Chapter 88 Should You Save or Substitute the Posterior Cruciate Ligament in Total Knee Replacement?
The posterior cruciate ligament (PCL) serves several important functions in the native knee joint. The PCL is the strongest ligament in the knee and runs from the posteromedial portion of the medial femoral condyle to the posterior aspect of the tibia.1 Because of its direction of attachment, it is the primary ligament resisting posterior subluxation of the tibia on the femur. During flexion, the PCL ensures that the femoral condyles are positioned appropriately on the tibial plateau. The ligament also contains receptors that are sensitive to stretch and allow for normal knee joint proprioception.
OPTIONS
Arguments for Sparing the Posterior Cruciate Ligament in Total Knee Arthroplasty
As the knee is flexed, the PCL tethers the femur to the posterior tibia. This causes the femoral condyles to roll backward on the tibial plateau. The resulting anterior-to-posterior translation of the femur on the tibia has been termed femoral roll back.2 The medial femoral condyle is more constrained than the lateral femoral condyle and, therefore, undergoes less roll back. This causes internal rotation of the tibia on the femur with knee flexion.
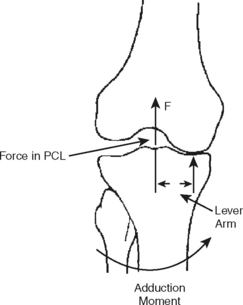
Preservation of normal femoral roll back is suggested as the mechanism for increased passive range of motion. Because of roll back, the femur moves backward on the tibia by 10 mm from full extension to full flexion. This posterior translation of the femur prevents it from impinging on the posterior portion of the tibial plateau during flexion. Posterior translation of the femur by 10 mm also increases the quadriceps lever arm by approximately 40% (Fig. 88-1).1 This improves quadriceps power for knee extension from a flexed position. Proponents of PCL sparing have argued that this leads to improved stair climbing. They have suggested that patients without normal femoral roll back need to lean forward while climbing stairs so that their center of gravity falls anterior to the knee (counteracting the reduced quadriceps lever arm).1
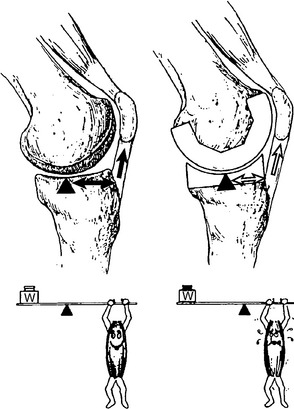
FIGURE 88-1 An illustration of increased quadriceps lever arm due to femoral roll back.
(From Andriacchi TP, Galante JO: Retention of the posterior cruciate in total knee arthroplasty. J Arthroplasty 3(Suppl): 13-19, 1988, p.S17.)
The PCL is the primary stabilizer for posteriorly directed forces on the tibia. These forces may be quite high during normal activities (e.g., approaching body weight during walking).1 Without the native PCL, these forces may be transferred to the bone-implant interface. Two types of PCL-sacrificing implants recreate the posterior stabilizing effect of the PCL using different designs: (1) posterior stabilized (PS) implants have a post on the tibial component and a cam on the femoral component, and (2) ultracongruent (UC) implants have deep troughs in the tibial component to accommodate the femoral condyles. In these PCL-sacrificing implants, a posterior-directed force on the tibia will pass through the tibial component and result in a shear force at the bone-implant interface. This may accelerate loosening of the tibial component.
Because of its location in the middle of the knee, the PCL is also a secondary stabilizer for both varus and valgus forces placed on the tibia.1 The typical varus thrust that occurs with walking on level ground results in an adduction moment about the knee joint. This is resisted by the PCL through a relatively short lever arm (Fig. 88-2). This function of the PCL may not be fully replicated by PS and UC implants. As a result, there may be greater forces through the medial compartment than the lateral compartment when the PCL is sacrificed.
