CHAPTER 3 Shoulder Biomechanics, Examination, and Rehabilitation Principles
Orthopedic surgeons frequently rely only on the evaluation of the musculoskeletal system to arrive at a clinical diagnosis. Although this is reliable in assessing acute injuries, deficits in the sensorimotor system, which consists of posture, postural stability, muscle tone, and movement patterns, play a significant role in the development of chronic musculoskeletal pain and therefore must be included in the consideration of cause.1
SHOULDER BIOMECHANICS
The Shoulder in the Kinetic Chain
The shoulder complex functions as part of a kinetic chain, which is defined as a series of links and segments activated sequentially in a coordinated fashion to generate and transmit forces to accomplish a specific function.2,3 An example of a kinetic chain is the childhood game crack the whip, wherein a group of children hold hands in a line to try to accelerate the last child by creating a whip effect. Each child represents a segment of the chain and their joined hands represent links that sequentially create increased energy, force, and velocity. In activities that use a throwing motion (e.g., pitching or tennis), there is proximal to distal muscle activation and coordination of body segments producing interactive moments at the terminal segment (hand or racket).4,5 The initiating ground reaction force is increased as it is transmitted through the knees and hips through the large muscles of the legs into the lumbopelvic region and the rest of the trunk. The proximal segments—that is, the legs and trunk—produce roughly half the energy (51%) and force (54%) that is ultimately delivered to the distal end of the kinetic chain.6,7 The scapula and glenohumeral joint function as both a link and segment in the chain, increasing the kinetic energy and force generated, and as a conduit to funnel and transmit these forces to the distal segments.
When an individual reaches, pushes, or pulls from a sitting position, there is less energy and force contribution from the legs, and the primary generator for upper extremity motion is the initiation of trunk stabilization. Coordinated muscle activation sequences result in movement patterns, which create joint motions to efficiently accomplish specific tasks. These diagonal activation patterns create a “serape effect” from the knee or lumbopelvic region to the shoulder,8 act locally on one joint or harmonize several joints, provide cocontraction force couples that control joint perturbations and provide stability, and generate and transmit force. This allows the scapular stabilizing muscles to position the scapula optimally for shoulder function and for the rotator cuff to compress and position the humeral head in the glenoid fossa.
The Scapula in Shoulder Function
The scapula provides anatomic and kinematic connections between the torso and upper extremities. The shoulder muscles can be classified anatomically by their origins and insertions into the axioscapular, scapulohumeral, and axiohumeral group. The axioscapular muscles that attach the scapula to the thorax include the serratus anterior, trapezius, rhomboids, levator scapulae, and pectoralis minor. These scapular stabilizing muscles position the scapula optimally for the humeral head. The serratus anterior and trapezius muscles are so large that the muscle fibers course in different directions and, as a result, both muscles have multiple functions that relate to activity and arm position.9 The scapulohumeral group consists of the supraspinatus, infraspinatus, teres minor, subscapularis, deltoid, and teres major. The rotator cuff muscles provide concavity or compression at the glenohumeral joint and fine-tune humeral head rotation and depression in an attempt to keep the humeral head centered in the glenoid throughout the arc of upper extremity motion. The axiohumeral muscles, the pectoralis major and latissimus dorsi, are the considered the power muscles of the shoulder. Shortening or tightness of these muscles is frequently associated with abnormal glenohumeral kinematics. The biceps and triceps comprise a special category, because they extend from the scapula to the forearm.
The shoulder complex is an important kinematic link between the trunk and arm, providing a stable platform for arm rotation during throwing. The scapulothoracic articulation, and the glenohumeral, acromioclavicular, and sternoclavicular joints, form two individual but paired mechanisms, one an open chain and one a closed chain.10 A closed kinetic chain, such as the one formed by the thorax, scapula, and clavicle, is defined by the terminal link being fixed or immovable. The glenohumeral joint is an open kinetic chain mechanism, allowing movement of the hand as the terminal link. Normal shoulder function and scapulohumeral rhythm require that all four articulations participate in a simultaneous, synchronous, and coordinated manner, and that the muscles controlling them are activated in the correct succession.
