a pathogenic factor such as Cold, Heat, Damp or Phlegm depending on the accompanying signs and symptoms. In these cases, changes in other pulse parameters may be apparent. For example, the pulse rate may be slow in the presence of Cold or rapid in the case of Heat.
The Sinking and forceful pulse may also imply the obstruction of Qi and blood. This may result from the aforementioned pathogenic factors or from retention of food (Lu 1996). The pulse presents forcefully and would be accompanied by some type of pain. (Pain is symptomatic of obstruction, irrespective of the cause of the obstruction.) Pain often results in an increase in arterial tension (another of the pulse parameters), resulting in a distinctly palpable arterial wall (see section 7.3 for further details).
• Mechanism: The deeply located pulse signifies the location of the disease, while the forcefulness of the pulse infers that the body’s defensive Qi has responded to the presence of the pathogenic factor and moved inwards to fight it.
Internal vacuous condition
The Sinking pulse due to vacuity (deficiency) will present with decreased pulsatile force. The main pattern associated with the Sinking and forceless pulse is Vacuity of Qi and blood, and in particular Yang Qi.
• Mechanism: Yang Qi is unable to lift the pulse so that it can be palpated at the superficial level of depth.
• Clinical relevance: Cold signs and symptoms such as aversion to cold, lethargy and cold extremities usually accompany the Yang vacuity pattern. Clinically this may be seen in hypothyroidism or in severe exhaustion.
6.8.3. Hidden pulse (Fú mài)

6.8.3.1. Alternative names
Deep-lying or Recondite pulse.
6.8.3.2. Requisite parameters
The Hidden pulse is a simple pulse quality defined only by changes in pulse depth. It can only be palpated below the deep level of depth (Fig. 6.8).
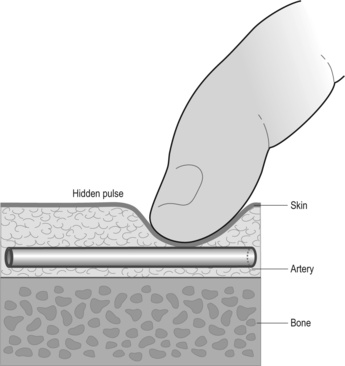 |
| Figure 6.8The Hidden pulse. The anatomical structure of the artery is located adjacent to the bone, deep in the tissue. This means the pulse cannot be felt at the superficial or middle levels of depth simply because there is no arterial structure for the pulse to occur in at these levels. |
6.8.3.3. Clinical definition
The Hidden pulse cannot be palpated at the superficial or middle levels of depth. It is located very deeply, situated just above the bone, requiring extremely heavy pressure with the palpating fingers. It is not necessarily a forceless pulse.
The formation of the Hidden pulse probably results from the actual anatomical location of the physical arterial structure deep in the flesh next to the bone or under other anatomical structures such tendons. In this sense, the Hidden pulse is not about the actual pulse wave, it is about anatomy.
6.8.3.4. Identifying whether the Hidden pulse is present
Step 1: First place the fingers gently on the skin overlying the radial artery, with only the weight of the palpating fingers exerting downward pressure. At this superficial level of depth the radial pulsation cannot be felt.
Step 2: As increasing finger pressure is exerted downwards through the epidermis and dermis and the subcutaneous layer of the hypodermis, the radial artery pulsation may still not be obtained. This is the expected ‘deep’ level of the pulse. Finger pressure is further increased, so that the radial bone can be felt just below the palpating finger tips. At this point the pulsation should be able to be felt.
Step 3: Once the pulse is located, determine its overall strength and rate.
6.8.3.5. Classical description from the Mai Jing and The Lakeside Master’s Study of the Pulse
The hidden pulse is a pulse imperceptible till the fingers touch the bone with extremely heavy pressure … (Mai Jing)
The pulse moves under the sinews (Bin Hue Mai Xue)
6.8.3.6. CM indications
The Hidden pulse is always indicative of pathogenesis, representing a more severe form of internal illness than the Sinking pulse (Box 6.18). The two patterns associated with the Hidden pulse are:
• An internal replete condition
• An internal vacuity condition.
Box 6.18
Summary of Hidden pulses
• Hidden and forceful: Severe obstruction of Yang Qi due to internal pathogenic factors or retained food
• Hidden and forceless: Severe vacuity of Yang Qi leading to internal cold
The two patterns can be differentiated by the parameter of pulse force.
Internal replete condition
The Hidden pulse when forceful indicates a severe obstruction of Yang Qi internally by either pathogenic Cold, retained food, Phlegm or toxic Fire. This pulse has historically been seen in ‘sudden turmoil’ or epidemic illnesses such as cholera like diseases causing severe vomiting and diarrhoea (indication from the Bin Hue Mai Xue, Li, Flaws (trans) 1998: pp. 114-115).
The Hidden pulse when forceless denotes a severe vacuity of Yang causing chronic internal cold, for example vacuity of Kidney Yang.
• Mechanism: The decreased Yang and resulting nature of the Cold that is produced by the severe vacuity of Yang results in the pulse being located at a very deep level, unable to lift the pulse to the exterior. The internal Cold may also impact on the pulse causing stasis and decreasing the flow of Qi and blood. This may also result in a decrease in pulse rate, the Slow pulse and potentially, an increase in arterial wall tension due to the contracting natare of cold.
6.9. Length (longitude)
Pulse length is categorised as a simple pulse parameter that reflects the quantity of Qi and blood circulating in the organs, blood vessels and channels and its smooth unimpeded flow. The parameter of pulse length refers to the presence or absence of a palpable arterial pulsation at the three traditional positions of Cun, Guan and Chi and beyond the Cun and Chi positions. There are two CM pulse qualities that utilise length solely as the defining pulse parameter:
• Long pulse (section 6.11.1)
• Short pulse (section 6.11.2).
The Long and Short pulses are defined only by their length. The palpable pulse length can also increase or shorten with other traditional CM pulse qualities, but this is in combination with changes in other pulse parameters. For example, the Stirred pulse can also be described as a ‘short’ pulse, commonly felt in the Guan position only. However, there are additional changes in the pulse contour, and the Stirred pulse is consequently categorised under the pulse contour parameter.
6.9.1. Pulse length and its assessment
Pulse length is evaluated by checking for the presence of pulsations at each of the three traditional pulse positions and at the pulse positions beyond Cun and beyond Chi, at all levels of depth:
• Beyond Cun is defined as the area of skin on the wrist crease one finger breadth distal, medial and lateral to the Cun position (Box 6.19).
Box 6.19
Presence of pulsations beyond Cun
The presence of the pulse beyond Cun extending into the palmar thenar eminence on the right hand side is said to indicate a constitutional Lung deficiency. This ‘special’ Lung position is found distally and medially to the Cun position where the Lung is represented (Maciocia, 2004: pp 503–504)
• Beyond Chi is defined as the skin region one finger breadth proximal to the Chi position, above the radial artery (Box 6.20).
