Chapter 2 Should Patients Undergoing Decompression for a Grade 1 Degenerative Spondylolisthesis Also Have an Instrumented Fusion?
BACKGROUND
Degenerative spondylolisthesis, spondylolisthesis with an intact neural arch, typically affects patients older than 40 years. The disorder is three times more common in people of African descent, and is four to six times more common in female than male individuals.1 The cause of degenerative spondylolisthesis is thought to derive from a combination of degenerative disc disease and facet arthritis in the presence of ligamentous laxity. Degenerative spondylolisthesis most commonly affects the L4-L5 level. The natural history of degenerative spondylolisthesis was reviewed in Matsunaga and colleagues’2 study, which followed a group of 40 patients over an average of 8.25 years (Level of Evidence 4). This study demonstrates that the conditions of only 10% of patients deteriorated clinically and were a subset of a group of patients who did not demonstrate progression of the spondylolisthesis. In this study, progression of the slip was found in 30% of patients, all of whom were asymptomatic. A majority of these of patients exhibited some improvement in their clinical symptoms over time. In Matsunaga and colleagues’3 long-term follow-up study, progressive slip was found in 34% of 145 nonsurgically managed patients at a minimum of 10 years (Level of Evidence 4). At the beginning of the study, 75% of patients were neurologically normal and remained so at final follow-up. Patients with neurologic symptoms comprised 34% of the patient population, and 84% of this group experienced neurologic deterioration with a resultant poor outcome.3 Several studies have demonstrated a lack of correlation between spondylolisthesis progression and clinical deterioration.4,5
The clinical presentation of symptomatic degenerative spondylolisthesis is similar to spinal stenosis and includes axial back pain, leg pain, or both. The axial component of degenerative spondylolisthesis involves increasing back pain with extension, which distinguishes it from degenerative disc pain that involves increasing pain with flexion. The leg pain caused by degenerative spondylolisthesis may exhibit a radicular component or a neurogenic claudication component, or both. The radicular component exhibits a dermatomal pattern, is often unilateral, and more frequently involves the nerve root traversing the level of the spondylolisthesis. A degenerative spondylolisthesis at L4-L5 produces compression in the lateral recess, which can produce an L5 radiculopathy, manifested by sensory changes in the lateral thigh, lateral calf, and dorsum of foot, as well as extensor hallucis longus motor weakness. A degenerative spondylolisthesis will also anatomically narrow the neural foramen at the level of the slip, thereby compressing the exiting nerve root. As such, a degenerative spondylolisthesis at L4-L5 can also produce an L4 radiculopathy. This is manifested by sensory changes in the anterior thigh and knee extending to the anterior leg and tibialis anterior motor weakness. Neurogenic claudication involves weakness, paresthesias, or pain that typically extends from the thighs into the legs in a nondermatomal distribution and is secondary to central stenosis. The symptoms of neurogenic claudication increase with ambulation or standing because of decreased spinal canal cross-sectional area in lumbar extension leading to nerve root compression.6 The symptoms of neurogenic claudication are improved with lumbar flexion, which increases the canal cross-sectional area.7 Neurogenic claudication may be bilateral or unilateral with pain typically being the predominant symptom. Foraminal, lateral recess, and central stenosis leading to radicular pain or neurogenic claudication in the setting of spinal stenosis are exacerbated by concomitant degenerative spondylolisthesis, which contributes to the compressive effect. Physical examination of patients with a degenerative spondylolisthesis often de-monstrates normal or hypermobility of the lumbar spine. This has been suggested to be secondary to general ligamentous laxity thought to predispose these patients to degenerative spondylolisthesis.