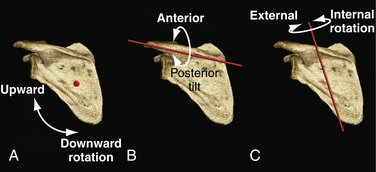
Scapular motions include upward and downward rotation in the coronal plane about an anterior-posterior axis (Fig. 3-1A), anterior and posterior tilting in the sagittal plane about a medial-lateral axis (see Fig. 3-1B), and internal and external rotation in the transverse plane about a vertical axis (see Fig. 3-1C). In addition, there are translations of the clavicle and thus of the scapula, in the superior and inferior directions (scapular movement along the vertical axis), as well as in protraction and retraction or abduction and adduction (scapular movement along the medial-lateral axis). Several investigators have shown that during glenohumeral elevation, the normal scapula demonstrates upward rotation, external rotation, and posterior tilting and translates into a more superior and posterior position.11,12
The scapular stabilizing muscles function as force couples to control the motions of the scapula. A force couple is formed when two forces act in opposite directions to impose rotation about an axis. The serratus anterior controls the movements of internal rotation, upward rotation, anterior tilting, and lateral translation when it fires concentrically, and external rotation, downward rotation, and posterior tilting when it fires eccentrically, depending on shoulder position.13 The upper and lower trapezius and rhomboids counteract this. Scapular elevation is a function of the upper trapezius, levator scapula, and the upper fibers of the serratus anterior. This is counterbalanced by the scapular depression resulting from the functions of the lower portions of the trapezius and serratus anterior.9,14
The Scapula in Shoulder Dysfunction
Abnormal scapular kinematics occur as a result of alterations in anatomy, physiology, and/or biomechanics, or musculoskeletal adaptations to these aberrations, and can usually be classified as being proximally or distally derived (Box 3-1).15 The appropriate term to describe the abnormal scapular movements that occur when the shoulder is moved voluntarily is dyskinesis, as opposed to abnormal involuntary movements, such as in cerebral palsy or Parkinson’s disease, which represent what is termed dyskinesia. When the basic problem occurs proximally and posteriorly to the glenohumeral joint, the observed scapular dyskinesis is considered proximally derived (PDSD). When an abnormality of the glenohumeral joint, subacromial space, clavicle, or acromioclavicular or sternoclavicular joints occurs, the resulting dyskinesis that is usually observed is considered distally derived (DDSD). The exception to this classification is the presence of shortening or tightness of the pectoralis minor or clavipectoral fascia, which fits best into PDSD, despite its anterior position. In the context of the kinetic chain, proximally derived scapular dyskinesis is associated with proximal link or segment weakness or interruption, whereas distally derived dyskinesis is the result of recoil or kickback from a distal link or segment dysfunction. This has important implications for the treatment of shoulder and upper extremity conditions.
Box 3-1 Causes of Scapular Dyskinesis
PDSD is frequently associated with postural dysfunction. The classic presentation is that of the patient who sits or stands with the head in a forward position, with focal cervical lordosis (usually at C5-C6), thoracic kyphosis, anterior tilt, and internal rotation of the scapula and humeral head.1 The anterior tilt is typically associated with tightness or shortening of the pectoralis minor muscle tendon unit, whereas the internal rotation of the humeral head usually results from tightness or shortening of the latissimus dorsi, teres major, pectoralis major, and/or subscapularis.16,17
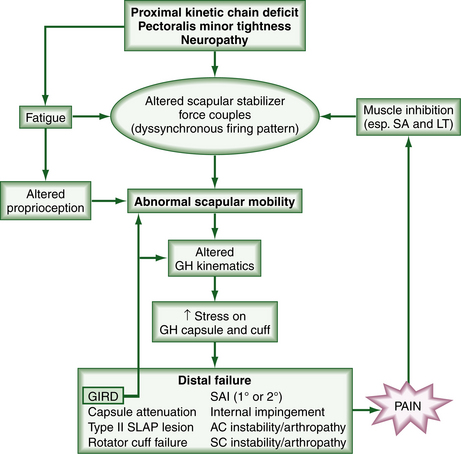
Proximal kinetic chain weakness can be caused by abnormalities of the lower extremities, lumbopelvic, lumbar, or thoracolumbar deficits. Lumbopelvic weakness with resulting core instability appears to be one of the most common causes of proximally derived scapular dyskinesis in the throwing athlete.8 Lumbar lordosis with poor control of the abdominal musculature is frequently associated. Injury to the long thoracic nerve or, less commonly, the spinal accessory nerve, causes weakness and atrophy of the serratus anterior and trapezius, respectively. Long thoracic stretch mononeuropathy is actually more common in overhead athletes than previously thought, and recently has been associated with the use of heavy backpacks by children and young adults (backpack palsy). When these muscles are compromised from neurologic interruption or fatigue, force couple imbalances ensue, and a significant adverse cascade of events occurs (Fig. 3-2). Proprioception is altered, a dyssynchronous muscle firing pattern occurs, and there is an abnormal increase in scapular mobility, which is usually manifested as a loss of external rotation control, with subsequent increased stress on the glenohumeral joint capsule, glenoid labrum, and rotator cuff.18–20 Increased protraction (scapular internal rotation and anterior tilt) has been shown specifically to increase the strain on the anterior band of the inferior glenohumeral ligament and decrease anterior translation of the humeral head.20 Optimum rotator cuff activation occurs only in the presence of a scapula that is optimally positioned for stability. As a result of scapular dyskinesis, there are increased intrinsic joint loads and decreased force delivered to the terminal segment.4
Distally derived scapular dyskinesis is very common and is associated with an array of pathologic conditions.7,18,21-24 Related intra-articular pathology may include labral tears or detachments, capsular attenuation or tears (with resultant instability), focal capsular restrictions such as glenohumeral internal rotation deficit (GIRD) commonly seen in overhead athletes, biceps lesions, adhesive capsulitis, and glenohumeral arthritis. Rotator cuff tendinitis and tears, primary impingement syndrome, and calcific tendinitis have been observed to be associated with scapular malposition. In these cases, the pain and altered biomechanics associated with the pathology appear to cause selective inhibition of the serratus anterior and lower trapezius, with the subsequent events outlined earlier. When glenohumeral internal rotation deficit (GIRD) is present, there is a direct consequence of altered scapular mobility. In any case, there results a vicious cycle of scapular dysfunction and shoulder pathology (see Fig. 3-2).