Box 6.20
Tibetan pulse diagnosis
Traditional Tibetan medicine has a form of pulse diagnosis that requires palpation far beyond the Chi position along the radial artery. Pulse examination as a diagnostic tool has been used by a number of different cultures (see section 2.5). While in CM use of the radial pulse has taken precedence, this wasn’t always the case. The Nine Continents pulse system (using various pulses located on the head and upper and lower limbs) was the main method discussed in the Nei Jing (see section 9.5 for detailed information), until CM theoretical developments in the Nan Jing led to focus upon the radial artery pulsation.
The three pulse positions are located according to the usual procedure. Each position is then palpated individually at all three levels of depth and the absence or presence of pulsations noted. The same procedure is then carried out at the positions beyond Cun and beyond Chi (Box 6.22).
Box 6.21
Questions to consider when assessing pulse length
When looking at the length of the pulse we need to consider the following:
• Under how many fingers is the pulse felt? (exerting even pressure with all three fingers)
• Can the pulse be felt as a continuous length of pulsation under all three fingers?
• Can the pulse be felt beyond the three traditional positions?
• What other factors are associated with the Long and Short pulses? (Hint: deficiency or excess?)
• Are there other signs and symptoms? In an otherwise healthy person the Long pulse can be a sign of abundant Qi and blood.
Box 6.22
Summary of definitions of the pulses defined by the length parameter
• Long: Felt at Cun, Guam and Chi and felt beyond the three positions, beyond the Cun and/or Chi positions (i.e. can be felt closer to thenar eminence and/ or towards the elbow). Classified as Yang.
• Short: Felt in only one or two of the three positions. Usually felt in the guan position plus one of the other two positions. Classified as Yin.
When examining the three traditional positions, it should be noted that there are differences in how ‘easy’ each position may be to palpate. This is associated with the physical characteristics of the radius, with the Cun and Guan pulse positions on the artery being better supported by underlying bony structures than the Chi position and beyond Chi position, so pulsations are more apparent. Note that pulsations can readily be felt beyond Chi position and can also denote health (Table 6.7).
| Presence of pulse | Normal length | Long pulse | Long pulse | Firm pulse | Wiry pulse | Short pulse | Short pulse | Stirred pulse |
|---|---|---|---|---|---|---|---|---|
| Possible pulse patterns | Possible pulse patterns | |||||||
| Beyond Cun | ✓ | |||||||
| Cun | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Guan | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Chi | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Beyond Chi | possible | ✓ | ✓ | ✓ | ✓ | |||
| Simultaneously felt under all three fingers? | ✓ | ✓ | ✓ | |||||
| Increased arterial tension? | ✓ | ✓ | ||||||
6.9.2. Pulse length: CM perspective
The concept of a continuous circulation throughout the body, introduced in the Nei Jing was expanded upon in the Nan Jing (Unschuld 1986) where the First Difficult Issue discusses the movement through the vessels during each inhalation and each exhalation. The contents of the vessels are said to progress six inches with each complete respiration, resulting in fifty complete cycles throughout the body in the ‘course of one day and one night’. Therefore the presence of pulsation at all three pulse positions and beyond is a sign of abundant Qi and blood circulating through the channels and vessels.
The length of the pulse reflects the relative amount of Qi and blood and the circulation of this within the arterial system, organs and channels. Wang noted in the Mai Jing (Wang, Yang (trans) 1997: p. 25) ‘Since the pulse is the mansion of the blood, the Qi is in a good state if the pulse is long, but diseased if the pulse is short’.
Accordingly, changes in pulse length occur as a reflection of health or change as the result of disease. When pathogenic agents or internal disharmony impact on Qi and blood, then Qi and blood can become overactive, obstructed or vacuous (deficient).
The length of the pulse can indicate:
• The overall ‘health’ of an individual
• The relative quality and quantity of Qi and Blood
• The presence of pathogenic heat
• Obstruction of Qi and blood.
6.9.3. Pulse length: biomedical perspective
The presence of arterial pulsations depends on the underlying support of the arterial structure at the point of palpation (by the radial bone in this case) in order to establish an internal/external pressure equilibrium that enables the pulsation to be felt. Additionally, there needs to be sufficient volume for the vessels to be filled. Where the artery is not supported or volume is lessened so the artery and pulsations become less distinct with finger pressure.
6.10. CM pulse defined by length
6.10.1. Long pulse (Cháng mài)

6.10.1.1. Requisite parameters
The Long pulse is a simple pulse quality with changes in the pulse parameter of length. It can be palpated at Cun, Guan and Chi and beyond Chi and/or beyond Cun.
6.10.1.2. Clinical definition
With the Long pulse we are only interested in whether we can feel the pulsation of the radial pulse at each of the three traditional positions and beyond these positions, that is, distal to the wrist crease, in the area of the thenar eminence and beyond the Chi position (defined as one finger breadth proximal to Chi, towards the direction of the elbow). The Long pulse can be palpated at Cun, Guan and Chi, beyond the Chi and maybe beyond the Cun position.
Note: Li (Flaws (trans) 1998: pp. 85-86) describes the Long pulse as not only ‘a pulse which extends beyond its position’ but ‘(It) is not only bowstring but full and distended.’ This description encompasses much more than length, incorporating increased arterial tension, width and an increase in pulse force.
6.10.1.3. Identifying whether the Long pulse is present
Step 1: The radial pulse is examined for the presence or absence of pulsations at the superficial and deep levels of depth and at each of three positions, using the radial styloid process as the anatomical landmark for the Guan position (see Box 6.21 for further information).
Step 2: The positions beyond Cun and beyond Chi are examined for the presence or absence of pulsations at all levels of depth.
‘The long pulse is neither large nor small, Far, far, calm and at ease.
A pulse which extends beyond its position is called long … is not only bowstring but full and distended
6.10.1.5. CM indications
The Long pulse is a simple CM pulse quality defined primarily on the presence of pulsation beyond Cun and/or Chi pulse positions. It is not always considered to be a pathological pulse quality, occurring in individuals with abundant Qi and blood and as well as those who are unwell.
Four patterns are associated with the Long pulse; one is a sign of health, but three represent pathology:
• Abundant Qi and blood (healthy)
• Heat
• Phlegm
• Liver disharmony.
Healthy
In the absence of abnormal signs and symptoms, the Long pulse indicates a normal flow of abundant Qi and blood filling the radial artery. In someone who is not sick, it is a sign of good health. When indicating good health, there is usually no corresponding change in other parameters — that is, the presence of the pulse is simply there. When there is an increase in arterial tension or contour changes then the increase in pulse length probably reflects pathology (see below).
Heat
The Long pulse occurs when Heat agitates the blood causing the blood to expand longitudinally. When Heat pathogens occur there are likely to be changes in other pulse parameters and these need to be assessed in relation to the increase in pulse length. Clinically, an increase in pulse length occurs in fever, but if the Heat is strong then the pulse rate may also increase.
Phlegm
A number of authors mention the Long pulse in connection with the presence of Phlegm or Phlegm fire, relating this clinically to epilepsy and manic symptoms: Deng (1999), Maciocia (2004). However, this would also usually include changes in accompanying pulse parameters.