The PCL, like the anterior cruciate ligament (ACL), contains mechanoreceptors that detect knee joint position (i.e., proprioception). These mechanoreceptors sense stress placed on the ligaments and act through a reflex arc to stimulate the dynamic stabilizers of the knee (i.e., muscles that cross the knee joint). Proprioceptive deficiency in the knee may lead to knee instability, gait abnormalities, and difficulties with balance.3 Improved knee joint proprioception through retention of the PCL may result in better patient function after total knee arthroplasty.4
Arguments for Sacrificing the Posterior Cruciate Ligament in Total Knee Arthroplasty
Advocates for PCL-sacrificing total knee arthroplasty generally cite three possible advantages: (1) it facilitates correction of deformity, (2) it enhances range of passive motion, and (3) it decreases stress at the bone-implant interface. Several authors suggest that release of the PCL allows for improved correction in knees with more than 15 degrees of varus or valgus deformity and knees with more than 15 degrees of fixed flexion deformity.5,6 Matsueda and colleagues7 showed in a cadaver study that release of the PCL led to the ability to achieve significantly greater tibiofemoral coronal angles during both medial and lateral releases. They also found that release of the PCL produced extension gaps of 10.9 mm and flexion gaps of 6.6 mm. This would allow for correction of significant flexion deformities.
The PS implant recreates the femoral roll back through the articulation between the cam on the femoral component and the post on the tibial component. Femoral roll back, as stated earlier, allows for increased passive range of motion and quadriceps mechanical function. Through fluoroscopic analysis, femoral roll back has been shown to be more consistent with PS implants than cruciate-sparing implants.8 Some cruciate-sparing implants exhibited paradoxical anterior femoral translation. The UC implant has an anterior lip and tibial surface that conforms to the femoral condyles to substitute for the PCL. This does not recreate femoral roll back; however, the axis of rotation of the femur on the tibia is placed posterior on the tibial plateau. This allows for improved range of motion and quadriceps mechanical function in the absence of femoral roll back.2
The PCL is thought to impart posterior stability to the flexed knee through two mechanisms. First, it is taut in flexion and orientated somewhat horizontal to the tibia, so that it may directly resist posterior displacement of the tibia on the femur.2 Second, the PCL holds the femoral condyles down on the tibial surface. The tibial surface slopes upward anteriorly, and this is further enhanced by the menisci.2 With the PCL securing the femoral condyles to the tibial surface, the condyles will impinge on the anterior sloping tibial surface if the tibia experiences a posterior-directed force. For the PCL to provide posterior stability through these mechanisms, it must have the appropriate tension in flexion. This is achieved by varying bone cuts on the superior tibia and posterior femur (i.e., varying the flexion gap).
The success of total knee arthroplasty with retention of the PCL is highly dependent on proper tensioning of the PCL. If the flexion gap is “overstuffed” (i.e., too large of a femoral component or too thick of a polyethylene spacer), the PCL will be under too much tension with flexion. This causes a large compressive force between the femoral condyles and the posterior aspect of the tibial surface. Unbalanced force on the tibial surface causes the tibial component to “book open” (i.e., the anterior portion of the tibial component lifts off the tibia). This must be recognized intraoperatively and the appropriate measures taken (recessing the PCL, reducing thickness of the spacer, or decreasing size of the femoral component). Otherwise, this unbalanced force on the tibial component will place undue stress on the bone-implant interface. Overtensioning the PCL has also been reported to increase the rate of polyethylene wear and may result in posterior femoral subluxation.9,10 On the other hand, leaving the flexion space too lax or over-recessing the PCL will lead to a slack PCL and subsequent flexion instability.