Subacromial impingement syndrome has historically been associated with abnormal acromial morphology25; however, recent observations have attributed the decrease in the subacromial space height to be more frequently related to a variety of factors that affect scapular position. For example, with increased thoracic kyphosis, there is elevation and anterior tilting of the scapula at rest, decreased upward rotation and posterior tilt of the scapula with glenohumeral elevation, decreased elevation of the glenohumeral joint, and decreased force generated at 90 degrees of scapular plane abduction.26 In addition, it has been shown that with cervical spine flexion of 25 degrees, there is an increase in scapular upward rotation and a decrease in posterior tilting in healthy subjects. Meskers and colleagues27 have demonstrated that the supraspinatus outlet narrows during elevation in the frontal plane from 30 to 130 degrees; however, with external rotation and movement in the horizontal plane, the greater tuberosity moves away from the coracoacromial ligament. Borstad and Ludewig have shown an association between subacromial impingement and anterior tilting, increased internal rotation, and decreased upward rotation of the scapula.28 Cools29,30 has shown that patients with subacromial impingement demonstrate a decrease in peak force for isokinetic protraction, decreased protraction-to-retraction ratio, and decreased electromyographic activity in the lower trapezius, as well as abnormal muscle recruitment in overhead athletes, with delayed activation of the middle and lower trapezius.
EXAMINATION OF THE SHOULDER IN THE CONTEXT OF THE KINETIC CHAIN
Physical Examination
In addition to the clinical history, the key components of the functional examination of the shoulder include assessment of postural alignment, core and lumbopelvic strength and stability, scapulothoracic kinematics, range of motion and movement patterns, muscular imbalances, including lower extremities, hips, and pelvis, glenohumeral joint stability, provocative and corrective maneuvers, and finally palpation.
Assessment of the Kinetic Chain
After the history is completed, the patient is asked to stand in a comfortable posture and observed from the front, back, and side. The patient’s overall standing and seated postures are assessed. Note is made of the relative position of the head and neck and topography of the anterior cervical musculature, elevation or depression of the shoulder girdle, arm position relative to the torso and degree of elbow extension, scapular position, including tilt, rotation, and elevation or depression, abnormal kyphosis, scoliosis or lordosis, pelvic tilt, rotation, or obliquity, and lower extremity malalignment, including hindfoot, midfoot, and forefoot positions. These observations allow the examiner to determine to a great extent the muscle imbalances (e.g., weakness, tightness) that are frequently the underlying pathology causing movement disorders that ultimately cause the presenting symptoms.17 When carefully assessed, patients with shoulder conditions will frequently demonstrate postural muscle imbalance patterns, which Janda has called upper crossed, lower crossed, and layer syndromes.1 In the upper crossed syndrome, the patient presents with a forward head, increased cervical lordosis and thoracic kyphosis, rounded shoulders, and scapular protraction as a result of weak cervical flexors, rhomboids, and lower trapezius muscles and tight pectorals, suboccipitals, upper trapezius, and levators. Lower crossed syndrome patients demonstrate increased pelvic tilt, lumbar lordosis, increased lateral pelvic shift, and increased lateral leg rotation because of weak abdominals and gluteus maximus and tight hip flexors and thoracolumbar and extensor muscles. Patients with the layer syndrome have a combination of upper and lower crossed syndromes and have a poorer prognosis because of the long-standing dysfunction.