Liver disharmony
The Long pulse is associated with Liver disease by a number of authors: Deng (1999), Lu (1996) and Maciocia (2004). However, this is not strictly a pattern that is solely associated with the classical Long pulse, as another pulse parameter, arterial wall tension, is also involved. If the Long pulse is accompanied by an increase in arterial tension so that the arterial wall feels increasingly ‘harder’ than usual, and the artery retains this rigidity on increased pressure, then this indicates that there is Liver disharmony. Associated Liver signs and symptoms would be expected to accompany this pulse.
6.10.2. Short pulse (Dûan mài) 

6.10.2.1. Requisite parameters
The Short pulse is a simple pulse quality defined only by the parameter of length. It has a decrease in length, indicated by the absence of a pulsation in at least one of the three traditional pulse positions.
6.10.2.2. Clinical definition
The Short pulse is defined as a pulse that cannot be felt across the three pulse positions of Cun, Guan and Chi, or beyond Cun or beyond Chi. It is usually felt at the Guan position and/or at the Cun or Chi position.
6.10.2.3. Classical description from The Lakeside Master’s Study of the Pulse
A short pulse does not reach its position (Mai Xue).
It responds to the fingers (as if) wound up.
It is not able to fill its position (Mai Jing).
The literature records conflicting views about the application of the term ‘short’ to the radial arterial pulse and the physical manifestation of a Short pulse. For example, authors such as Maciocia, when defining the Short pulse, imply that the pulsation can be short within each position. That is, even when the pulse is clearly felt at the three pulse positions, the pulse can be simultaneously described as ‘short’ for a particular position, because it does not expand across the whole position as it should.
In contrast, Li Shi-zhen, who often described the clinical significance of specific qualities within the Cun, Guan or Chi pulse positions, does not attribute the term short to the pulse in the same sense that Maciocia has. Rather, Li Shi-zhen’s use of the term ‘short’ appears to imply that the Short pulse is used only to describe the situation when there is a total absence of a discernable pulse at one of the three pulse positions Cun, Guan or Chi.
6.10.2.4. CM indications
The Short pulse indicates two main patterns:
• Vacuity of Qi
• Obstruction and stagnation of Qi
Vacuity of Qi (Short and forceless)
The Short pulse that is also forceless indicates Qi vacuity. As Qi leads blood, and accordingly if Qi is vacuous, then blood will not have the motive force to be propelled along the arteries as usual.
One possible interpretation of the Short pulse relates to the relationship between the Cun, Guan and Chi positions and their respective relationship to the upper, middle and lower Heaters of the body. In a situation where pulsations are absent from both the Cun positions, for example, and present in the Guan and Chi positions, then an upper Heater vacuity (deficiency) would be indicated.
Obstruction or stagnation of Qi (Short and forceful)
The Short pulse due to stasis presents with an increase in pulsatile force. Generally this indicates Qi obstruction due to the presence of phlegm or retained food. To relate the three pulse positions to the upper, middle and lower Heaters, it can be seen if there is obstruction in one of the heaters, this can affect communication between the three regions of the body and consequently the formation of the Short pulse. For example, a lack of a pulse in the Cun positions with a strong pulse in the Guan positions and forceless pulses in the Chi positions could indicate an obstruction in the middle Heater; Qi is not being distributed to the upper and lower Heaters.
When the Short pulse only manifests on either the left or right side, and the pulse on the other side is felt normal, then obstructive circulatory disorders disrupting the flow wave within the artery on the affected side need to be considered. From a CM perspective, this may also reflect an organ type disharmony or vacuity according to where the pulsation can not be felt (see section 9.4 on Five Phase pulse diagnosis).
When the Short pulse occurs bilaterally with strength then systemic causes arising from obstruction in the digestive tract need to be assessed.
6.11. Width (latitude)
Pulse width is classified as a simple pulse parameter, which is concerned with the actual tactile presentation of the radial artery across the lateral plane. It is the diameter of the radial artery or the lateral displacement of the pulse wave acting on the radial artery that is examined to determine whether the artery is thinner or wider than would be expected relative to that individual.
Assessment of pulse width provides information mainly pertaining to the volume of circulating Yin fluids. Pulse width may also indicate the level of activity of Qi; the ability of the Qi to move blood outward, and also ‘Qi’ in the broader sense as relating to the presence of Cold or Damp pathogenic factors. In these cases, there are usually accompanying changes in other pulse parameters in conjunction with specific pathological signs and symptoms. In a CM context, pathogenic factors are seen as affecting the pulse width.
Only one CM pulse quality is solely defined by its width; the Fine pulse. The Fine pulse is associated with a decrease in pulse width and is defined as a ‘thin’ pulse quality. Three other CM pulse qualities can be defined as ‘thin’:
The Fine pulse can be seen as the template or prototype pulse of these narrow pulses. It is the presence of changes in other pulse parameters that further differentiate the Soggy pulse, Weak pulse and Faint pulse from the Fine pulse. For example, the Weak pulse, while also a thin pulse, is found at the deep level of depth and is defined primarily by its decrease in pulse force (Box 6.23).
Box 6.23
Further differentiation of pulses presenting with narrow arterial diameter
Any pulse with a narrow diameter can be defined as the Fine pulse. However, if changes in other pulse parameters are also present then this may become another CM pulse quality. For example:
• Narrow + forceless + superficial: Soggy pulse
• Narrow + forceless + deep: Weak pulse
• Narrow + extremely forceless + lack of arterial tension: Faint pulse
• Narrow + increased arterial tension: Stringlike pulse
At the other extreme of the pulse width parameter are several pulse qualities that are associated with an increase in pulse width: Replete pulse, Firm pulse, Tight pulse, Scallion Stalk pulse, Drumskin pulse, Scattered pulse, Vacuous pulse and Surging pulse.
These pulse qualities also have important changes in other pulse parameters such as pulse force or contour and flow wave, and are therefore discussed in the sections on the more relevant pulse parameter to which they relate.
6.11.1. Pulse width and its assessment
The width of the artery is identified manually by determining the proportion of the total arterial circumference that can be palpated under the fingertips. In this way, the pulse or artery is categorised ‘thin’ or ‘not thin’ by the area that the arterial wall displaces laterally on the palpating finger.
The arterial width is examined by using all three fingers to apply pressure simultaneously over the three pulse positions. The pulse is examined at the deep and superficial levels.
There are two basic subdivisions: thin and not thin (Fig. 6.9).
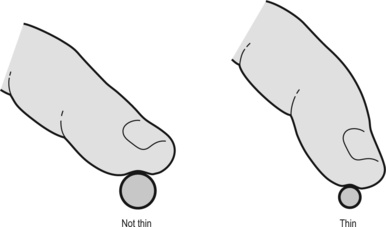 |
| Figure 6.9Cross-sectional schematic of the radial artery and diameter variations with finger palpation. |
Thin
A pulse that is ‘thin’ is defined as having a very narrow arterial diameter, with a definite edge-like feel to it. It does not displace a wide surface area of the fingertip laterally. A greater proportion of the total arterial wall circumference is palpable, indenting the fingertip. Classical descriptions often compare the narrow pulse with a piece of sewing cotton or thread, giving the impression that the arterial wall is definitely palpable within the confines of the fingertips, the artery does not need to be ‘rolled’ to feel the entire arterial width. Alternatively, the artery is seen occupying a relatively small space between the styloid process and the flexor carpi radialis tendon.