The diagnosis of degenerative spondylolisthesis is confirmed with a radiographic examination of the lumbar spine that includes a standing lateral radiograph.8 A standing lateral radiograph will demonstrate the presence of a spondylolisthesis that is not detected in 15% of patients with supine films alone. Flexion/extension films of the lumbar spine may demonstrate dynamic instability at the level of spondylolisthesis. Computed tomography (CT), with or without myelography, has traditionally been used to further evaluate degenerative spondylolisthesis associated with spinal stenosis. CT gives excellent detail of the source of compression and the osseous pathology. Magnetic resonance imaging (MRI) has been used to further evaluate the source of nerve root compression including disc pathology, facet joint synovial cysts, and ligamentum flavum hypertrophy. An MRI scan may fail to demonstrate a degenerative spondylolisthesis that may be reduced with the patient supine. The “Open Facet Sign” on MRI involves increased T2 signal in the facet joints that are subluxed open. The “Open Facet Sign” may indicate instability in the absence of a visible spondylolisthesis, and ideally the MRI would have been preceded by a standing lateral radiograph of the lumbar spine. More recently, the upright MRI has been developed to further identify soft-tissue pathology with the patient in the standing position. Spondylolisthesis is typically measured in millimeters from the posterior inferior corner of the cephalad vertebra to the posterior superior corner of the caudal vertebra.9 The Meyerding classification of spondylolisthesis provides a simple quantification system for the degree of spondylolisthesis. The Meyerding classification of spondylolisthesis descri-bes the percentage of forward translation of the cephalad vertebral body relative to the end plate of the caudal vertebrae. A grade 1 slip is 0% to 25%, a grade 2 slip is 26% to 50%, a grade 3 slip is 51% to 75%, a grade 4 slip is 76% to 100%, and a grade 5 slip is greater than 100%.10 Although the Meyerding classification system was traditionally used to describe isthmic spondylolisthesis, it can also be applied to degenerative spondylolistheses. As such, translation secondary to degenerative spondylolisthesis can be objectively quantified on a standing lateral lumbar radiograph. Unfortunately, the radiographic differentiation between normal motion and symptomatic instability is more problematic. Clinically significant radiographic instability of the lumbar spine is difficult to distinguish from the reference range of translation seen between motion segments in the lumbar spine.11,12 The importance of identifying clinically significant instability on an upright radiograph secondary to degenerative spondylolis-thesis is essential to selecting the appropriate treatment.
TREATMENT
The classic surgical indications as described by Herkowitz and Kurz13 for degenerative spondylolisthesis are persistent or recurrent leg pain despite a minimum of 3 months of conservative treatment, progressive neurologic deficit, significant reduction in the quality of life, and confirmatory imaging studies concordant with the clinical findings14 (Level of Evidence 5). The options for surgical intervention include decompression alone, decompression and posterolateral fusion with or without instrumentation, or anterior or posterior interbody fusion. The focus of this chapter is to review the literature and evidence available to answer the question, “Should patients undergoing decompression for a grade 1 degenerative spondylolisthesis also have an instrumented fusion?”
EVIDENCE
A meta-analysis of the role of decompression without fusion for the treatment of degenerative spondylolisthesis reviewed 11 articles published from 1970 to 1993.15 The studies reviewed included a nonrandomized retrospective study, two randomized prospective studies, and eight nonrandomized, retrospective, and uncontrolled studies16 (Level of Evidence 4). This study included 216 patients and found that 69% had a satisfactory result, 31% had an unsatisfactory result, and 31% had progression of the spondylolisthesis. This meta-analysis reviewed the literature regarding decompression without fusion only. Another retrospective study reviewed surgeon-reported outcomes of decompression without fusion for degenerative spondylolisthesis. This study examined a group of 290 patients with an average age of 67 years and suggested similar results.17 This study was limited to patients with a stable spondylolisthesis that was defined as a slip with less than 4-mm translation and less than 12 degrees of angulation on flexionextension lateral lumbar radiographs. The average follow-up was 10 years with 69% of patients having excellent results, 13% with good results, 12% with fair results, and 6% with poor results. It was concluded in this group of elderly patients with a stable degenerative spondylolisthesis that a decompression without fusion was a successful procedure with an 82% rate of excellent or good results (Level of Evidence 4).