While the patient is standing, core and lumbopelvic stability are evaluated by having the patient balance on one leg and do a single leg partial squat while the examiner watches for compensatory movements such as pelvic tilt or rotation, internal rotation of the femur, and/or pronation of the midfoot. Flexibility of the hip flexors using the Thomas test is assessed because iliopsoas shortening or tightness has been clearly implicated in the development of many upper and lower extremity dysfunction diagnoses.1
Scapulothoracic kinematic assessment is accomplished by having the patient slowly elevate and lower the arms in abduction and forward flexion, and observing for dyskinetic scapular motion and/or limitation thereof in the concentric (raising) or eccentric (lowering) phase of scapular stabilizer muscle function (Fig. 3-3). Scapular dyskinesis is most commonly observed during the eccentric phase of lowering the arms from forward flexion. If there is pain or limitation of motion, the test is repeated, with the examiner assisting scapular upward rotation and posterior tilt. If this is successful in decreasing the pain or increasing the motion, it is considered a positive scapular assistance test (SAT).21 Having the patient place his or her hands on the hips with the thumbs pointing posterior and observing scapular position provides an efficient and accurate screening assessment of scapular muscle function.
While the patient is standing, isolated manual muscle testing of the serratus anterior and rotator cuff muscles is performed. The serratus anterior is evaluated by resisted eccentric contraction with the arm elevated above 90 degrees, with the scapula internally rotated and upwardly rotated (protracted) and the elbow flexed to 90 degrees with a downward force being applied to the upper arm (Fig. 3-4). Weakness is demonstrated by giving way and/or scapular winging. We have found this to be more reproducible and valuable than observing the patient doing a wall pushup. Rotator cuff evaluation involves resisted external rotation in adduction (external rotators), resisted scaption at 90 degrees with the thumb pointing up (supraspinatus),31 and resisted internal rotation of the shoulder with the hand on the contralateral shoulder (bear hug test)32 or belly press test33 (subscapularis). If there is demonstrable weakness of the rotator cuff, the test is repeated with the scapula optimally positioned actively or passively to help differentiate between weaknesses that are primarily a result of rotator cuff pathology and those that are secondary to scapulothoracic dysfunction. This is referred to as the scapular retraction test (SRT).15 The scapular assistance and scapular retraction tests are functional corrective maneuvers that provide critical information in making a diagnosis of proximally based scapular dyskinesis.
In addition to postural observations and assessment of scapulohumeral rhythm, muscle imbalances are assessed with the patient in the supine position. Shortness or tightness of the pectoralis minor muscle tendon unit is confirmed by looking for anterior tilt of the scapula and the amount of space between the examination table and the anterior aspect of the acromion. In these patients, as pressure is applied to the anterior shoulder, the upper arm and scapula externally rotate and the hand and forearm move away from the body. While in this position, evaluation for tightness or shortness of the pectoralis major, subscapularis, latissimus dorsi, and teres major is carried out.17
Evaluation of the Subacromial Space, Biceps, and Acromioclavicular Joint
Clinical evaluation of anterior shoulder pain can be confusing and difficult. In our experience, the diagnosis of subacromial impingement syndrome can usually be made on the basis of the corrective maneuvers discussed earlier. However, provocative maneuvers, including resisted internal rotation with the arm in 90 degrees of abduction and 90 degrees of external rotation (90/90 position), and passive internal rotation, starting with the arm in 90 degrees of forward flexion, can be helpful.34 Painful subacromial crepitus with internal rotation in the 90/90 position is somewhat confirmatory. We have not found the Neer impingement sign25 to be helpful in differentiating between the causes of anterior shoulder pain. Long head biceps tendon inflammation can be assessed by comparing the location and severity of anterior pain produced by resisting arm elevation in 90 degrees of forward flexion, with the forearm pronated and supinated (Speed’s test), and repeating the test in 90 degrees of abduction. The diagnosis of an acromioclavicular joint arthropathy is made by the production of anterior pain with passive horizontal adduction (crossover test), forward flexion and, occasionally, with passive extension of the shoulder, in addition to localized tenderness.
Assessment of Capsule and Labrum
Upward of 20 superior labrum anterior posterior (SLAP) tests have been published. Our preferred tests for the clinical detection of a SLAP tear are to use the active compression test and passive distraction test in combination.35,36 For the active compression test, the involved arm is placed in internal rotation at 90 degrees, forward flexion, and 10 to 15 degrees adduction and with the elbow in full extension and the thumb pointed down. A downward force is applied to the arm against resistance. The maneuver is repeated with the palm facing up. The test is considered positive if pain is felt deep within the glenohumeral joint and is decreased or absent when the test is repeated with the forearm supinated. The passive distraction test is performed with the patient lying supine at the edge of the examination table. The affected extremity is elevated to 150 degrees in the coronal plane, with the elbow fully extended and the upper arm stabilized to prevent humeral rotation. If this position is reasonably, comfortable the forearm is pronated. Pain or the sensation of a “pop” deep inside the glenohumeral joint is considered a positive test result. Although in our experience the positive predictive value of either test alone is approximately 70%, if both tests are negative, the negative predictive value is 90% and therefore the diagnosis of a clinically significant SLAP lesion is almost eliminated. If the presenting symptoms and history are consistent with internal impingement syndrome, an attempt is made to reproduce the symptoms using the Mayo shear test.37 For this test, the patient’s arm is passively placed in the 90/90 position and the humeral head is forcefully compressed against the glenoid as it is externally rotated and adducted, producing a painful shearing of the articular side of the rotator cuff against the posterior superior labrum. Determination of excessive capsular laxity, symptomatic instability, and labral integrity are made based on the history in conjunction with load and shift testing in the seated (drawer test) and lateral decubitus positions. The lateral decubitus position allows for a more accurate assessment of all portions of the glenohumeral joint capsule by more effectively limiting scapular motion while the humeral head is translated in all directions while varying the rotation of the arm to create localized capsular tension and feeling for labral clicks and grinds. The structural integrity of the rotator interval and inferior capsule are assessed by comparing the amount of inferior translation with downward traction of the arm with the humeral head in internal rotation (inferior capsule) and external rotation (rotator interval), the Nobuhara test.22 Anterior and posterior apprehension tests, combined with apprehension suppression maneuvers, are helpful for diagnosing clinically significant instability.