The underlying aetiology of a thin pulse means that irrespective of the degree of pressure applied to it, the thin pulse should retain its ‘thin’ classification. For example, a thin pulse felt superficially does not become a ‘wide’ pulse when further finger pressure is applied. If this does occur, then this would not be categorised as a ‘thin’ pulse. It is simply the uppermost level of a wider pulse that is not being sufficiently palpated.
Not thin
A pulse that is ‘not thin’ is any pulse with a diameter wider than the ‘thin’ pulse and this may encompass a pulse width that is neither narrower nor wider than expected, being the norm for that individual. It may also describe a pulse that is broader or wider than it should be, with the pulse expanding both laterally and longitudinally. The category of ‘not thin’ includes those pulses that displace a broad area under the fingertip and possess a distinct arterial wall. It also includes pulses where the arterial wall is not distinctly felt, with the artery felt as an area of pulsation with no clear separation of artery from the surrounding connective tissue, yet the pulse displacement across the finger is wide. The artery occupies a relatively larger space between the styloid process of the radius and the flexor carpi radialis. ‘Not thin’ pulses can equally be forceful or forceless.
Additional palpatory technique
An additional method of palpating the width of the radial artery involves moving the fingers medially and laterally across the artery to check the width (Fig. 6.10). To do this:
• First place the fingers on the skin surface overlying the radial artery.
• Next, feel for the level of depth where the pulsation is felt strongest.
• Maintaining the amount of pressure to locate the pulsation, move the fingers consecutively from medial to lateral (or from left to right) ‘rolling’ the arterial structure under the fingers.
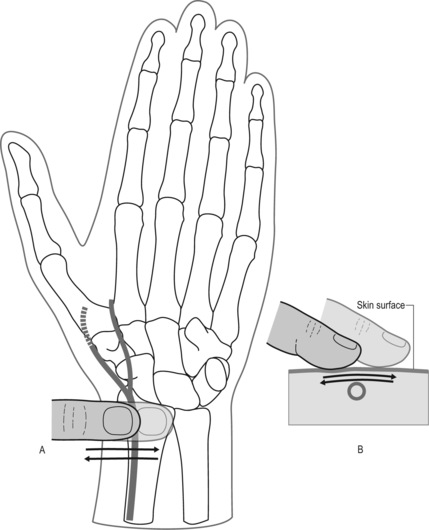 |
| Figure 6.10The rolling technique for assessing arterial width. (The technique is also used for assessing arterial wall tension). |
This method is also used to determine if there is any increased tension in the arterial wall.
When a thin pulse is palpated and the rolling method applied there is very little more that can be felt of the arterial structure. When the pulse is ‘not thin’, the rolling technique further reveals areas of the arterial wall that could not be readily palpated initially. When the arterial wall tension is not distinct, assessment of pulse width is best done by assessing the displacement of the pulse wave across the finger tip.
6.11.2. Normal pulse width
There is no standard quantifiable measure for the normal pulse width, nor consequently a definitive measurement of a thin or not thin pulse, in spite of an objective measurement being obtainable using Doppler ultrasound. The average diameter of the muscular arteries, of which the radial artery is one, is approximately 4 mm (Stables & Rankin 2005: p. 227) but this will vary from individual to individual according to the height and body type.
Broadly speaking, pulse width is considered normal so long as the artery is wide enough to allow sufficient blood flow for tissue perfusion to maintain healthy normal function. In this sense, the pulse width is described in terms of ‘appropriateness’. In terms of the radial artery, ‘appropriateness’ of normal pulse width can be assessed in two ways:
• Response of the peripheral circulation to return to capillary beds when tissue is compressed
• Degree of warmth in the extremities, skin and muscle.
The idea of the pulse width as ‘appropriate’ occurs in a number of classical CM literature sources. For example, the Mai Jing discusses the necessity of taking into consideration a person’s physique:
Large or small, long or short, and whether their nature’s Qi is moderate or impetuous … if the pulse … is in agreement with the form and nature of the person, it is auspicious. Otherwise it is ominous … if the person is small, a female, or thin, the pulse is (accordingly) small and limp.
6.11.3. Variables affecting pulse width
When assessing the appropriateness of pulse width there are several factors to consider, including:
• An individual’s physique
• Temperature
• Body fluids.
6.11.3.1. Physique
A tall person should have a wider pulse than a short person, and someone who is slim would have a smaller arterial width than someone of a larger build. This correlates simply to the relative size of the individual: small, slender individuals have proportionally smaller arteries than individuals of a large build.
6.11.3.2. Temperature
With increased heat in the body, the blood vessels in the skin dilate in an attempt to decrease the core body temperature, leading to an increase in arterial width. This is controlled by inhibition of the sympathetic centres in the posterior hypothalamus that canse vasoconstriction (Guyton & Mall 2006: p. 895).
Variations in the environmental temperature can also cause regulatory changes in the arterial width. For example, climatic cold may cause the blood vessels in the skin to constrict to conserve body heat, thereby decreasing blood vessel width.
6.11.3.3. Body fluids
Body fluids play an important part in the circulatory system, comprising about 60% of the total body weight (Box 6.24). The term ‘body fluids’ refers to both the body water and solutes (substances such as electrolytes) dissolved in it (Tortora & Grabowski 2000: p. 956). An important part of homeostasis involves regulation of body fluids, which helps to maintain the proper functioning of cellular activity. These body fluids consist of intracellular fluid (ICF) fluid and extracellular fluid (ECF). The ECF in blood vessels is called plasma and the ECF that surrounds the cells of tissues is known as interstitial fluid.
Box 6.24
Body fluids
In an average 70 kilogram person body fluids account for about 42 litres (L). This is mainly composed of ICF (inside cells) 28 L, while BCF constitutes the remaining 14 L and is composed of interstitial fluid, plasma and transcellular fluid (fluids found in the synovial, peritoneal, pericardial and intraocular spaces as well as cerebrospinal fluid constituting about 1–2 L in total) (Guyton and Hall 2006: p. 292-3).
Capillary exchange between plasma and interstitial fluid takes place so that nutrients, oxygen, ions and other nutrients can reach cells and waste material such as carbon dioxide and other metabolic by-products can be removed. More fluid moves slowly out of capillaries by filtration than is removed by reabsorption, so this excess interstitial fluid moves into the lymphatic system to become lymph which eventually moves back into the blood. Lymphatic vessels also carry lipids and lipid-soluble vitamins (A, D, E, K) absorbed through the gastrointestinal tract to the blood. About 20 litres of fluid filters out of capillaries each day. Of this, 17 litres is reabsorbed and the remaining 3 litres enters the lymphatic capillaries and becomes lymph.
6.11.4. Regulation of pulse width: CM perspective
The parameter of width refers to arterial diameter. Normal pulse width requires appropriate volume of Yin fluids (Blood, body fluids and Essence) to fill the vessels. The secondary component determining pulse width is sufficient Qi. Sufficient Qi is required to cause the Yin fluids to move in the vessels. This causes the arterial wall to expand, leading to changes in the arterial width. The pulse width is primarily affected when the Yin fluids are affected. This can occur in a number of ways: as a primary problem affecting the fluid volume, or secondary effects on the volume such as quality of Qi and pathogenic factors which affect this (Fig. 6.11). In this context, changes in pulse width occur when the Yin fluids are affected by:
• Internal factors affecting blood volume; fluid can decrease or increase and accordingly the pulse width may also increase or decrease
• External factors such as EPAs affecting blood volume; the Yin or Yang nature of the pathogen determines the effect this will have on pulse width and lateral expansion of the flow wave.
