2 Shock
Classification of Shock
Septic Shock
Sepsis is defined as the presence of the systemic inflammatory response syndrome (SIRS) caused by a presumed or confirmed infection (Box 2-1). Sepsis may occur because of bacterial, viral, fungal, or parasitic infections. Septic shock is defined as sepsis and cardiovascular dysfunction. Classifying septic shock may be difficult because of the developmental variability in physiologic response to sepsis. A clinical picture consistent with hypovolemic, distributive, or cardiogenic shock may be present in a child with sepsis. Additionally, studies have demonstrated that the cardiovascular pathophysiology of children with sepsis can evolve over time, and the adjustment of hemodynamic therapy is commonly necessary.
Box 2-1
Systemic Inflammatory Response Syndrome Criteria
Adapted from American Academy of Pediatrics and American Heart Association. Pediatric Advanced Life Support. Dallas, 2006, AHA.
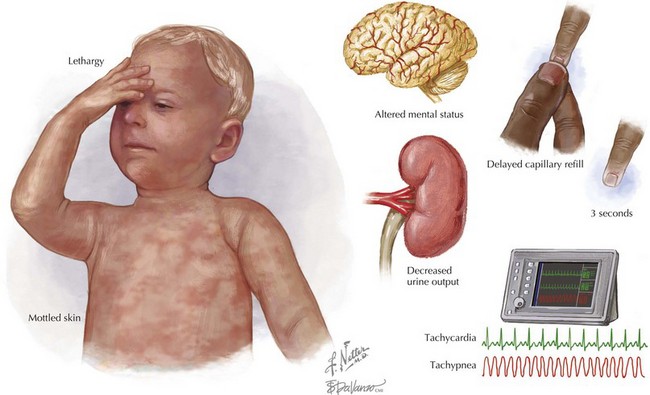
Clinical Manifestations and Evaluation
Shock remains a clinical diagnosis (Figure 2-1). Early recognition of the clinical signs of shock (including familiarity with normal ranges for vital signs by age; see Chapter 1) should lead to directed management. An accurate history should be obtained from the family and, if possible, the child, simultaneously with treatment initiation.
Management
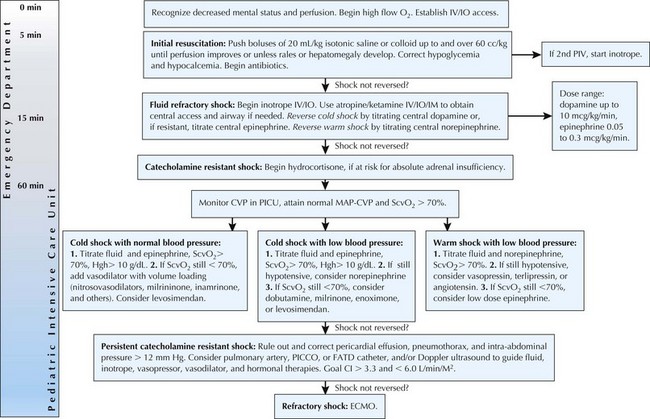
General Principles
Early recognition of compensated shock is critical to ensuring appropriate and expedient therapy. Initial therapy of shock is universal, regardless of the cause of the shock state, with the goals of optimizing blood oxygen content, improving cardiac output, reducing oxygen demand, and correcting metabolic abnormalities (Figure 2-2). General principles of resuscitation should be applied immediately on presentation to medical care (see Chapter 1). Ultimately, after initial management has commenced, correction of the underlying cause is essential (e.g., stopping blood loss in hemorrhagic shock, antibiotics for shock caused by bacterial infection).
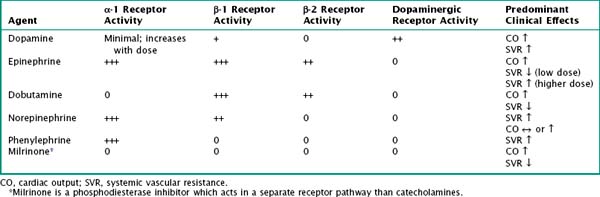
Circulatory Support
Table 2-1 outlines commonly used vasoactive agents, their targeted receptors, and their hemodynamic effects. Data are varied on the choice of initial agent; current recommendations from the American College of Critical Care Medicine state that dopamine, epinephrine, or norepinephrine may be appropriate first-line therapy for septic shock, provided they are administered through a central venous catheter. Dopamine or low-dose epinephrine may be given via a peripheral vein while central venous access is obtained.
Special Circumstances: Shock in Neonates
When faced with a neonate with shock, early consideration should be given to ductal-dependent congenital heart disease. Lesions marked by ductal-dependent systemic blood flow, such as aortic stenosis, hypoplastic left heart syndrome, coarctation of the aorta, and interrupted aortic arch, may present as shock in the neonatal period (see Chapter 44). Infants with these lesions depend on blood flow from the pulmonary artery across the ductus arteriosus into the aorta for perfusion of all or part of the systemic circulation. Although this is deoxygenated blood, the oxygen content is sufficient to meet the metabolic demands of the tissues. Therefore, when the ductus arteriosus closes, circulatory failure and tissue hypoxia occur.
American College of Surgeons Committee on Trauma. Advanced Trauma Life Support for Doctors (ATLS), 8th ed. Chicago: American College of Surgeons; 2008.
American Heart Association. Pediatric Advanced Life Support (PALS) Provider Manual. Dallas: American Heart Association Publications; 2006.
Bell L. Shock. In: Fleisher G, Ludwig S, editors. Textbook of Pediatric Emergency Medicine. ed 6. Philadelphia: Lippincott Williams & Wilkins; 2010:46-57.
Brierley J, Carcillo JA, Choong K, et al. Clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock: 2007 update from the American. Crit Care Med. 2009;37(2):666-688.
Ceneviva G, Paschall JA, Maffei F, Carcillo JA. Hemodynamic support in fluid-refractory pediatric septic shock. Pediatrics. 1998;102(2):e19.
Goldstein B, Giroir B, Randolph A. Pediatric sepsis consensus conference: definitions of sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005;6(1):2-8.
McKiernan C, Lieberman S. Circulatory shock in children: an overview. Pediatr Rev. 2005;26:451-460.
Rivers E, Nguyen B, Havstad S, Ressler J, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368-1377.