Another retrospective study reviewed a group of 49 elderly patients with an average age of 68 years with symptomatic degenerative spondylolistheses who underwent decompression without fusion (Level of Evidence 4). These patients all had stable slips on flexion-extension radiographs and were followed for an average of 3.7 years. Clinical instability is defined as the loss of the ability of the spine under physiologic loads to maintain relationships between vertebrae in such a way that there is neither initial nor subsequent damage to the spinal cord or nerve roots; in addition, there is no development of incapacitating deformity or severe pain.18 Gross clinical instability should be suspected whenever there is 4.5 mm of translation or 22 degrees of relative sagittal plane angulation on lateral radiographs.19 This study reported 73.5% excellent or good results with 10% of patients eventually needing an instrumented fusion. The previously referenced studies recommend that, in older patients with stable spondylolistheses, decompression without fusion avoids the significant potential morbidity and mortality related to a fusion procedure in this age group.14,20–22
The role of noninstrumented fusion in the treatment of degenerative spondylolisthesis with instability is generally accepted as beneficial. A meta-analysis reviewing the results of noninstrumented fusions for degenerative spondylolisthesis included a total of six publications.15 This study found a satisfactory clinical outcome in 90% of patients undergoing decompression with a noninstrumented fusion, and 86% of patients achieved arthrodesis. The fusion rate varied significantly between the studies from 30% to 100%. When this group of patients who underwent decompression and fusion were compared with the group of patients who underwent decompression alone, they had statistically significantly better clinical outcomes (Level of Evidence 3).
Herkowitz and Kurz13 performed a prospective and randomized study that compared decompression alone with decompression with noninstrumented fusion in patients with L3-L4 and L4-L5 degenerative spondylolisthesis and associated stenosis. This study demonstrated a statistically significant difference between 44% satisfactory outcomes in the decompression group compared with 96% satisfactory outcomes in the decompression and fusion group. The proportion of excellent outcomes was also significantly greater at 44% for the decompression and arthrodesis group compared with 8% for the decompression alone group (P = 0.0001). This result was independent of the variables of age, sex, preoperative disc height, extent of decompression, or success of achieving a solid arthrodesis. In fact, 36% of the arthrodesis group experienced development of a pseudoarthrosis, but all of these patients had an excellent or good result. In the group of patients who underwent decompression alone, there was a significant increase (P = 0.02) in the progression of spondylolisthesis. This randomized, prospective study demonstrated better clinical outcomes in patients who underwent in situ fusions for degenerative spondylolisthesis with concomitant stenosis (Level of Evidence 1).
The role of fusion in patients with a degenerative spondylolisthesis was investigated by Lombardi and colleagues22a, who completed a study that involved 47 patients who underwent decompression with or without fusion (Level of Evidence 3). These results showed that the patients who underwent a radical decompression faired poorly, and those who received a fusion fared the best. The poor results with decompression without fusion were attributed to the progression of the spondylolisthesis or persistent instability, or both, at the level of the spondylolisthesis. Another smaller study that supported the addition of fusions to decompressive procedures for degenerative spondylolisthesis found that in patients who underwent decompression alone, 45% had good results and 55% had fair or poor results in a group of 11 patients. This was compared with the finding of 63% good results with an arthrodesis and decompression in a group of eight patients.23
A multicenter historical cohort study of 2684 patients with degenerative spondylolisthesis reviewed spinal fusion using pedicle screw instrumentation and found solid arthrodesis in 89% of patients who underwent instrumented fusion and only 70% of patients without instrumentation24 (Level of Evidence 3). The clinical outcomes for the instrumented fusion group were also better relative to the noninstrumented fusion group in this study. A recent comprehensive literature review of lumbar and lumbosacral fusions from 1979 to 2000 reported a trend in increasing instrumented fusions.25
A prospective randomized study compared noninstrumented, semirigid, and rigid instrumented fusions in 124 patients at 1 year after surgery.26 A subset of 56 patients was treated for degenerative spondylolisthesis, and this group achieved a radiographic fusion rate of 65% for the noninstrumented group, 50% for the semirigid instrumentation group, and 86% for the rigid instrumentation group. This study demonstrated a trend toward better clinical outcomes in the group that underwent instrumented fusions that achieved 95% good results compared with 89% for the semirigid instrumentation group and 71% of the noninstrumented group (Level of Evidence 2). A retrospective review of 30 patients undergoing decompression and instrumented fusion for degenerative spondylolisthesis used both radiographic evaluation of arthrodesis and clinical outcomes as measured by the Short Form-36 (SF-36) and patient questionnaire.27 This study demonstrated that both the rate of fusion and the rate of patient satisfaction was 93% despite a 43% complication rate (Level of Evidence 5).