If the patient demonstrates a significant limitation of motion with markedly abnormal scapular kinematics, the diagnosis of adhesive capsulitis should be considered, especially in women in their fifth or sixth decade and in diabetic patients. Demonstration of loss of external rotation in adduction, and loss of the inferior sulcus when an inferiorly directed force is applied with the arm in 90 degrees of scaption (or maximum elevation if this level cannot be reached) when compared with the contralateral side, confirms the thickening of the inferior glenohumeral ligament and/or scarring of the rotator interval consistent with this diagnosis. GIRD is a localized capsular contracture of the posterior inferior quadrant. It is confirmed by demonstration of a side to side difference of 25 degrees of humeral internal rotation measured with the scapula fixed against the table, with pressure on the coracoid process with the patient in the supine position.38
PRINCIPLES AND RATIONALE OF CORE-BASED FUNCTIONAL REHABILITATION
The goal of functional rehabilitation is to restore normal function, rather than merely resolve symptoms. Reestablishment of a normal sensorimotor system is dependent on the restoration of normal anatomy by the repair and healing of damaged tissue and restoration of normal muscle length and physiology, with the return of correct joint position and movement, and lastly kinematics, by the activation of muscles in the proper sequences followed by the integration of movements in the kinetic chain. Thus, restoring the integrity of the kinetic chain is the ultimate goal of functional rehabilitation. In some cases, such as in swimmers or patients who function in a seated position, the kinetic chain is somewhat shortened. For this reason, the concept of core-based functional rehabilitation has been introduced.39 Adherence to the principles and guidelines based on the previously discussed concepts regarding scapular function and dysfunction in the context of the kinetic chain allows the rehabilitation process to be more predictable and successful for the clinician, physical therapist, and athletic trainer.
Postural Alignment
For the body to function properly, it must be in proper alignment. Upper quarter posture depends on correct positioning of the pelvis, lumbopelvic region, lower extremities, cervical and thoracic spine, scapula, and shoulder. The physical therapist, through soft tissue releases and stretching, is able to address these postural components. Rehabilitation exercises should be carried out with a neutral spine, appropriate pelvic position, and proper activation of trunk musculature. Shoulder protraction, excessive cervical and lumbar lordosis, and thoracic kyphosis should be corrected whenever possible. Other postural abnormalities, especially thoracic hypomobility, which is commonly seen in these patients, must be corrected early in the rehabilitation process. Exercises should be performed in a position that replicates function. Because of recent adverse changes in insurance reimbursements for physical therapy services and the limitation of allowed visits, we stress having patients take responsibility for correcting their alignment and performing their exercises correctly to make the time with the therapist more productive.
Core Stability
Core stability can be defined as the ability to control the position of the trunk over the pelvis to allow optimum production, transfer, and control of force and motion to the terminal segment in integrated activities.40 The core is central to almost every kinetic chain of sports and work activities and therefore, the importance of core strength, balance, endurance, and control in maximizing function and minimizing injury cannot be overstated. Zazulak and associates41 have explained that for a dynamic system to be stable, there must be accurate and complete feedback information from sensory receptors to the central nervous system (CNS). The CNS must then use this information to generate appropriate input to the muscles and the information accurately relayed to and from the CNS,. The muscles must have sufficient power to bring about quick changes in joint motions. Hodges42 has demonstrated that before arm or leg movement is initiated, the transversus abdominis is consistently activated first to increase the intra-abdominal pressure and stabilize the torso for the anticipated action, thus preventing postural perturbation. Therefore, strengthening of the abdominal musculature and the other core muscles is done early in the rehabilitation process. Much of the central core is made up of larger bulkier muscles, which when functioning properly create a rigid cylinder that prevents body perturbation and allows a more stable base for the more distal components of the kinetic chain. Neuromuscular training, which includes proprioceptive exercise, perturbation, and correction of body sway, allows for improved retraining to restore normal movement control. We have found that the incorporation of the principles of Pilates-based exercises is helpful in reestablishing core strength.
