Sensation
What You Find and What It Means
WHAT YOU FIND
Patterns of sensory loss
Sensory deficits (Fig. 22.1) can be classified into eight levels of the nervous system:
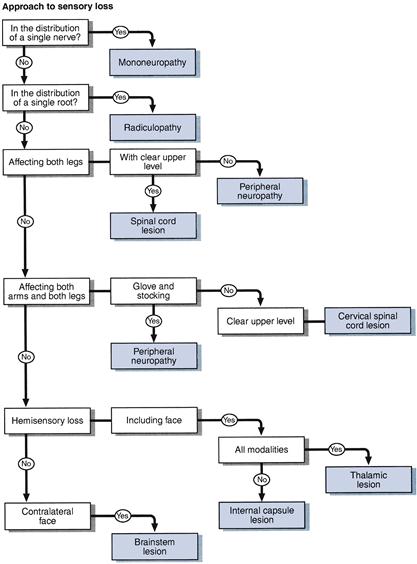
Figure 22.1 Simplified approach to sensory loss
1. Single nerve: sensory loss within the distribution of a single nerve, most commonly median, ulnar, peroneal, lateral cutaneous nerve to the thigh. Distributions are illustrated in Chapter 21.
2. Root or roots: sensory deficit confined to a single root or a number of roots in close proximity—common roots in the arm C5, C6 and C7 and in the leg L4, L5 and S1. Distributions are illustrated in Chapter 21. When multiple nerve roots are involved in the lumbosacral spine (usually S1–S5 roots bilaterally), this results in a cauda equina syndrome with sensory loss in the perianal region and buttocks (saddle anaesthesiae) and the back of both thighs.
3. Peripheral nerve: distal glove and stocking deficit (Fig. 22.2).

Figure 22.2 Glove and stocking loss
4. Spinal cord: five patterns of loss can be recognised (Fig. 22.3):
• Complete transverse lesion: hyperaesthesia (increased appreciation of touch/pinprick) at the upper level, with loss of all modalities a few segments below the lesion (Fig. 22.3A).
• Hemisection of the cord (Brown–Séquard syndrome): loss of joint position sense and vibration sense on the same side as the lesion and pain and temperature on the opposite side a few levels below the lesion (Fig. 22.3B).
• Central cord: loss of pain and temperature sensation at the level of the lesion, where the spinothalamic fibres cross in the cord, with other modalities preserved (dissociated sensory loss)—seen in syringomyelia (Fig. 22.3C).
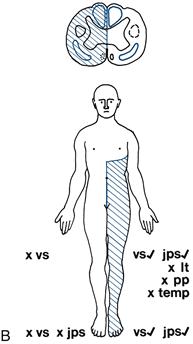
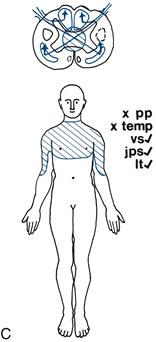
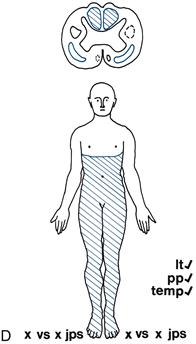
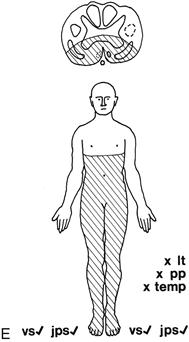
Figure 22.3 B,C,D,E B. Hemisection of the cord C. Central cord lesion. D. Posterior column loss. E. Anterior spinal syndrome
• Posterior column loss: loss of joint position sense and vibration sense with intact pain and temperature (Fig. 22.3D).
• Anterior spinal syndrome: loss of pain and temperature below the level, with preserved joint position sense and vibration sense (Fig. 22.3E).
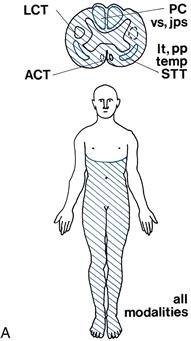
Figure 22.3A Sensory loss associated with spinal cord lesions: A. Complete transverse lesion.
Legend for Figure 22.3 A-G Cross-section of spinal cord: these are the same as in Figure 21.1, with the lesions shaded in blue. LCT, lateral corticospinal tract; ACT, anterior corticospinal tract; PC, posterior column; STT, spinothalamic tract
Sensory modalities: areas of sensory loss are shaded in blue. Modalities are marked: x, absent; tick, present. pp, pinprick; temp, temperature; vs, vibration sense; jps, joint position sense; lt, light touch
5. Brainstem: loss of pain and temperature on the face and on the opposite side of the body. Common cause: lateral medullary syndrome (Fig. 22.3F).
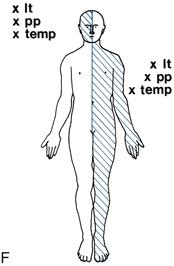
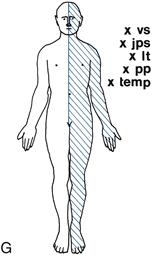
Figure 22.3F,G F. Brainstem lesion. G. Thalamic sensory loss
6. Thalamic sensory loss: hemisensory loss of all modalities (Fig. 22.3G).
WHAT IT MEANS
Interpretation of the sensory findings depends on integrating them with the results of other parts of the neurological examination, especially the motor examination.
• Single nerve lesion. Common cause: entrapment neuropathy. More common in diabetes mellitus, rheumatoid arthritis, hypothyroidism. May be presentation of more diffuse neuropathy (see Chapter 20).
• Cauda equina syndrome (see also Chapter 26). Common cause: compression of cauda equina by prolapsed intervertebral disc. Rare causes: tumours or herpes simplex polyradiculitis.
• Peripheral nerve (see Chapter 20). Common causes: diabetes mellitus, alcohol-related vitamin B1 deficiency, drugs (e.g. vincristine); frequently no cause is found. Rarer causes: Guillain–Barré syndrome, inherited neuropathies (e.g. Charcot–Marie–Tooth disease), vasculitis, other vitamin deficiencies, including vitamin B12.
– Hemisection. Common causes: as for transection.
– Central cord syndrome (rare). Common causes: syringomyelia, trauma leading to haematomyelia.
– Anterior spinal syndrome (rare): anterior spinal artery emboli or thrombosis.
• Functional: may indicate conversion disorder. N.B. This is a difficult diagnosis to make.

 TIP
TIP