Evidence
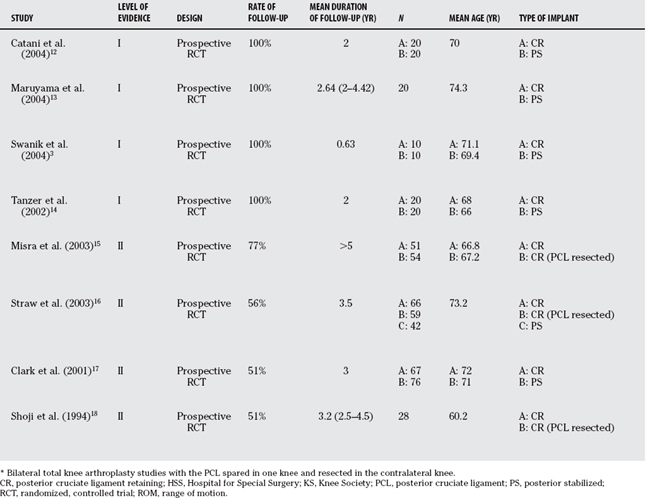
A Cochrane meta-analysis was performed recently to identify differences in functional, clinical, and radiological outcomes for patients receiving either a cruciate retaining or sacrificing total knee arthroplasty.11 Eight randomized, controlled trials were identified in the literature. These consisted of four level I studies and four level II studies (Table 88-1).3,12–18 Two treatment options were compared to PCL retention: PCL sacrifice with use of a PCL-retaining (CR) implant, and PCL sacrifice with use of a PS implant. The group receiving PCL sacrifice with a PS implant were found to have a significantly greater (8.1 degrees; P = 0.01) range of motion after surgery as compared with the CR group. There was no significant difference in range of motion in patients receiving CR implants with either PCL retention or sacrifice. The Hospital for Special Surgery score was significantly better for PCL sacrifice (CR and PS implants together) than PCL retention. This outcome measure evaluates overall patient function and specific clinical variables (e.g., knee range of motion and radiographic appearance). All other variables did not reveal any significant difference between treatment groups. The authors of the Cochrane analysis were reluctant to make conclusions because the methodologic quality of the studies, as determined by the van Tulder score, was quite variable.11 For future studies, they suggest more information on the patient population, more information on the type of treatment and intraoperative findings, and better outcome measures (e.g., range of motion, contact position of the femur on the tibia, and knee stability). Despite their hesitation to make a conclusion, these authors state that there is “strong” evidence that there is no difference between PCL retention and sacrifice using the same prosthesis.11
TABLE 88-1 Studies Reporting Outcomes for Posterior Cruciate Ligament–Retaining Implants, Posterior Cruciate Ligament–Substituting Implants and Posterior Cruciate Ligament Sacrifice with Use of a Posterior Cruciate Ligament–Retaining Implant
Long-term case series (Level IV) are available for similarly designed CR and PS implants. The Press-Fit Condylar prosthesis (PFC; Johnson and Johnson, Raynham, MA) has been used since 1984, and survival data have been published for both CR and PS designs.19 Survival of the CR design has been reported at 91.5% at a mean of 15.8 years, and survival of the PS design has been reported at 94.6% at 12 years.19,20 The similar longevity of these implant designs suggests that the PCL may be substituted without increasing revision rates. Therefore, rates of aseptic loosening, knee instability, and component wear may be unaffected by PCL substitution.
Authors have suggested sacrifice of the PCL and use of a PS implant for certain clinical scenarios: severe deformity (varus/valgus > 15 degrees and fixed flexion deformity > 15 degrees), previous patellectomy, and inflammatory arthritis.6 Laskin21 has reported a retrospective case series (Level IV) showing poor results in patients with a fixed varus deformity treated with a CR prosthesis. Laskin and others5,21 suggest PCL sacrifice and use of a PS implant for varus or valgus deformity greater than 15 degrees (Level V). Lombardi and colleagues6,22 originally believed that a fixed flexion contracture of greater than 15 degrees required PCL sacrifice; however, based on a recent retrospective comparative study (Level III), these authors now recommend an intraoperative algorithm to determine whether the PCL should be sacrificed for flexion deformity. Sacrifice of the PCL is recommended if full extension cannot be achieved with CR trial, or more than 2 mm (beyond the amount required using a measured resection technique) of distal femur must be resected to achieve full extension. Paletta and Laskin23 published a retrospective, comparative trial (Level III) on total knee arthroplasty after a patellectomy that showed superior results for a PS implant as compared with a CR implant. In a case series of CR implants used to treat patients with rheumatoid arthritis compared with a case series of CR implants used to treat patients with osteoarthritis, Laskin and O’Flynn24 found an increased incidence of posterior instability and recurvatum deformity in the patients with rheumatoid arthritis. They recommend use of a PS implant in patients with inflammatory arthritis (Level IV).
AREAS OF UNCERTAINTY
Does Sacrifice of the Posterior Cruciate Ligament Lead to Changes in Knee Joint Proprioception?
The neurosensory function of the PCL is often used as an argument to retain this ligament during knee arthroplasty.4 Proprioception is used to regulate motor control, coordination, and stability of a joint. An association between reduced proprioception and function has been reported in patients with osteoarthritis.3 Given the importance of joint stability and coordination in an elderly population (i.e., prevention of falls), every effort should be made to preserve knee joint proprioception. However, many other structures other than the PCL contribute to proprioception (e.g., ACL, collateral ligaments, and joint capsule). Should the PCL be retained to allow for improved proprioception?