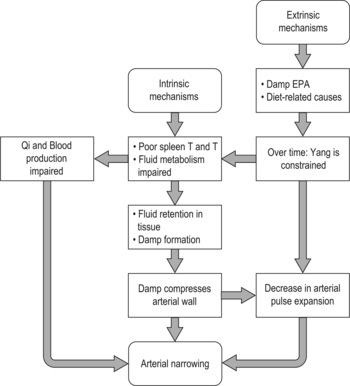 |
| Figure 6.11Extrinsic and intrinsic mechanisms associated with the formation of pulses with a narrow (thin) arterial width. |
6.11.4.1. Volume of Yin fluids
In CM there are three distinct ‘elements’ that are incorporated under the concept of ‘Yin fluids’. These are blood, Yin Ye (thick and thin fluids not associated with blood) and Essence.
Blood and arterial width
Blood is the primary Yin fluid associated with the arterial pulse. From a palpatory perspective, Chapter 53 in the Nei Jing (Ni 1995: p. 190) states:
When the pulse is large and full, there is an abundance of blood. When the pulse is small, thready and weak, there is not enough blood. These conditions are normal; their opposites indicate abnormality.
Blood pathologies affecting pulse width are primarily associated with vacuities (deficiencies). Blood vacuity is associated with either increased or decreased changes in arterial width. The body’s response to blood vacuity often depends on the cause or pathogenesis of the vacuity and the presence of complicating factors such as Damp or Qi vacuity. Primary blood vacuities are associated with an increase in arterial width. When there are Qi and/or Damp complications then arterial width decreases. Table 6.8 lists the association between blood and the CM organs.
| Yin organ | Relationship with blood | Production | Function |
|---|---|---|---|
| Spleen | Blood production | The Spleen converts food and drink into Gu Qi that is sent up to the Lungs | Spleen holds the blood in the vessels-easy bruising occurs when this function is impaired |
| Lung | Blood production | The Lung moves Gu Qi received from the Spleen to the Heart | |
| Heart | Blood production | The Heart converts Gu Qi from the Lungs into Blood | The Heart governs the Blood and blood vessels |
| Kidney | Blood production | The Kidneys provide Kidney | |
| Essence and Yuan Qi for the conversion of Gu Qi into Blood in the Heart | |||
| Liver | Storage and replenishment of Blood | At night the Blood returns to the Liver to be replenished | The Liver helps Blood to move smoothly through the body by ensuring the smooth flow of Qi |
Body fluids and arterial width
Body fluids are the second component of Yin fluids. Clavey (1995) refers to ‘body fluids’ or Jin Ye as:
All the normal physiological fluids in the body, including internal fluids which may be secreted by the Zang organs, such as tears, saliva, sweat, normal nasal mucus and stomach or Intestinal fluids, and also the fluids which act to moisten the various tissues within the body, such as the skin, the flesh, the tendons, the bones and the marrow (p. 1).
Body fluids are classified as Yin, being substantial (in the form of liquids) in comparison to Qi. They play an important part in nourishing and moistening the various tissues of the body and maintaining the fluidity and volume of blood. They are further differentiated into Jin and Ye, with differing functions and textures. Ye fluids have a thicker and more viscous form, lubricating the organs, bones, joints, marrow and brain, for example the synovial fluids lubricating the joints or cerebrospinal fluid bathing the spinal cord and brain comparable to the transcellular component of ECF described in Box 6.24. Jin fluids are thin, clearer and able to flow swiftly, and are responsible for nourishing and moistening the skin and muscles of the exterior body. Sweat is a clear example of a Jin fluid. These fluids can be used for thermoregulation and are able to be transformed into sweat or urine, in order to regulate the level of fluids in the body. Jin fluids flow with Qi and blood within the blood vessels and can be transformed into blood when necessary. Therefore, both blood and Jin contribute to filling out the blood vessels and expanding the arterial diameter.
The relationship between blood and fluids is apparent in dehydration where fluid moves from the blood to replenish tissue fluids. This is reversed in the case of haemorrhage, where fluids move from the tissues to the blood vessels, in order to maintain a functional blood volume for continuing blood supply to the vital organs.
Vomiting, diarrhoea and excessive sweating or urination are ways in which fluid is also lost from the body. As Jin fluids contribute to blood volume, any loss of body fluids may also result in decreased blood volume and thus decreased arterial width.
Fluid pathologies affecting pulse width are often vacuity related, especially in chronic conditions, but may also result from acute viral or bacterial infections (EPAs). Of the two fluid types, ‘thick’ or Ye and ‘thin’ or Jin, it is the Jin fluids which are primarily involved.
Essence and arterial width
Kidney Essence (also known as Kidney Jing) is considered to be one of the fundamental substances that contribute to an individual’s overall health. It is involved in our constitutional health, development and reproductive ability and is also responsible for marrow (the brain) and the material foundation of the Shen or Mind (Maciocia 1989). Kidney Essence is closely related to Yuan Qi, considered as Essence in the form of Qi, and has an integral role in the transformation of fluids by the various Zang Fu organs via the Three Heaters. Kidney Essence and Yuan Qi both play an important part of the transformation of blood in the Heart.
Vacuity of Essence affects pulse width, causing a Fine pulse. This can be seen in a vacuity of Kidney Essence/Jing leading to problems with the production of blood or the transformation of fluids. The natural decline of Kidney Jing occurs with age, therefore, as noted in The Lakeside Master’s Study of the Pulse, the Fine pulse is not unusual in elderly people, but it always indicates a vacuous (deficient) condition.
6.11.4.2. Activity of Qi and arterial width
Qi provides the vitality for the functional operation of the various organs, including the Heart. The Heart is seen as governing or controlling both the blood and the blood vessels. The ability of the Heart to contract and pump blood through the arterial system is dependent on both the condition of Heart Blood and strength of Qi. When the Qi is affected so the heart is affected. This occurs with:
• Qi vacuity
• Pathogenic factors affecting Qi.
Qi vacuity
Vacuity of Qi may affect the strength of the cardiac contraction, resulting in a reduced volume of blood being expelled into the arterial system. This causes a decreased expansion of the radial artery and so can affect the perception of pulse width.
Qi vacuity can also play a role in the accumulation of body fluids and so affects arterial width. Yuan Qi is an important catalyst in the transformation and transportation of Qi and fluids. Therefore vacuity of Yuan Qi can affect any of those steps in the transformative process of fluids.
Pathogenic factors
The presence of a pathogenic factor may impact on the arterial width, causing it to be either narrower or wider than usual.
• Decrease in width: The presence of an internal Yin pathogenic factor such as Damp can decrease arterial width by compressing the artery so that is unable to expand laterally. This may occur due to an abnormal increase in fluid in the connective tissues surrounding the artery, that is, oedema. When Damp causes pulse width to narrow, there is often an underlying vacuity of the body’s Qi and blood allowing this to occur. When Qi and blood are strong and Damp is present, pulse width will not decrease.
