Chapter 89 Should Patella Be Resurfaced in Total Knee Replacement?
The issue of whether the patella should be replaced during total knee replacement (TKR) for osteoarthritis is controversial. Three options are available to the surgeon, namely, always resurface, never resurface, or selectively resurface. This chapter examines the available evidence in the literature to help make a supported decision.
The specific questions examined in this chapter are as follows:
RESURFACING VERSUS NONRESURFACING
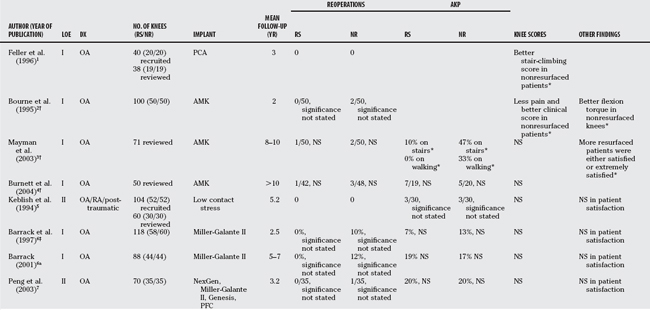
Among the 13 Level I/II studies, only one found an inferior result in the resurfaced group favoring nonresurfacing as the preferred management. Eight studies found conflicting results within the same cohort over time or statistically nonsignificant results. Four studies found superior results in the resurfaced group (Table 89-1).
Evidence Favoring Nonresurfacing
Feller and coauthors1 report a prospective randomized, control trial (RCT) of 40 patients who had unilateral TKR by a single surgeon. Patients with severely deformed patellae were excluded. Removal of osteophytes was performed on the nonresurfaced group, and cemented, all-polyethylene components were inserted in patients in the resurfaced group. One patient in each group had died on follow-up. Thirty-eight knees were reviewed at 3 years after surgery. There were no patellar complications or revisions in either group. No statistically significant difference was found in Hospital for Special Surgery (HSS) and specific Patellar scores between the resurfaced and nonresurfaced groups. Women and heavier patients were found to have significantly lower HSS and Patellar scores. Significantly worse scores were reported for stair climbing in the resurfaced group. The authors conclude that there were no significant benefits to resurfacing the patella if it was not severely deformed.
EVIDENCE FAVORING NEITHER ROUTINE RESURFACING NOR NONRESURFACING
Bourne and colleagues2 report a series of 90 patients in a RCT with 50 knees in each group. At a minimum of 2 years, two nonresurfaced patellae had subsequent resurfacing for intractable knee pain. They found no statistically significant difference in Knee Society functional score, 30-second stair climbing, and the knee extension torque. The nonresurfaced patients had significantly less pain and better clinical rating. At the 8- to 10-year follow-up examination, Mayman and coauthors3 report results on the same group of patients. Twenty-nine patients had died leaving 71 patients to follow-up. One patient in the resurfaced group fell and fractured the patella, requiring a patellectomy. The clinical results had changed since the last report in favor of resurfacing. The incidence of anterior knee pain with walking and stair climbing was significantly less in the resurfaced group. More patients were either satisfied or extremely satisfied in the resurfaced group. At the minimum of 10 years review, Burnett and researchers4 report on 50 knees. From the original 90 patients, 7 refused to participate after enrollment in the study, 36 patients had died, and 2 patients could not attend the follow-up because of dementia and a stroke. Consequently, 45 patients and 50 knees remained to review. One more patient in the nonresurfaced group had had a subsequent resurfacing for anterior knee pain since the last review. No statistically significant difference was found between the groups regarding revision rates, Knee Society clinical rating and functional scores, patient satisfaction, anterior knee pain, and patellofemoral radiographic outcomes. The authors recommend a selective resurfacing approach.