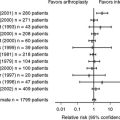
A prospective and randomized study divided a group of patients with degenerative spondylolisthesis into those who received no fusion, noninstrumented posterolateral fusion, and instrumented posterolateral fusion.28 This study demonstrated significantly improved fusion rates, functional outcomes, and sagittal alignment in the instrumented posterolateral fusion group relative to the other groups. This study also showed that slip progression correlated with a poorer outcome in a subgroup of 10 patients who underwent decompression with noninstrumented fusion. The functional outcome was improved in only 30% of patients, and 70% had a progression in their spondylolisthesis that correlated with a poorer outcome (Level of Evidence 1). Another study that examined posterolateral fusion for unstable spondylolisthesis demonstrated that instrumentation significantly improved the functional outcomes if a decompression was performed29 (Level of Evidence 3). Other comparisons between the instrumented and noninstrumented groups, including fusion rates, did not show significant differences. A meta-analysis of the literature on degenerative spondylolisthesis found that of patients who underwent decompression without arthrodesis, 69% had a satisfactory outcome.3 Progression of the spondylolisthesis was noted in the majority of patients in this study. The addition of arthrodesis increased the satisfactory outcome to 90%, with 86% achieving a solid fusion. This meta-analysis also reported a strong trend with increasing fusion rates with instrumentation that did not affect clinical outcomes (Level of Evidence 3).
A prospective and randomized study of 68 patients with degenerative spondylolisthesis and stenosis compared decompression and noninstrumented arthrodesis with decompression and segmental transpedicular instrumented arthrodesis. At an average follow-up of 2 years, there was a significantly greater fusion rate of 83% in the instrumented group compared with the noninstrumented group, which had a fusion rate of 45%.30 Despite the increased fusion rate in the instrumented fusion group relative to the noninstrumented group, there was no significant difference in clinical outcomes with 86% compared with 76% good/excellent outcomes, respectively, at the 2-year time point. Interestingly, a comparison of outcomes at an average follow-up of 7 years and 8 months for 47 patients from both the noninstrumented and instrumented fusion groups demonstrated a significant difference in clinical outcome.31 With this longer follow-up, these two groups of patients exhibited excellent and good clinical outcomes in 86% of patients who experienced development of a solid arthrodesis, but in only 56% of those who experienced development of a pseudoarthrosis. The group of patients who had a solid arthrodesis was reported to have significantly less back pain and a better functional outcome relative to the group of patients who had a pseudoarthrosis. A clear benefit was demonstrated regarding the effects of achieving a solid arthrodesis after decompression for degenerative spondylolisthesis. As such, it was inferred that because instrumented fusions result in a greater rate of arthrodesis and because arthrodesis results in improved long-term clinical outcomes, instrumented fusions produce better long-term clinical outcomes in the treatment of degenerative spondylolisthesis (Level of Evidence 2).