Swanik and colleagues3 conducted a prospective, randomized, controlled trial to investigate the effect of PCL sacrifice on proprioception (Level I evidence). They assessed joint position sense, threshold to detect joint motion, and ability to balance on an unstable platform both before surgery and over 6 months after surgery. Ten patients were randomized to the CR group, and 10 to the PCL-sacrificing group with use of a PS implant group. Joint position sense and balance were significantly better after surgery as compared with before surgery for both treatment groups. The only significant difference between treatment groups was an improvement in joint sensation (sensing extension from a flexed position) for the PS implant group. The authors conclude that arthroplasty improves knee joint proprioception, and sacrifice of the PCL has no significant effect on proprioception. This agrees with two other retrospective comparative studies (Level III) that showed no difference in proprioception with PCL sacrifice.25,26
Is a Posterior Stabilized Implant Required When the Posterior Cruciate Ligament Is Sacrificed?
The PS implant reproduces the stability of the PCL through a post and cam mechanism. Articulation of the tibial post within the femoral cam during flexion also simulates physiologic femoral roll back. However, the cam-post articulation can be an additional source of polyethylene wear debris and may dislocate (i.e., the cam may jump anteriorly over the post) if collateral ligament laxity is present.27 Therefore, UC implants have been proposed as an alternative to PS implants.
Parsley and coworkers28 conducted a retrospective comparative study (Level III) with 121 patients in the PS treatment group and 89 patients in the UC treatment group.28 They found no significant difference between groups for terminal flexion, range of motion, and functional scores at the time of follow-up (the time of follow-up was undefined). The authors conclude that there was no clinical difference between implant designs.
Is it possible to use a CR implant with sacrifice of the PCL? Three Level II studies were identified that compared PS implants with CR implants used without retention of the PCL (see Table 88-1).15,16, 18 These studies did not show any significant difference in range of motion, functional score, or radiographic assessment between the two treatment groups. This led the authors to conclude that a PS implant is not required when the PCL is sacrificed. However, follow-up periods for the studies were relatively short (i.e., only one study had a follow-up period of at least 5 years). Instability and polyethylene wear may become apparent beyond this follow-up time.
The literature contains significant debate regarding the fate of the PCL during total knee arthroplasty. However, both long- and short-term studies suggest little difference between PCL retention and sacrifice. Based on our examination of the literature, we make the following recommendations (Table 88-2):
TABLE 88-2 Grades of Evidence for Recommendations Regarding Posterior Cruciate Ligament in Total Knee Arthroplasty
| RECOMMENDATIONS | LEVEL OF EVIDENCE/GRADE OF RECOMMENDATION |
|---|---|
CR, posterior cruciate ligament retaining; PCL, posterior cruciate ligament; PS, posterior stabilized.
1 Andriacchi TP, Galante JO. Retention of the posterior cruciate in total knee arthroplasty. J Arthroplasty. 1988;3(suppl):13-19.
2 Freeman MA, Railton GT. Should the posterior cruciate ligament be retained or resected in condylar nonmeniscal knee arthroplasty? The case for resection. J Arthroplasty. 1988;3(Suppl):3-12.
3 Swanik CB, Lephart SM, Rubash HE. Proprioception, kinesthesia, and balance after total knee arthroplasty with cruciate-retaining and posterior stabilized prostheses. J Bone Joint Surg. 2004;86-A:328-334.
4 Simmons S, Lephart S, Rubash H, et al. Proprioception following total knee arthroplasty with and without the posterior cruciate ligament. J Arthroplasty. 1996;11:763-768.
5 Laskin RS, Rieger M, Schob C, et al. The posteriorstabilized total knee prosthesis in the knee with a severe fixed deformity. Am J Knee Surg. 1988;1:199-203.
6 Lombardi AVJr, Mallory TH, Fada RA, et al. An algorithm for the posterior cruciate ligament in total knee arthroplasty. Clin Orthop Relat Res. 2001;392:75-87.
7 Matsueda M, Gengerke TR, Murphy M, et al. Soft tissue release in total knee arthroplasty. Cadaver study using knees without deformities. Clin Orthop Relat Res.; 366; 1999; 264-273.
8 Dennis DA, Komistek RD, Mahfouz MR, et al. Multicenter determination of in vivo kinematics after total knee arthroplasty. Clin Orthop Relat Res.; 416; 2003; 37-57.