Kinetic Chain
The simple task of lifting the arm integrates the entire body in a feed-forward motor pattern.43 Prior to the onset of anterior deltoid function, the soleus deactivates and the following muscles are sequentially activated: tensor fascia lata, rectus femoris, hamstrings, glutei, and erector spinae. The thoracolumbar fascia connects the lower limbs via the gluteus maximus to the upper limbs via the latissimus dorsi, covers the deep muscles of the back and trunk, including the multifidi, and has attachments to the internal obliques and transverse abdominis muscles, thus integrating the core into the kinetic chain for activities such as throwing. In looking at the contribution of joints and planes of motion to overall task acuity in throwing, Tripp and coworkers44 have shown that the acuity of proximal joints has larger effects on upper extremity tasks than distal joints, and that small deficits proximally develop into larger deficits distally and ultimately have more of an effect on overall acuity of the extremity. Proper activation of trunk musculature and normal trunk and leg strength and flexibility facilitate scapular position, reinforcing the concept of rehabilitation progression from proximal to distal. When possible, correct proximal weaknesses first and then add the upper extremity. During this time, scapular and upper extremity exercises can be done in the seated position to separate the dysfunctional segments. The rehabilitation program should integrate functional movement patterns as soon as possible.
Scapular Position
Ability to position the scapula properly by external rotation and posterior tilting (retraction) and downward rotation (depression) is critical to the success of any shoulder rehabilitation program. The periscapular muscles control the position of the scapula during concentric and eccentric function. For example, when the serratus anterior functions concentrically, it works as a scapular protractor; however, its eccentric function during throwing or overhead activities is to rotate the scapula externally and thus it is important for this muscle to be strengthened eccentrically. Patients should be taught very early in the process (preoperatively if surgery is contemplated) how to “find” their scapula and position it properly to enhance humeral head compression by the rotator cuff and decrease subacromial impingement caused by anterior tilting of the acromion. Normalizing the position of the scapula improves rotator cuff strength by 23% in elevation7 and helps reestablish normal force couples for scapular stabilization and elevation. In some cases, it is helpful to use single- or dual-channel surface biofeedback techniques to monitor muscle activity with auditory and/or visual cues using dual mirrors. We have found inhibition of the upper trapezius or latissimus dorsi and activation of the lower trapezius to be particularly beneficial. It is frequently necessary to reestablish normal length of the periscapular muscles, especially the pectoralis minor, to position the scapula appropriately. It is not uncommon for the postoperative patient to develop subacromial bursitis as a result of inability to position the scapula correctly. Various kinesiotaping and bracing techniques have been developed to decrease the incidence of this occurrence. These techniques do not hold the scapula in position; rather, they provide a proprioceptive link to the brain to stimulate the scapular stabilizing muscles to rotate the scapula externally and tilt it posteriorly (retract and depress) to widen the subacromial space. Walther and colleagues45 have shown that bracing improves shoulder function. This is consistent with our observations using kinesiotape or the Spine and Scapula Stabilizing (S3) brace or Posture Shirt (Alignmed, Santa Ana, Calif) or the Intelliskin shirt (http://www.intelliskin.com) for patients with postural dysfunction and difficulty positioning their scapulae.
Functional Progression
Progression is based on acquisition of function rather than time; therefore, the phases of the rehabilitation program are based on obtaining normal proximal control and proceeding distally. Learning speed and neuromuscular control differ among patients as a result of factors such as different learning abilities, intelligence, age, ability to focus, or comorbidities, such as diabetes. Progress should be monitored by the overall trend of improvement rather than by chronologic landmarks. In general, exercise progression is from general to specific, simple to complex, easy to difficult, proximal to distal, single to multiple plane, isometric stability to isometric movement, stability to mobility, controlled mobility to skill movements, controlled to uncontrolled environment, horizontal to vertical movements, and unidirectional to multidirectional movements.46 In addition, the patient moves from lesser to greater volume, lesser to greater intensity, and lesser to greater frequency.
Therapeutic Exercises
Closed-chain exercises replicate both the physiologic and biomechanical patterns of movement. Physiologically, there is coordinated muscle firing, resulting in rotator cuff muscle coactivation, reciprocal inhibition, and proprioceptive feedback. Biomechanically, there is increased joint compression with decreased shear, translational, and distractive forces on the glenohumeral joint and rotator cuff, and resultant improved control of joint movement and reestablishment of scapulohumeral rhythm. This allows the patient to increase strength and motion while protecting the repaired and/or healing tissue.47–49 Open-chain exercises, which allow movement of the terminal segments, increase the stress on the soft tissue structures; however, they are important in completing the recovery to normal function. These exercises involve concentric movement against gravity with no fixation feedback (e.g., free weight training). In general, progression is from closed-chain to open-chain exercises as healing, strength, and control improve. Incorporation of motor patterns, which include the legs and trunk, should be done as soon as the patient can tolerate these activities. Sequential distal segment activation is facilitated with exercises that connect the hip and trunk with the scapula and the scapula with the rotator cuff. Some exercises are performed in diagonal patterns to reproduce the serape effect.