The majority of more recent literature supports decompression with arthrodesis for the treatment of degenerative spondylolisthesis secondary to improved clinical outcomes with successful arthrodesis (grade B). Furthermore, the literature demonstrates that arthrodesis augmentation with transpedicular instrumentation increases the rate of successful fusion (grade A). As such, instrumented arthrodesis for degenerative spondylolisthesis leads to improved clinical outcomes (grade B). The use of instrumentation to augment the arthrodesis should be tailored to the extent of the decompression and the amount of preoperative instability. In the presence of gross instability on preoperative flexion-extension radiographs and in the presence of an aggressive decompression with the associated risks for iatrogenic instability, the immediate stability afforded by an instrumented fusion warrants its increased morbidity, time, and expense (grade B). Furthermore, young and active patient populations with instability and good bone stock are more appropriate surgical candidates for instrumented fusions than are older and sedentary populations with stable degenerative spondylolistheses and poor bone stock. In conclusion, the question “Should patients undergoing decompression for a grade 1 degenerative spondylolisthesis also have an instrumented fusion?” can be answered from the available literature. It can be concluded that because instrumentation increases arthrodesis rates and achieving arthrodesis improves long-term clinical outcomes, instrumented fusions in certain patient populations should also improve long-term clinical outcomes in the surgical management of degenerative spondylolisthesis.32–34
| Summary of Recommendations | ||
|---|---|---|
| STATEMENT | LEVEL OF EVIDENCE/GRADE OF RECOMMENDATION | REFERENCE |
1 Rosenberg NJ. Degenerative spondylolisthesis. Predisposing factors. J Bone Joint Surg Am. 1975;57:467-474.
2 Matsunaga S, Sakou T, Morizono Y, et al. Natural history of degenerative spondylolisthesis: Pathogenesis and natural course of the slippage. Spine. 1990;15:1204-1210.
3 Matsunaga S, Ijiri K, Hayashi K. Nonsurgically managed patients with degenerative spondylolisthesis: A 10- to 18-year follow-up study. J Neurosurgery. 2000;93(2 suppl):194-198.
4 Grob D, Humke T, Dvorak J. Degenerative lumbar spinal stenosis decompression with and without arthrodesis. J Bone Joint Surg Am. 1995;77:1036-1041.
5 Cinotti G, Pstacchini F, Fassari F, et al. Predisposing factors in degenerative spondylolisthesis: A radiographic and CT study. Int Orthop. 1997;21:337-342.
6 Katz J, Dalgas M, Stucki G, et al. Degenerative lumbar spinal stenosis: Diagnostic value of the history and physical examination. Arthritis Rheum. 1995;38:1236-1241.
7 Inufusa A, An HS, Lim TH. Anatomic changes of the spinal canal and intervertebral foramen association with flexion-extension movement. Spine. 1996;21:2412-2420.
8 Bendo J, Ong B. Importance of correlating static and dynamic imaging studies in diagnostic degenerative lumbar spondylolisthesis. Am J Orthop. 2001;30:247-250.
9 O’Brien MF, Kuklo TR, Blanke KM, Lenke LG: Spinal Deformity Study Group. Radiographic Measurement Manual. Medtronic Sofamore Danek USA, Inc., 2004.
10 Meyerding HW. Spondylolisthesis. J Bone Joint Surg. 1931;13:39-48.
11 Hayes MA, Howard TC, Gruel CR, et al. Roentgenographic evaluation of lumbar spine flexion-extension in asymptomatic individuals. Spine. 1989;14:327-331.
12 Boden SD, Wiesel SW. Lumbosacral segmental motion in normal individuals: Have we been measuring instability properly? Spine. 1990;5:571-576.
13 Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis: A prospective study comparing decompression with decompression and intertransverse progressive arthrodesis. J Bone Joint Surg Am. 1991;73:802-808.