Keblish and colleagues5 report on a quasirandomized, prospective, control trial of 52 patients who had bilateral TKR. Forty-four patients had osteoarthritis, six had rheumatoid arthritis, and two had post-traumatic osteoarthritis. All patients had a resurfacing on one side and nonresurfacing on the other. Fifty-one of the 52 had a metal-backed uncemented mobile-bearing patella, and 1 had a cemented all-polyethylene component. Only 58% (30/52) of patients were available for review. At a mean follow-up examination of 5.24 years, no statistically significant difference was found in subjective preference, performance on ascending and descending stairs, or the incidence of anterior knee pain. The authors conclude that nonresurfaced patellae could perform as well as resurfaced patellae.
Barrack and coauthors6 report on 118 knees in 86 patients at 2.5 years in a RCT. 10% of those in the non-resurfaced group had subsequent resurfacing because of pain. No patient in the resurfaced group had another operation. The statistical significance of this apparent difference in the incidence of reoperation was not reported. No statistically significant difference was found in regarding overall score, pain score, functional score, patient satisfaction, or the incidence of anterior knee pain. At the 5- to 7-year follow-up examination, Barrack and coauthors6a report on 88 knees in 64 patients in the same cohort. One more patient in the nonresurfaced group had had a subsequent patellar resurfacing for anterior knee pain. Again, the statistical significance of the apparent difference in the incidence of reoperation was not reported. No statistically significant difference was found in any of the parameters previously examined. The conclusion of the authors was that the occurrence of anterior knee pain was unlikely to be related to whether the patella was resurfaced.
Peng and investigators7 report on 35 patients having bilateral TKR by a single surgeon in a quasi-randomized prospective study. A variety of implants was used: 30 NexGen (Zimmer, Warsaw, Indiana), 36 Miller-Galante II (Zimmer, Warsaw, Indiana), 2 PFC (Johnson & Johnson, Langhorne, Philadelphia), 2 Genesis (Smith & Nephew, Memphis, Tennessee). One patient in the nonresurfaced group had a patellar realignment for lateral subluxation after a fall. No statistically significant difference was found in Knee Society overall, clinical or function scores, incidence of anterior knee pain or reoperation, and no patient preference for either knee. No recommendation was made by the authors.
Campbell and researchers8 report on 100 TKRs in a RCT. At 10-year follow-up examination, 22 patients had died, 7 had dementia, 10 were lost to follow-up, and 3 had refused to participate because of poor health. Fifty-eight knees were therefore available to be reviewed. Two patients in the nonresurfaced group had undergone subsequent resurfacing for anterior knee pain. One patient in the resurfaced group had an arthroscopic lateral release for lateral tilting and anterior knee pain. No statistically significant difference was found in Knee Society score, Western Ontario and McMaster University Osteoarthritis Index, and specific patellofemoral-related questions. The authors conclude that they were not able to recommend routine resurfacing of the patella.
Evidence Favoring Routine Resurfacing
Schroeder-Boersch and investigators9 report on 40 patients in a RCT. One patient in the nonresurfaced group had a lateral release for subluxation. Better functional and clinical Knee Society scores, as well as better stair-climbing score, were found in the resurfaced group. The authors recommend routine resurfacing, especially in those with severe osteoarthritis. One major deficiency in this article is that there were no preoperative scores on the patients. Because this is known to be the single strongest predictor of postoperative scores, the lack of these scores is a major concern. In addition, the method of randomization was not described.
Newman and colleagues10 reported on a welldesigned RCT involving 125 knees. Forty-two knees were in each of the resurfaced and nonresurfaced groups. Twenty patients had died at the last follow-up; therefore, 105 knees were available for review. No patient in the resurfaced group required a reoperation. Six knees in the nonresurfaced group had a subsequent resurfacing for anterior knee pain. The difference in the incidence of reoperation was statistically significant. No statistically significant difference was found in Bristol Knee score. The authors recommend routine patellar resurfacing.