• Increase in width: The presence of a Yang pathogenic factor such as Heat or Fire can affect the arterial width by agitating Qi and blood, causing it to expand and thereby increasing the arterial diameter. Heat also affects the contractility of the heart with an increase in cardiac contraction causing greater expansion of the vessel by the resultant pulse wave.
6.11.5. Regulation of pulse width: biomedical perspective
The width or size of the pulse, generally speaking, is related to the circulatory blood volume, the cardiac contractility … Insufficient filling of blood, weak contraction of the heart and the arteries may cause lowering of blood pressure, which will in turn lead to a small or thready pulse.
The circulating blood volume has an effect on the size of the arterial width. A decreased strength of cardiac contraction leads to less blood entering the arterial system, resulting in a decreased expansion of the arterial walls.
Other factors may also influence the arterial width by causing vasoconstriction and vasodilatation of the arteries. This may occur as part of the normal regulation of the body’s metabolic processes known as homeostasis. Homeostasis maintains the body’s internal environment within set physiological limits (Tortora & Grabowski 2000: p. 6). There are several factors that attempt to maintain or regulate homeostasis, including hormonal influences and other processes regulated by the nervous system.
6.11.5.1. Hormonal influence
The endocrine system produces hormones that can influence the action of the heart, blood vessels and blood volume. This is used to maintain a stable blood pressure and ensure the continuous flow of blood throughout the circulatory system to the vital organs, particularly the brain.
Epinephrine (adrenaline) and norepinephrine causes vasoconstriction of the vessels supplying the abdominal cavity and the skin, while causing vasodilatation of vessels to the brain, lung, heart and skeletal muscles. This comes into play during ‘fright, flight or fight’ reactions (Tortora and Grabowski 2006: p. 600).
Antidiuretic hormone (ADH) can affect blood volume especially when there has been excessive blood or body fluid loss due to haemorrhage, dehydration, vomiting, diarrhoea or excessive sweating. Its main action is to decrease urine output, thereby retaining extra fluid that can be returned to the blood to maintain blood pressure. Other effects of ADH include decreasing sweat production and constriction of arterioles, which helps to further retain fluids and increase blood pressure.
The cortex of the adrenal gland secretes aldosterone, a hormone that also helps to maintain body fluid balance by controlling the concentration of sodium and potassium ions. By retaining sodium ions (Na+), this also leads to retention of water and can affect blood volume and arterial width.
Relationship between Qi and Blood
There is a dynamic balance between Qi and blood. Blood depends on the activity of Yang Qi to move it through the blood vessels and Qi depends upon Blood for its nourishing and stabilising influence. When blood becomes vacuous, then the Yang aspect of Qi can become relatively hyperactive. Yang’s nature is to move upward and outward and once the anchoring effect of Yin has been eroded then Yang is more difficult to contain. This is reflected in the pulse by the movement of Yang to the superficial level of depth and may also lead to an increase in pulse width.
6.12.1. Fine pulse (Xì mài)

6.12.1.1. Alternative names
Thin, Thready, Minute or Small pulse.
6.12.1.2. Requisite parameters
The Fine pulse is a simple pulse quality with a change solely in the parameter of arterial width, which is decreased.
6.12.1.3. Clinical definition
The Fine pulse is primarily concerned with the physiological presentation of the arterial width, irrespective of the presentation of the arterial flow wave. The Fine pulse has a narrow arterial width. It has a distinctly palpable arterial wall that retains its form with increasing finger pressure. This is not necessarily a forceless pulse and may be a difficult pulse to occlude, even with heavy pressure. It would be expected that the Fine pulse would be relatively strongest at the middle level of depth. If it is felt strongest at either the deep or superficial level of depth, this would respectively suggest the development of either the Weak pulse or Soggy pulse.
6.12.1.4. Identifying whether the Fine pulse is present
Step 1: The pulse is examined at each level of depth. The arterial width is noted at all levels of depth. It would be expected that the pulse should be narrow at all levels of depth where it can be palpated and probably strongest at the middle level of depth.
Step 2: As the deep level of depth is examined, note whether the pulse is easily occluded or whether it takes considerable pressure to stop the pulsations. This information is used to further differentiate the pathogenesis of the pulse.
6.12.1.5. Classical description from the Mai Jing
The fine pulse is a little larger pulse than the faint pulse, a pulse constantly present yet thin.
Note that the term ‘fine’ is often used in the literature to denote a specific CM pulse quality, the Fine pulse, or, may also be confusingly used as a descriptive term meaning ‘narrow’ that is applied to other CM pulse qualities. For example, when a pulse is fine, superficial and lacking in force it is classified as the Soggy pulse.
6.12.1.6. CM indications
The Fine pulse is always seen as a pathological pulse quality. Three main patterns are associated with the Fine Pulse:
• Blood and Qi vacuity
• Depletion of body fluids
• Internal pathogenic Damp
All three patterns are vacuity-type disorders, as the pathogenic Damp is the result of an underlying failure of fluids to be transformed properly.
Blood vacuity and Qi vacuity (Box 6.25)
Insufficient blood volume circulating through the arterial system leads to an inadequate expansion of the radial artery, resulting in a narrower than normal arterial diameter. This may be the result of decreased blood volume occurring due to loss of blood or through poor production of blood. In addition, vacuity of blood adversely affects Qi, resulting in Qi vacuity. Qi vacuity affects the strength of cardiac contraction and this in turn affects the capacity of the pulse wave to expand the radial artery.
Blood vacuity arises from dysfunction in the production and storage of blood or vacuity due to the loss of blood (Box 6.26).
• Dysfunction in the production or storage of blood: The production of blood involves the interaction of the Spleen, Lung, Heart and Kidney (as noted in Table 6.8) and the Liver plays an important part in the storage of blood. Therefore, although blood vacuity can involve dysfunction any of these organs, it usually involves dysfunction of the Spleen, Heart or the Liver (Maciocia 2004, Wiseman & Ye 1998).
• Loss of blood through abnormal bleeding: If blood vacuity continues to occur untreated then eventually the loss in Yin fluids via blood will lead to a relative imbalance between Yin and Yang, with Yang becoming relatively excessive. Yin is no longer able to exert a stabilising and constraining effect on Yang, resulting in Yang following its natural behaviour of moving outwards and upwards. This results in a pulse that can be felt wider and at a more superficial level of depth than usual and may see a progression of the fine pulse into a Scallion stalk or Vacuous pulse.