14 Turner JA, Ersek M, Herron L, et al. Patient outcomes after lumbar spinal fusions. JAMA. 1992;268:907-911.
15 Mardjetko S, Connolly P, Shott S. Degenerative lumbar spondylolisthesis: A meta-analysis of the literature, 1970-1993. Spine. 1994;19(20 suppl):2256S-2265S.
16 Johnson K, Uden A, Rosen I. The effect of decompression on the natural course of spinal stensosis: A comparison of surgically treated and untreated patients. Spine. 1991;16:615-619.
17 Epstein N, Epstein J. Decompression in the surgical management of degenerative spondylolisthesis: Advantages of a conservative approach in 290 patients. J Spinal Disord. 1998;11:116-122.
18 White AAIII, Panjabi MM. Clinical Biomechanics of the Spine, 2nd ed. Philadelphia: JB Lippincott, 1990.
19 Neumann P, Nordwal A, Osvalder A. Traumatic instability of the lumbar spine: A dynamic in vitro study of flexion distraction injury. Spine. 1995;20:1111-1121.
20 Oldridge N, Yuan Z, Stoll J, Rimm A. Lumbar spine surgery and mortality among medicare beneficiaries, 1986. Am J Public Health. 1994;84:1292-1298.
21 Deyo R, Ciol M, Cherkin D, et al. Lumbar spinal fusion: A cohort study of complications, reoperations, and resource use in the medicare population. Spine. 1993;18:1463-1470.
22 Deyo R, Cherkin D, Loeser J, et al. Morbidity and mortality in association with operations of the lumbar spine. J Bone Joint Surg Am. 1992;74:536-543.
22a Lombardi JS, Wiltse LL, Reynolds JB, Widell EH, Spencer C. Treatment of degenerative spondylolisthesis. Spine. 1985;10:821-827.
23 Feffer H, Wiesel S, Cuckler JM, Rothman RH. Degenerative spondylolisthesis: To fuse or not to fuse. Spine. 1985;10:287-289.
24 Yuan HA, Garfin SR, Dickman CA, et al. A historical cohort study of pedicle screw fixation in thoracic, lumbar, and sacral spinal fusions. Spine. 1994;19(20 suppl):2279-2296.
25 Bono CM, Lee CK. Critical analysis of trends in fusion for degenerative disc disease over the past 20 years: Influence of techniques on fusion rate and clinical outcome. Spine. 2004;29:455-463.
26 Zdeblick T. A prospective randomized study of lumbar fusion. Spine. 1993;18:983-991.
27 Nork SE, Serena SH, Workman KL, et al. Patient outcomes after decompression and instrumented posterior spinal fusion for degenerative spondylolisthesis. Spine. 1999;24:561-569.
28 Bridwell K, Sedgewick T, O’Brien M, et al. The role of fusion and instrumentation in the treatment of degenerative spondylolisthesis with spinal stenosis. J Spinal Disord. 1993;6:467-472.
29 Thomsen K, Christensen FB, Eiskjaer SP, et al. The effect of pedicle screw instrumentation on functional outcome and fusion rates in posterolateral lumbar spinal fusion: A prospective, randomized clinical study. Spine. 1997;22:2813-2822.
30 Fischgrund JS, Mackay M, Herkowitz HN, et al. Degenerative lumbar spondylolisthesis with spinal stenosis: A prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine. 1997;22:2807-2812.
31 Kornblum MB, Fischgrund JS, Herkowitz HN, et al. Degenerative lumbar spondylolisthesis with spinal stenosis. Spine. 2004;29:726-734.
32 McLain RF. Instrumented fusion for degenerative spondylolisthesis, is it necessary. Spine. 2004;29:170.
33 Phillips FM. The argument for noninstrumented posterolateral fusion for patients with spinal stenosis and degenerative spondylolisthesis. Spine. 2004;29:170-172.
34 Fischgrund JS. The argument for instrumented posterolateral for patients with spinal stenosis and degenerative spondylolisthesis. Spine. 2004;29:173-174.