Wood and coworkers11 report on a well-designed RCT involving 201 patients. Nine had died and 12 had withdrawn from the study. A total of 198 knees in 180 patients were therefore available for review. Fifteen of 128 nonresurfaced knees required a reoperation because of patellofemoral problems. Eleven of these were secondary patellar resurfacing, one had an arthroscopy for anterior knee pain, two had surgeries for mal-tracking, and one had tibial tubercle transfer after a traumatic patellar dislocation. Nine of the 92 resurfaced knees required reoperations. There were five patellar revisions; three of these were done for loosening. One patient had a patellectomy for a comminuted patellar fracture, one had a lateral release, and two had arthroscopies. A significantly lower incidence of anterior knee pain was found in the resurfaced group. There was no statistically significant difference in Knee Society score. Better ability with borderline statistical significance was found in stair descent in the resurfaced group. The authors note that the results of their study are specific to the Miller-Galante type II knee.
Waters and Bentley12 report on 474 knees in 390 patients in a RCT. Eleven of 231 knees had to have a secondary resurfacing in the nonresurfaced group. This was a well-designed RCT looking at the Press Fit Condylar Knee from Johnson & Johnson. In the resurfaced group, one loose patellar component was removed, and two knees had lateral releases. There was a significantly lower incidence of reoperation, lower incidence of anterior knee pain, greater Knee Society score, and higher patient satisfaction in the resurfaced group. The authors recommend routine patellar resurfacing.
Meta-analyses
Forster13 examined three prospective, randomized trials with a minimum of 5-year follow-up and strict inclusion criteria. A 78% follow-up rate was reported with a total of 235 knees. The resurfaced patients had a significantly lower incidence of reoperation. Anterior knee pain could not be analyzed because of study heterogeneity. The authors conclude that there was no mid- to long-term benefit to leaving the patella nonresurfaced.
Pakos and colleagues14 examined 10 prospective, randomized trials with a total of 1223 knees. The range of follow-up was between 1 and 10 years. There was a well-designed meta-analysis with strict inclusion criteria. A significantly lower risk for having a reoperation or anterior knee pain was found in the resurfaced patients. No statistically significant difference was found in terms of knee scores. The authors conclude that routine resurfacing was a marginally superior strategy.
Nizard and coworkers15 examined 12 prospective trials with a total of 1490 knees. Randomized and quasi-randomized trials were included. A significantly lower risk for having a reoperation, anterior knee pain, or pain during stair climbing was found in the resurfaced patients. No statistically significant difference was found in terms of patient satisfaction. The authors conclude that there seemed to be an advantage in routine resurfacing the patella.
Parvizi and investigators16 examined 14 prospective trials with a total of 1519 knees. Randomized and quasi-randomized trials were included. A significantly lower risk for having anterior knee pain and a higher patient satisfaction rate was found in the resurfaced patient. No statistically significant difference was found in the incidence of reoperation, complications, or knee scores. The authors did not make a recommendation.
SELECTIVE RESURFACING
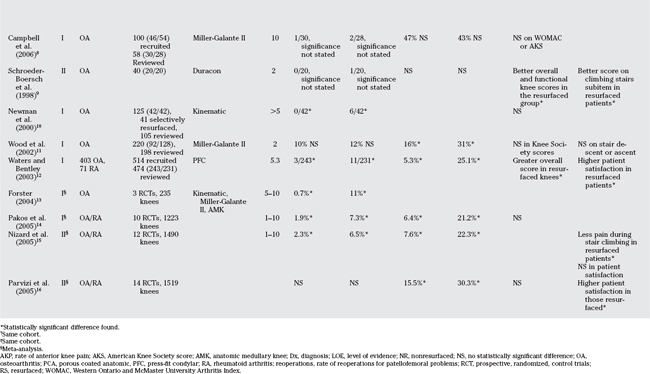
Evidence for and against the Reliability of Predictors for Postoperative Anterior Knee Pain
Four Level I studies and four Level IV studies have presented data on the validity of different predictive factors for postoperative anterior knee pain. These factors include age, sex, weight, height, body mass index, preoperative anterior knee pain, preoperative Knee Society score, preoperative range of movement, degree of osteophytes, grading of the articular surface of the patellofemoral joint, and the need for a lateral release. No Level I/II data are available on the diagnosis of inflammatory arthritis as a predictor of postoperative anterior knee pain. Only the Level I evidence is considered here (Table 89-2).