SUMMARY
A thorough understanding of the kinetic chain and the role of the shoulder in that context allows for the history and physical examination to identify the mechanical flaws that cause the functional deficits that have motivated the patient to present for evaluation. Identification of the true cause of the dysfunction allows for establishment of a rehabilitation program that corrects the mechanical flaws responsible for the pain and/or dysfunction rather than elimination of symptoms, which is the ultimate goal of an effective core-based functional rehabilitation program for the shoulder.
1. Janda V Muscles and motor control in low back pain: assessment and management. Twomey LT, Taylor JR, editors. Physical Therapy of the Low Back. Edinburgh: Churchill Livingstone, 1987.
2. Dillman CJ. Proper mechanics of pitching. Sports Med Update. 1990;5:15-18.
3. Feltner ME, Dapena J. Three-dimensional interactions in a two-segment kinetic chain. Part 1. General model. Int J Sports Biomech. 1989;5:403-419.
4. Kibler WB. Biomechanical analysis of the shoulder during tennis activities. Clin Sports Med. 1995;14:79-85.
5. Putnam CA Sequential motions of body segments in striking and throwing skills: descriptions and explanations. J Biomech, 26(suppl 1); 1993:125-135.
6. Atwater AE Movement characteristics of the overarm throw: a kinematic analysis of men and women performers. Dissertation Abstracts Int, 31; 1971:5819A.
7. Kibler WB. The role of the scapula in athletic shoulder function. Am J Sports Med. 1998;26:325-337.
8. Young JL, Herring SA, Press JM. The influence of the spine on the shoulder in the throwing athlete. J Back Musculoskeletal Rehabil. 1996;7:5-17.
9. Happee R, Van der Helm FC. The control of shoulder muscles during goal-directed movements, an inverse dynamic analysis. J Biomech. 1995;28:1179-1191.
10. Dvir Z, Berme N The shoulder complex in elevation of the arm: a mechanism approach. J Biomech, 11; 1978:219-225.
11. McClure PW, Michener LA, Sennett BJ, Karduna AR. Direct 3-dimensional measurement of scapular kinematics during dynamic movements in vivo. J Shoulder Elbow Surg. 2001;10:269-277.
12. Van der Helm FC, Pronk GM. Three-dimensional recording and description of motions of the shoulder mechanism. J Biomech Eng. 1995;117:27-40.
13. Bagg SD, Forrest WJ. Electromyographic study of the scapular rotators during arm abduction in the scapular plane. Am J Phys Med. 1986;65:111-124.
14. Inman JT, Saunders M, Abbott L. Observations on the function of the shoulder joint. J Bone Joint Surg Am. 1944;26:1-30.
15. Rubin BD, Kibler WB Fundamental principles of shoulder rehabilitation: conservative to postoperative management. Arthroscopy, 18((suppl 2); 2002:29-39.
16. Borstad JD, Ludewig PM. The effect of long versus short pectoralis minor resting length on scapular kinematics in healthy individuals. J Orthop Sports Phys Ther. 2005;35:227-238.
17. Sahrmann SA. Diagnosis and Treatment of Movement Impairment Syndromes. St. Louis: Mosby; 2002.
18. Kebaetse M, McClure P, Pratt NA. Thoracic position effect on shoulder range of motion, strength, and three-dimensional scapular kinematics. Arch Phys Med Rehabil. 1999;80:945-950.
19. McQuade KJ, Dawson J, Smidt GL. Scapulothoracic muscle fatigue associated with alterations in scapulohumeral rhythm kinematics during maximum resistive shoulder elevation. J Orthop Sports Phys Ther. 1998;28:74-80.
20. Weiser WM, Lee TQ, McMaster WC, McMahon PJ. Effects of simulated scapular protraction on anterior glenohumeral stability. Am J Sports Med. 1999;27:801-805.
21. Burkhart SS, Morgan CD, Kibler WB. Shoulder injuries in overhead athletes. The “dead arm” revisited. Clin Sports Med. 2000;19:125-158.
22. Nobuhara K, Ikeda H Rotator interval lesion. Clin Orthop Relat Res (223); 1987:44-50.
23. Ozaki J Glenohumeral movements of the involuntary inferior and multidirectional instability. Clin Orthop Relat Res (238); 1989:107-111.
24. Solem-Bertoft E Thomas KA, Westerberg CE. The influence of scapular retraction and protraction on the width of the subacromial space. An MRI study. Clin Orthop Relat Res (296); 1993:99-103.