Box 6.25
Blood vacuity signs and symptoms
Signs and symptoms of Blood vacuity will depend on which Zang organs are affected. In addition to changes in pulse parameters, Blood vacuity signs and symptoms may include:
• Pale face and lips
• Dizziness
• Pale inside lower rim of eye
• Slow return of blood to nail bed following digital pressure
• Dizziness on rising quickly
• Pale tongue colour
In addition to the general signs and symptoms of Blood vacuity there are other signs and symptoms which occur when Blood vacuity involves certain organs. These are:
• Heart: Palpitations, poor memory, anxiousness, trouble falling asleep
• Liver: Numbness or tingling in limbs, cramping in limbs, blurry vision, floaters in the eyes (‘spots’), ridges on nails
• Spleen: Digestive disturbances, lighter than normal menstruation or even absent period, weakness of muscles
Box 6.26
Causes of Blood loss and vacuity contributing to the formation of the Fine pulse
• Menorrhagia (excessive menstrual bleeding)
• Metrorrhagia (uterine bleeding outside menstruation)
• Nosebleeds
• Haemorrhage (for example, due to trauma or childbirth)
• Haemoptysis
• Gastrointestinal bleeding (for example, stomach ulcer, ulcerative colitis, coeliac disease)
• Poor production of blood can arise as a result of organ-based dysfunction (not producing blood) or through dietary causes (organ functioning well but there are insufficient sources of dietary iron or vitamin B12).
Depletion of body fluids
As previously described, there is a close relationship between blood and body fluids, with body fluids moving into the blood vessels when necessary to replenish blood and maintain its volume and vice versa. The causes of body fluid loss are varied and include excessive sweating, vomiting, diarrhoea or urination (Box 6.27).
Box 6.27
Vacuity of body fluids as a compensatory response to blood loss
• If excessive blood loss occurs, then compensatory mechanisms draw on body fluids outside the blood vessels to replace the fluid within the arterial system. This can then result in deficiency of body fluids, with signs and symptoms such as thirst, dry mucous membranes (such as nose, mouth and eyes, dry throat), cracked lips, decreased urine output, lack of sweating, and dry skin. Depending on the organs affected, menstrual bleeding may become lighter and constipation may occur.
• If there is excessive loss of body fluids, then fluids may leave the arterial system to help replace the lost body fluids. This results in the blood vessels ‘empty and deficient, a condition known as ‘jin withered and blood parched’. As Clavey notes, this can result in severe Shen disturbances, as blood is considered to be the residence of the Shen (Clavey 1995: p. 14).
If there is an excessive loss of body fluids this can also affect the quality and quantity of blood, as there are insufficient body fluids to replenish blood. If severe, body fluids will move from the blood volume to replenish the fluids in the tissue. This may also result in a decreased arterial diameter.
A consequence of movement of fluid in and out of the arterial system would be a change in the viscosity of the blood. An increase in the viscosity of blood can lead to changes in blood viscosity and the smoothness of blood flow (see section 2.3).
Depletion of Kidney Essence may also result in a narrow arterial wall, due to its contribution to the formation of both blood and body fluids via Yuan Qi and Kidney Yang. Depletion of Kidney Essence may arise from natural decline with age, constitutional weakness, or excessive sexual activity.
Internal pathogenic Damp
Pathogenic Damp may arise from dysfunction of the Spleen, which is unable to transform and move fluids correctly. If fluids are not transformed properly, then excessive fluid may leak into the area under the skin (connective tissue layer) exerting increased pressure on the vessels in this layer. This compresses the radial artery so that it cannot expand to its normal width. This also results in a pulse that is not necessarily forceless, as the volume of Blood is being compressed into a smaller arterial diameter.
6.12.1.7. Other literature descriptions
There appears to be differences in the pulse literature regarding the severity of the pathology underlying the Fine pulse:
•Maciocia (2004: p. 480) describes this pulse as indicating a severe deficiency of blood and Qi. It is seen as reflecting a more severe deficiency of blood than the Rough pulse (defined by Maciocia as the Choppy pulse).
•Lu (1996: p. 101) describes the Fine pulse as indicating a mild deficiency while the ‘Feeble’ pulse (known in this text as the Faint pulse) indicates ‘severe deficiency’ such as collapse of Yang due to profuse sweating or massive haemorrhage.
• Li Shi-zhen notes that this pulse would be appropriate if seen in a weak or elderly person.
A common thread linking these opinions is that a vacuity condition of Qi and Yin fluids is the underlying mechanism for the formation of this pulse (Box 6.28). It is the presentation of varying accompanying signs and symptoms that can assist in further differentiating the pathogenesis.
Box 6.28
Summary of causes of change in arterial width
A decrease in pulse width or size can indicate:
• Vacuity of Yin fluids such as blood, body fluids or Essence resulting in insufficient blood or Yin fluids to sufficiently fill the vessel
• Insufficient Qi to propel the blood to the periphery of the body and expand the vessel
• Pathogenic damp compressing the vessel.
An increase in the width of the pulse can indicate:
• The presence of a Yang pathogen which can agitate or cause excessive movement of Qi and Blood. Heat has an expansive quality
• Blood vacuity causing a relative hyperactivity of Yang — floating and wide due to Yin being unable to contain or anchor Yang
6.13. Summary
This concludes the chapter on the simple pulse parameters of rate, rhythm, depth, length and width and their associated CM pulse qualities. These are considered to be simple pulse qualities because they are defined by changes in either a single pulse parameter or, at most, two pulse parameters (Table 6.9).
| CM pulse quality | Pulse parameters involved | Change in parameter | Indications |
|---|---|---|---|
| Rapid pulse | Rate | Increase in rate: >90 bpm | Pathogenic Heat or Fire, heart dysfunction, Yin vacuity |
| Slow pulse | Rate | Decrease in rate: <60 bpm | Pathogenic Cold or sign of health, Yang vacuity |
| Moderate pulse | Rate | Rate of 60 bpm | Pathogenic Damp or sign of health |
| Skipping pulse | Rate | Increase in rate: >90 bpm | Pathogenic Heat or Fire |
| Rhythm | Irregular pause in rhythm | Heart arrhythmia due to heart dysfunction, e.g. pacemaker, | |
| Hyperthyroidism | |||
| Bound pulse | Rate | Decrease in rate: <60 bpm | Pathogenic cold |
| Rhythm | Irregular pause in rhythm | Heart arrhythmia due to heart dysfunction, e.g. pacemaker, | |
| Hypothyroidism | |||
| Intermittent pulse | Rhythm | Regular interruption to rhythm, the closer the pauses, the more severe the condition. | Serious heart disease Severe pain Chronic disease |
| Floating pulse | Level of depth at which pulse is felt relatively strongest | Felt relatively strongest at the superficial level of depth | External Replete condition: Attack of EPA such as Wind Heat or Wind Cold |
| Cannot be felt at the deep level of depth | Internal Vacuous condition: Yin Vacuity | ||
| Sinking pulse | Level of depth at which pulse is felt relatively strongest | Felt relatively strongest at the deep level of depth | Internal replete condition: pathogenic factor of cold or damp, retention of food, phlegm |
| Internal vacuous condition: Yang Qi vacuity, vacuity of Yin organs | |||
| Hidden pulse | Level of depth at which pulse is felt relatively strongest | Very difficult to palpate, requiring extremely strong digital pressure. Felt relatively strongest beyond the deep level of depth | Internal Replete condition: pathogenic factor of cold or damp, retention of food, phlegm, toxic Fire |
| Cannot be felt at the superficial or middle levels of depth | Internal vacuous condition: severe Yang vacuity leading to strong internal cold | ||
| Long pulse | Length | An increase in length: can be felt at Cun, Guan and Chi and beyond Chi and/or beyond Cun | Internal Heat or Fire |
| Sign of good health: abundant Qi and Blood | |||
| Liver disharmony | |||
| Short pulse | Length | A decrease in length: can be felt only in one or two pulse positions | Vacuity: Vacuity of Qi |
| Repletion: Stagnation of Qi | |||
| Fine pulse | Arterial width | Decrease in arterial diameter: narrow | Deficiency of blood, body fluids or Kidney |
| Essence |
If there is one message to take from this chapter it is that changes in the pulse parameters are always happening and this is considered normal or healthy when those changes are in response to maintaining homeostasis or Yin/Yang balance through day-to-day activities. It is when the changes in the pulse parameters are sustained that dysfunction is often indicated, and it is only when the change in the parameter is excessive that it warrants categorisation as a CM pulse quality. For example, an increase in pulse rate does not necessarily mean that the pulse is Rapid. It is only a Rapid pulse when the pulse rate exceeds 90 bpm. So with this in mind, it is acceptable not to feel a CM pulse quality as is defined in the literature, and not all changes in the pulse parameters will always form a CM pulse quality.