Newman and colleagues10 found in their RCT that the intraoperative grade of the articular cartilage of the patellofemoral joint did not correlate with the occurrence of postoperative knee pain. Wood and coworkers11 found that age, sex, weight, body mass index, preoperative anterior knee pain, preoperative Knee Society score, preoperative range of movement, grading of patellar articular cartilage, degree of osteophytes formation, and lateral release did not correlate with the incidence of postoperative anterior knee pain. However, when the nonresurfaced group was considered in isolation, the weight of the patient was found to be a significant predictor of anterior knee pain. Waters and Bentley12 found that age, sex, weight, preoperative radiographic appearance, lateral release, and whether the posterior cruciate ligament was sacrificed were not to predictive of postoperative anterior knee pain. Campbell and researchers8 found that the grading of the articular surfaces of either the patella or of the trochlea was not predictive of postoperative anterior knee pain.
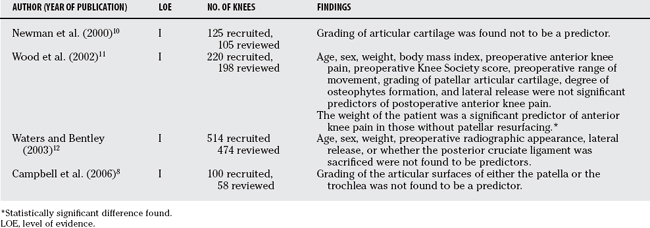
Data on Selective Resurfacing
In contrast with routine resurfacing, there are few direct comparative studies on selective resurfacing against other treatment options in the literature. Most of the evidence on this subject is of low quality. In the English literature, there is one RCT (Level I) comparing routine resurfacing, nonresurfacing and selective resurfacing. There is one case–control study (Level III) and four case series (Level IV). Because of the paucity of Level I-II evidence, studies of all levels of evidence are considered (Tables 89-3 and 89-4).
Selective Resurfacing versus Routine Resurfacing
Newman and colleagues10 compared 42 patients who had their patellae resurfaced and 41 patients who had selective resurfacing of their patellae in an RCT. One patella had to be revised in the selective group for loosening. None of the patients in the resurfaced group had a reoperation. No statistically significant difference was found in terms of incidence of reoperations, Bristol knee score, and clinical Patellar score. However, although not significantly different, the nonresurfaced group and nonresurfaced knees in the selected group scored worse than the knees that were resurfaced, either selectively or by random allocation. The authors recommend routine patellar resurfacing.
Tabutin and coauthors17 report on the incidence of anterior knee pain as a part of a multicenter 5-year clinical and radiologic study on 5915 Nex Gen TKRs. Only osteoarthritic knees with no previous osteotomies or replacements were included. The 2-year results of French (487 knees) and the international (5428 knees) groups were reported. A significantly greater incidence of preoperative anterior knee pain was found in the French group (85.1% vs. 66.6%). The percentage of patellar resurfacing was also found to be significantly different between the two groups with the French resurfacing 98.8% and the international group resurfacing 35.7% of the knees. The main finding in this report was the significant difference in postoperative anterior knee pain with 0.7% in the French group and 6.3% in the international group. The incidence of patellofemoral complication or reoperations was not reported. It must be pointed out that this is not a true comparison between routine resurfacing and selective resurfacing. Not the entire French cohort was resurfaced, and the criteria for resurfacing in the international group were not reported. The authors conclude with caution that resurfacing was a better option with this prosthesis.