25. Neer C2nd Impingement lesions. Clin Orthop Relat Res (173); 1983:70-77.
26. Michener LA, McClure PW, Karduna AR. Anatomical and biomechanical mechanisms of subacromial impingement syndrome. Clin Biomech (Bristol, Avon). 2003;18:369-379.
27. Meskers CG, van der Helm FC, Rozing PM The size of the supraspinatus outlet during elevation of the arm in the frontal and sagittal plane: a 3-D model study. Clin Biomech (Bristol, Avon), 17; 2002:257-266.
28. Borstad JD, Ludewig PM. Comparison of scapular kinematics between elevation and lowering of the arm in the scapular plane. Clin Biomech (Bristol, Avon). 2002;17:650-659.
29. Cools AM, Witvrouw EE, Declercq GA, et al Scapular muscle recruitment patterns: trapezius muscle latency with and without impingement symptoms. Am J Sports Med, 31; 2003:542-549.
30. Cools AM, Witvrouw EE, Declercq GA, et al. Evaluation of isokinetic force production and associated muscle activity in the scapular rotators during a protraction-retraction movement in overhead athletes with impingement symptoms. Br J Sports Med. 2004;38:64-68.
31. Itoi E, Kido T, Sano A, et al. Which is more useful, the “full can test” or the “empty can test,” in detecting the torn supraspinatus tendon. Am J Sports Med. 1999;27:65-68.
32. Barth JR, Burkhart SS, De Beer JF The bear-hug test: a new and sensitive test for diagnosing a subscapularis tear. Arthroscopy, 22; 2006:1076-1084.
33. Gerber C, Hersche O, Farron A. Isolated rupture of the subscapularis tendon. J Bone Joint Surg Am. 1996;78:1015-1023.
34. Hawkins RJ, Kennedy JC. Impingement syndrome in athletes. Am J Sports Med. 1980;8:151-158.
35. O’Brien SJ, Pagnani MJ, Fealy S, et al The active compression test: a new and effective test for diagnosing labral tears and acromioclavicular joint abnormality. Am J Sports Med, 26; 1998:610-613.
36. Schlechter J, Rubin BD The passive distraction test: a clinical exam maneuver to diagnose superior labral pathology. Arthroscopy, 25; 2009:1374-1379.
37. Cheung E, O’Driscoll S. The dynamic labral shear test for superior labral anterior posterior tears of the shoulder. San Diego, Calif: American Academy of Orthopedic Surgeons Annual Meeting; February 14-17, 2007. Paper presented at
38. Burkhart SS, Morgan CD, Kibler WB The disabled throwing shoulder: spectrum of pathology. Part Ipathoanatomy and biomechanics. Arthroscopy, 19; 2003:404-420.
39. Rubin BD. Principles of shoulder rehabilitation. In: Johnson D, Pedowitz R, editors. Practical Orthopaedic Sports Medicine and Arthroscopy. Philadelphia: Lippincott Williams & Wilkins; 2007:323-335.
40. Kibler WB, Press J, Sciascia A. The role of core stability in athletic function. Sports Med. 2006;36:189-198.
41. Zazulak BT, Hewett TE, Reeves NP, et al Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanical-epidemiologic study. Am J Sports Med, 35; 2007:1123-1130.
42. Hodges PW. Is there a role for transversus abdominis in lumbo-pelvic stability. Man Ther. 1999;4:74-86.
43. Zattara M, Bouisset S. Posturo-kinetic organisation during the early phase of voluntary upper limb movement. 1. Normal subjects. J Neurol Neurosurg Psychiatry. 1988;51:956-965.
44. Tripp BL, Uhl TL, Mattacola CG, et al. A comparison of individual joint contributions to multijoint position reproduction acuity in overhead-throwing athletes. Clin Biomech (Bristol, Avon). 2006;21:466-473.
45. Walther M, Werner A, Stahlschmidt T, et al The subacromial impingement syndrome of the shoulder treated by conventional physiotherapy, self-training, and a shoulder brace: results of a prospective, randomized study. J Shoulder Elbow Surg, 13; 2004:417-423.
46. Kelley MJ, Clark CA. Orthopedic Therapy of the Shoulder. Philadelphia: JB Lippincott; 1994.
47. Cipriani D. Open- and closed-chain rehabilitation for the shoulder complex. In: Andrews JR, Wilk KE, editors. The Athlete’s Shoulder. New York: Churchill Livingstone, 1994.
48. Kibler WB, Livingston B. Closed-chain rehabilitation for upper and lower extremities. J Am Acad Orthop Surg. 2001;9:412-421.
49. Uhl TL, Carver TJ, Mattacola CG, et al. Shoulder musculature activation during upper extremity weight-bearing exercise. J Orthop Sports Phys Ther. 2003;33:109-117.