Chapter 27 Sexuality and Female Sexual Dysfunction
 Variation in Sexual Expression
Variation in Sexual Expression
Transgender or transsexual individuals are often confused with homosexuals. They have a strong belief from childhood that they were born into a body with the wrong sex. Most are heterosexual to their identified gender (i.e., men who believe they are women are attracted to men), and few are homosexual. Children with ambiguous genitalia who are assigned a particular gender may later show regret toward their assignment. Some experts recommend that these children be given a name that is appropriate to both genders to allow them to decide their gender for themselves later in life. Female-to-male transsexuals (FTM) are women that grow up as “tomboys” and often cross-dress. Male-to-female transsexuals (MTF) are men that grow up dressing as women. Transgender surgery is difficult to perform, especially FTM, and it is only performed in certain areas of the United States and the world. Box 27-1 lists some other variations in human sexual expression along with their definitions.
BOX 27-1 Other Forms of Sexual Expression and Their Definitions
 Sexual Response
Sexual Response
FEMALE SEXUAL RESPONSE CYCLE
The Excitement Phase
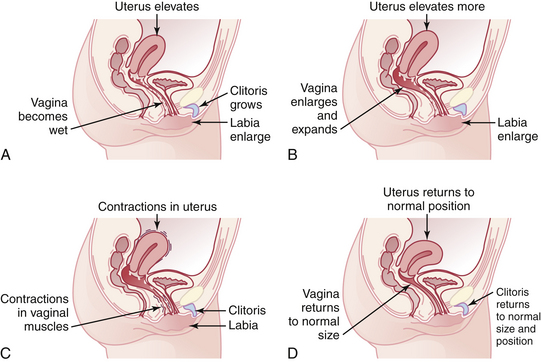
This phase starts with physical or psychological stimulation and may last minutes or hours. There is a sex flush, accompanied by erection of the nipples and engorgement of the breasts. A sex flush is an erythematous morbilliform skin change over the chest, neck, and face that occurs to a noticeable degree in 75% of women. In addition, the uterus elevates, and vaginal lubrication begins. The clitoris and labia enlarge, and the heart rate and blood pressure increase. Most muscles become tense (Figure 27-1A).
The Plateau Phase
During this phase, the breasts continue to enlarge, and the clitoris may elevate and retract under its hood. The Bartholin’s glands may secrete fluid near the vaginal opening, and there is tenting of the uterus to allow easier passage of sperm. The vagina and labia become more engorged, and there is increased blood pressure, heart rate, respiratory rate, and muscle tension (see Figure 27-1B).
The Orgasmic Phase
During this phase, there is release of sexual tension. The orgasmic phase is possible without actual physical stimulation. This phase is concentrated in the clitoris, vagina, and uterus. There is contraction of vaginal, uterine, lower abdominal, and anal muscles, usually 5 to 12 synchronized contractions 1 second apart. The first few contractions are the strongest and the closest together. Blood pressure, heart rate, and respiratory rate peak in this phase, and there is usually loss of voluntary muscle tone (e.g., most women curl their toes at orgasm). Women can have multiple orgasms before they enter the resolution phase (see Figure 27-1C).
MALE SEXUAL RESPONSE CYCLE
The Excitement Phase
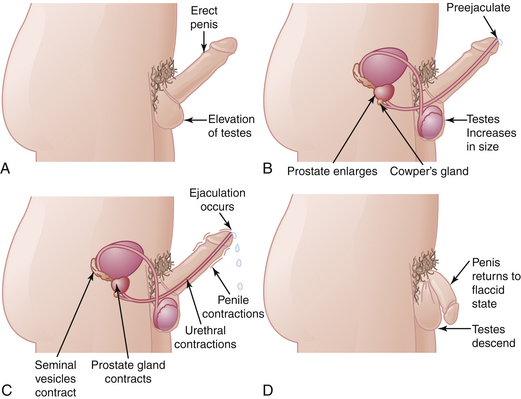
This phase begins with physical or psychological stimulation and may last minutes or hours. The nipples and penis become erect, and there is increased heart rate and blood pressure. The muscles become tense, and there is blood pooling in the extremities with vasocongestion in the penis and scrotum with testicular swelling and elevation (Figure 27-2A).
The Plateau Phase
The testicles enlarge by 50%, and the prostate and penis also enlarge. There is increased blood flow, and the bulbourethral or Cowper’s gland secretes pre-ejaculatory fluid, which may contain sperm. There is increased blood pressure, heart rate, respiratory rate, and muscle tension. There is generally chest sex flushing (see Figure 27-2B).
The Orgasmic Phase
During the orgasmic phase, there is release of sexual tension; this phase is possible without actual physical stimulation. There are rhythmic contractions of the seminal vesicles, vas deferens, and prostate. The ejaculatory ducts push semen into the urethra, and ejaculation occurs with urethral contractions. The first few contractions are the strongest and the closest together. During this phase, the anal sphincter contracts. The point of imminence occurs a few seconds before ejaculation and refers to the point when a man knows an orgasm is inevitable (see Figure 27-2C).
The Resolution Phase
In the resolution phase, the genitals and penis decrease in size and return to a flaccid state. The testes descend, and the sex flush disappears. The blood pressure, heart rate, and respiratory rate return to normal (see Figure 27-2D).
 Sexual Dysfunction
Sexual Dysfunction
EVALUATION OF SEXUAL FUNCTION
FEMALE SEXUAL DYSFUNCTION
Sexual dysfunction is categorized by the Sexual Function Health Council of the American Foundation of Urologic Disease by failure of one or more of the phases of the sexual response cycle. Sexual dysfunction also includes pain disorders (Box 27-2).
ETIOLOGY OF SEXUAL DYSFUNCTION
As a general rule, primary problems are predominantly psychogenic and tend to be of longer duration. Secondary problems are often associated with the onset of a disease process or the use of a pharmacologic agent. If such an association cannot be established, deterioration in the patient’s relationship or some other chronologically related change in the patient’s life experience should be sought. It is important to consider psychological causes, such as depression or anxiety; organic causes, such as atherosclerosis, diabetes, or genital infections; and pharmacologic causes (Box 27-3). Factors initiating a problem may be different from those maintaining it. For example, drugs may precipitate a problem, but if anxiety and fear of failure sustain the difficulty, discontinuation of the drug alone may not rectify the problem.
SEXUAL FUNCTION DISORDERS
Berman J.R., Goldstein I. Female sexual dysfunction. Urol Clin North Am. 2001;28:405-416.
Esposito K., Giugliano F., Ciotola M., et al Obesity and sexual dysfunction, male and female Jul-Aug. Int J Impot Res, 20(4); 2008:358-365. Epub 2008: April 10
Frank J.E., Mistretta P., Will J. Diagnosis and treatment of female sexual dysfunction. Am Fam Physician. 2008;77:635-642.
Hayes R.D., Dennerstein L., Bennett C.M., et al. Risk factors for female sexual dysfunction in the general population: Exploring factors associated with low sexual function and sexual distress. J Sex Med. 2008;5(7):1694-1701. Jul
Palha A.P., Esteves M. Drugs of abuse and sexual functioning. Adv Psychosom Med. 2008;29:131-149.

 Sexual Development
Sexual Development