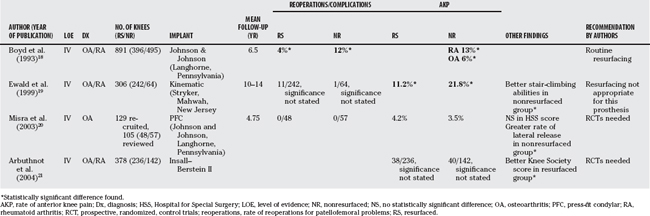
Selective Resurfacing Case Series
Boyd and coworkers18 retrospectively evaluated a group of 891 selectively resurfaced knees. A total of 396 knees were selectively resurfaced based on the gross appearance of the patellofemoral joint and on the patellar tracking intraoperatively. A posterior cruciate–retaining prosthesis was used. Thirty percent of resurfaced knees and 37% of the knees that were not resurfaced had osteoarthritis. The incidence of reoperations was significantly lower in the resurfaced group compared with the nonresurfaced group. The incidence of anterior knee pain was significantly lower in patients with osteoarthritis as compared with those with inflammatory arthropathy in the nonresurfaced group. The authors recommend routine resurfacing when a cruciate-retaining prosthesis was used.
Ewald and colleagues19 reported on a prospective case series of 306 knees. Approximately 45.5% of the patients had osteoarthritis, 49.5% had rheumatoid arthritis, and 5% had post-traumatic arthritis. About 79% of the patellae were resurfaced. The indications included rheumatoid arthritis, eburnated patellofemoral joint, and patellar deformity. Ten of the 242 resurfaced patellae became loose and were revised. One resurfaced patella had to be realigned for recurrent dislocation. One nonresurfaced patella was resurfaced for recurrent dislocation. A significantly greater incidence of anterior knee pain was found in the nonresurfaced group, but significantly better stair-climbing abilities were found in the nonresurfaced group. The authors conclude that routine resurfacing may not be the most effective strategy with that prosthesis.
Misra and coauthors20 report a case series on 105 TKRs that were treated with selective resurfacing. The criteria for resurfacing included preoperative patellofemoral symptoms, patellar instability/malalignment, and grade III-IV articular changes. Forty-eight knees were resurfaced according to these criteria. A significantly greater incidence of lateral release was found in the nonresurfaced group. No statistically significant difference was found in the incidence of anterior knee pain or in the HSS score. No revisions were required in any knees. The authors conclude that an RCT was needed.
Arbuthnot and investigators21 report on a prospective case series of 378 TKRs. All of these knees had preoperative patellofemoral pain. A total of 236 knees were resurfaced at the surgeons’ discretion. The criteria for resurfacing were not described. A significantly better Knee Society score was found in the resurfaced group. No statistically significant difference was found in the incidence of postoperative anterior knee pain, reoperations, or complications. The authors were unable to make a recommendation.
CONCLUSION
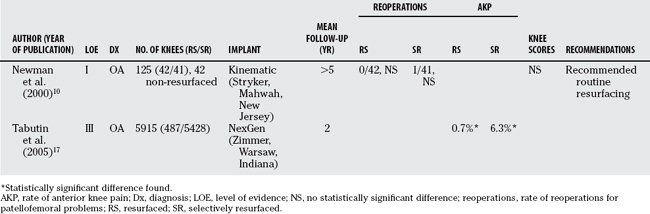
To date, the best evidence available supports routine resurfacing of the patella. This is based on three well-designed RCTs and two meta-analyses. However, the conclusions of these studies are specific to the prosthesis used. Meta-analysis, although providing some insight, again is limited because of many factors including limited number of high-quality RCTs, multiple prosthetic designs, multiple surgeries, and ill-defined primary outcomes. Given that this is an important question to be answered, future high-quality RCTs are of value. However, equally important is the clinician’s decision on what primary outcome would be of utmost importance for him/her and his/her patients. In this way, RCTs can be appropriately powered to show a difference in important clinical outcome if the difference truly exists. Until further evidence becomes available, routine resurfacing of the patella is recommended. Table 89-5 provides a summary of recommendations.
| STATEMENT | LEVEL OF EVIDENCE/GRADE OF RECOMMENDATION | REFERENCES |
|---|---|---|
1 Feller JA, Bartlett RJ, Lang DM. Patellar resurfacing versus retention in total knee arthroplasty. J Bone Joint Surg Br. 1996;2:226.
2 Bourne RB, Rorabeck CH, Vaz M, et al. Resurfacing versus not resurfacing the patella during total knee replacement. Clin Orthop Relat Res.; 321; 1995; 156.