9 Yamakado K, Worland RL, Jessup DE, et al. Tight posterior cruciate ligament in posterior cruciate-retaining total knee arthroplasty: A cause of posteromedial subluxation of the femur. J Arthroplasty. 2003;18:570-574.
10 Swany MR, Scott RD. Posterior polyethylene wear in posterior cruciate ligament-retaining total knee arthroplasty. A case study. J Arthroplasty. 1993;8:439-446.
11 Jacobs WC, Clement DJ, Wymenga AB. Retention versus sacrifice of the posterior cruciate ligament in total knee replacement for treatment of osteoarthritis and rheumatoid arthritis. Cochrane Database Syst Rev. 2005;4:CD004803.
12 Catani F, Leardini A, Ensini A, et al. The stability of the cemented tibial component of total knee arthroplasty: Posterior cruciate-retaining versus posterior-stabilized design. J Arthroplasty. 2004;19:775-782.
13 Maruyama S, Yoshiya S, Matsui N, et al. Functional comparison of posterior cruciate-retaining versus posterior stabilized total knee arthroplasty. J Arthroplasty. 2004;19:349-353.
14 Tanzer M, Smith K, Burnett S. Posterior-stabilized versus cruciate-retaining total knee arthroplasty: Balancing the gap. J Arthroplasty. 2002;17:813-819.
15 Misra AN, Hussain MR, Fiddian NJ, et al. The role of the posterior cruciate ligament in total knee replacement. J Bone Joint Surg. 2003;85-B:389-392.
16 Straw R, Kulkarni S, Attfield S, et al. Posterior cruciate ligament at total knee replacement. Essential, beneficial or a hindrance? J Bone Joint Surg. 2003;85-B:671-674.
17 Clark CR, Rorabeck CH, MacDonald S, et al. Posterior-stabilized and cruciate-retaining total knee replacement: A randomized study. Clin Orthop Relat Res.; 392; 2001; 208-212.
18 Shoji H, Wolf A, Packard S, et al. Cruciate retained and excised total knee arthroplasty. A comparative study in patients with bilateral total knee arthroplasty. Clin Orthop Relat Res.; 305; 1994; 218-222.
19 Rodricks DJ, Patil S, Pulido P, et al. Press-fit condylar design total knee arthroplasty. Fourteen to seventeen-year follow-up. J Bone Joint Surg Am. 2007;89-A:89-95.
20 Rasquinha VJ, Ranawat CS, Cervieri CL, et al. The press-fit condylar modular total knee system with a posterior cruciate-substituting design. A concise follow-up of a previous report. J Bone Joint Surg Am. 2006;88-A:1006-1010.
21 Laskin RS. Total knee replacement with posterior cruciate ligament retention in patients with a fixed varus deformity. Clin Orthop Relat Res.; 331; 1996; 29-34.
22 Berend KR, Lombardi AVJr, Adams JB. Total knee arthroplasty in patients with greater than 20 degrees flexion contracture. Clin Orthop Relat Res.; 452; 2006; 83-87.
23 Paletta GA, Laskin RS. Total knee arthroplasty after a previous patellectomy. J Bone Joint Surg Am. 1995;77-A:1708-1712.
24 Laskin RS, O’Flynn HM. The Insall Award. Total knee replacement with posterior cruciate ligament retention in rheumatoid arthritis. Problems and complications. Clin Orthop Relat Res.; 345; 1997; 24-28.
25 Cash RM, Gonzalez MH, Garst J, et al. Proprioception after arthroplasty: Role of the posterior cruciate ligament. Clin Orthop Relat Res.; 331; 1996; 172-178.
26 Lattanzio PJ, Chess DG, MacDermid JC. Effect of the posterior cruciate ligament in knee-joint proprioception in total knee arthroplasty. J Arthroplasty. 1998;13:580-585.
27 Puloski SK, McCalden RW, MacDonald SJ, et al. Tibial post wear in posterior stabilized total knee arthroplasty. An unrecognized source of polyethylene debris. J Bone Joint Surg Am. 2001;83-A:390-397.
28 Parsley BS, Conditt MA, Bertolusso R, et al. Posterior cruciate ligament substitution is not essential for excellent postoperative outcomes in total knee arthroplasty. J Arthroplasty. 2006;21(suppl 2):127-131.