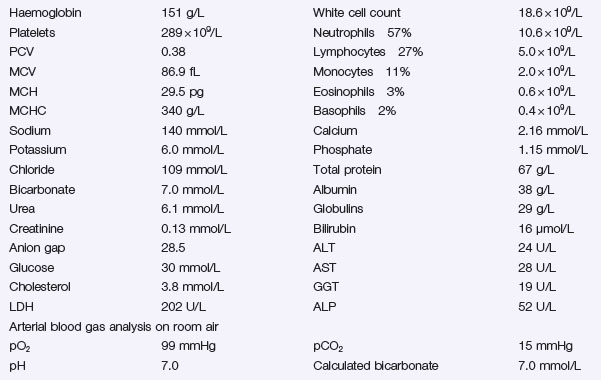
Problem 48 Severe dehydration in a young woman
There are a number of possible causes for this woman’s comatose state.
You have a working diagnosis for this patient who is critically ill.
The patient decides to curtail her backpacking holiday and return home.
Answers
A.1 Her Glasgow coma score is 11 (E4, V2, M5).
A.3 As part of the immediate management, the following must be undertaken:
Metabolic acidosis can be divided into:
Fluid and Sodium Replacement
Correction of Acidosis and Hyperglycaemia with Insulin
Insulin therapy will correct both the acidosis and hyperglycaemia.
Potassium Replacement
Prevention of the Complications of Ketoacidosis
Insulin infusion is ceased 1 hour after the first dose of subcutaneous insulin is given.
In Hospital:
As an Outpatient
Revision Points
Diabetic Ketoacidosis
Treatment
Intravenous insulin infusion allows a gradual and steady correction of the metabolic abnormalities.