3 Mayman D, Bourne RB, Rorabeck CH, et al. Resurfacing versus not resurfacing the patella in total knee arthroplasty: 8- to 10-year results. J Arthroplasty. 2003;5:541.
4 Burnett RS, Haydon CM, Rorabeck CH, et al. Patella resurfacing versus nonresurfacing in total knee arthroplasty: Results of a randomized controlled clinical trial at a minimum of 10 years’ followup. Clin Orthop Relat Res.; 428; 2004; 12.
5 Keblish PA, Varma AK, Greenwald AS. Patellar resurfacing or retention in total knee arthroplasty. A prospective study of patients with bilateral replacements. J Bone Joint Surg Br. 1994;6:930.
6 Barrack RL, Wolfe MW, Waldman DA, et al. Resurfacing of the patella in total knee arthroplasty. A prospective, randomized, double-blind study. J Bone Joint Surg Am. 1997;8:1121.
6a Barrack RL, Bertot AJ, Wolfe MW, et al. Patellar resurfacing in total knee arthroplasty. A prospective, randomized, double-blind study with five to seven years of follow-up. J Bone Joint Surg Am. 2001;9:1376-1381.
7 Peng CW, Tay BK, Lee BP. Prospective trial of resurfaced patella versus non-resurfaced patella in simultaneous bilateral total knee replacement. Singapore Med J. 2003;7:347.
8 Campbell DG, Duncan WW, Ashworth M, et al. Patellar resurfacing in total knee replacement: A ten-year randomised prospective trial. J Bone Joint Surg Br. 2006;6:734.
9 Schroeder-Boersch H, Scheller G, Fischer J, et al. Advantages of patellar resurfacing in total knee arthroplasty. Two-year results of a prospective randomized study. Arch Orthop Trauma Surg. 1998;1-2:73.
10 Newman JH, Ackroyd CE, Shah NA, et al. Should the patella be resurfaced during total knee replacement? Knee. 2000;1:17.
11 Wood DJ, Smith AJ, Collopy D, et al. Patellar resurfacing in total knee arthroplasty: A prospective, randomized trial. J Bone Joint Surg Am. 2002;2:187.
12 Waters TS, Bentley G. Patellar resurfacing in total knee arthroplasty. A prospective, randomized study. J Bone Joint Surg Am. 2003;2:212.
13 Forster MC. Patellar resurfacing in total knee arthroplasty for osteoarthritis: A systematic review. Knee. 2004;6:427.
14 Pakos EE, Ntzani EE, Trikalinos TA. Patellar resurfacing in total knee arthroplasty. A meta-analysis. J Bone Joint Surg Am. 2005;7:1438.
15 Nizard RS, Biau D, Porcher R, et al. A meta-analysis of patellar replacement in total knee arthroplasty. Clin Orthop Relat Res. 2005;432:196.
16 Parvizi J, Rapuri VR, Saleh KJ, et al. Failure to resurface the patella during total knee arthroplasty may result in more knee pain and secondary surgery. Clin Orthop Relat Res.; 438; 2005; 191-196.
17 Tabutin J, Banon F, Catonne Y, et al. Should we resurface the patella in total knee replacement? Experience with the Nex Gen prothesis. Knee Surg Sports Traumatol Arthrosc. 2005;7:534.
18 Boyd ADJr, Ewald FC, Thomas WH, et al. Long-term complications after total knee arthroplasty with or without resurfacing of the patella. J Bone Joint Surg Am. 1993;5:674.
19 Ewald FC, Wright RJ, Poss R, et al. Kinematic total knee arthroplasty: A 10- to 14-year prospective follow-up review. J Arthroplasty. 1999;4:473.
20 Misra AN, Smith RB, Fiddian NJ. Five year results of selective patellar resurfacing in cruciate sparing total knee replacements. Knee. 2003;2:199.
21 Arbuthnot JE, McNicholas MJ, McGurty DW, et al. Total knee replacement and patellofemoral pain. Surgeon. 2004;4:230.