In a study by Boutouyrie et al. (2001) looking at the effect of acupuncture on radial artery haemodynamics, in subjects with previous experience of acupuncture, real acupuncture was shown to statistically significantly increase the radial artery diameter (pulse width). There was no change during the sham acupuncture. It was suggested in this study that, ‘acupuncture might be able to decrease smooth muscle tone at the site of a muscular artery’. This occurs due to inhibition of sympathetic vasoconstriction. It hypothesized that this may occur via numerous mechanisms: endogenous opioids (because naloxone counteracted this effect), a centrally mediated reflex response and a presynaptic inhibition of sympathetic nerves. The inhibition of sympathetic vasoconstriction will also have an effect upon arterial tension, resulting in an arterial wall that does not feel as ‘hard’ on palpation. (Refer to arterial wall tension parameter in Chapter 7.)
Interestingly, in this study in naive subjects (subjects that had never had acupuncture before) the radial arterial diameter did not change during real or sham acupuncture. Clinically, the results of the study may have implications for practitioners that use perceived changes in the radial pulse to successfully gauge treatment effects, in regards to using this technique with naive (first time) acupuncture clients.
Thus, rather than always focusing on the CM pulse qualities it is just as important to understand the diagnostic meaning of pulse parameter changes, how and why these occur and the related diagnostic meaning. In this way the information provided by parameter changes is very important for diagnostic purposes.
In the following chapter we move on to the more complex pulse parameters such as arterial wall tension, pulse force, pulse occlusion and pulse contour. It is the various combinations of these complex parameters in conjunction with the simple parameters that produce the more complex CM pulse qualities such as the Firm pulse or the Soggy pulse, to name but two.
Medical AtCor, A clinical guide: pulse wave analysis. (2006) AtCor Medical, West Ryde, NSW .
P Boutouyrie, K Corvisier, M Azizi, et al., Effects of acupuncture on radial artery haemodynamics: controlled trials in sensitized and naive subjects, American Jounal of Physiology-Heart and Circulatory Physiology 280 (2001) 628–633.
Braunwald E, Fauci A, Kasper D et al (eds) Harrison’s principles of internal medicine, Volume 1, 15th edn. McGraw-Hill, New York
S Clavey, Fluid physiology and pathology in traditional Chinese medicine. (1995) Churchill Livingstone, South Melbourne .
J Constant, Bedside cardiology. (1999) Lippincott Williams and Wilkins, Philadelphia .
T Deng, Practical diagnosis in traditional Chinese medicine. (1999) Churchill Livingstone, Edinburgh .
D Danzl, Hypothermia and frostbite, In: (Editors: E Braunwald, A Fauci, D Kasper, et al.) 15th edn Harrison’s principles of internal medicine, Volume 1 (2001) McGraw-Hill, New York; Ch 20.
O Epstein, GD Perkin, DP de Bono, J Cookson, Clinical examination. (1992) Mosby-Wolfe, London .
M Estes, Health assessment and physical examination. 3rd edn. (2006) Thomson Delmar Learning, Southbank, Vic .
B Flaws, Statements of fact in traditional Chinese medicine. (1994) Blue Poppy Press, Boulder, CO .
R Funnell, G Koutoukidis, K Larence, Tabner’s nursing care: theory and practice. 4th edn. (2005) Elsevier, Sydney .
Guangzhou Chinese Medicine College, Inspection of the tongue and pulse taking. (1991) Guangzhou, China. .
A Guyton, J Hall, Textbook of medical physiology. 11th edn. (2006) Elsevier Saunders, Philadelphia .
A Katz, Heart failure pathophysiology, molecular biology and clinical management. (2000) Lippincott Williams and Wilkins, Philadelphia .
T Lee, Chest discomfort and palpitations, In: (Editors: E Braunwald, A Fauci, D Kasper, et al.) 15th edn Harrison’s principles of internal medicine, Volume 1 (2001) McGraw-Hill, New York; Ch 13.
SZ Li, B Flaws, The lakeside master’s study of the pulse. (1998) Blue Poppy Press, Boulder, CO ; (trans).
Y Lu, Pulse diagnosis. (1996) Science and Technology Press, Jinan .
J Lyttleton, Treatment of infertility with Chinese medicine. (2004) Churchill Livingstone, Edinburgh .
G Maciocia, The foundations of Chinese medicine. (1989) Churchill Livingstone, Edinburgh .
G Maciocia, Diagnosis in Chinese medicine: a comprehensive guide. (2004) Churchill Livingstone, Edinburgh .
EN Marieb, Human anatomy and physiology. 5th edn. (2001) Benjamin Cummings, San Francisco .
KL McCance, SE Huether, Pathophysiology: the biologic basis for disease in adults and children. 5th edn. (2006) Elsevier/Mosby, St Louis .
C Mitchell, Y Feng, N Wiseman, Shang han lun on cold damage: translation and commentaries. (1999) Paradigm, Brookline, MA .
M Ni, The Yellow Emperor’s classic of medicine: a new translation of the neijing suwen with commentary. (1995) Shambala, Boston ; (trans).
G Perk, J Stressman, G Ginsberg, et al., Sex differences in the effect of heart rate on mortality in the elderly, Journal of the American Geriatrics Society 51 (9) (2003) 1260–1264.
In: (Editors: D Stables, J Rankin) Physiology in childbearing with anatomy and related biosciences (2005) Elsevier, Edinburgh.
GJ Tortora, SR Grabowski, Principles of anatomy and physiology. 9th edn. (2000) John Wiley and Sons, Inc., New York .
G Townsend, Y De Donna, Pulses and impulses. (1990) Thorsons, Wellingborough .
P Unschuld, Huang di nei jing su wen. (2003) University of California Press, Berkeley .
P Unschuld, Nan ching: the classic of difficult issues. (1986) University of California Press, Berkeley .
SH Wang, S Yang, The pulse classic: a translation of the mai jing. (1997) Blue Poppy Press, Boulder, CO ; (translator).
N Wiseman, F Ye, A practical dictionary of Chinese medicine. 2nd edn. (1998) Paradigm Publications, Brookline, MA .