CHAPTER 22 Seizure Disorders
I. Introduction/Definitions
A. Seizure: A seizure occurs when these neurons generate electrical discharges that spread throughout the brain. This can occur with both normal and abnormal nerve cells.
B. Epilepsy: Epilepsy is a group of disorders characterized by recurrent seizures. In epilepsy, brain cells (neurons) create abnormal electricity that causes seizures or jerking movements. In some cases, seizures cause a loss of consciousness, a period of confusion, a staring spell, or muscle spasms. A single seizure is not considered epilepsy. Individuals with epilepsy have repeated episodes of seizures. Different forms of epilepsy are either secondary to a particular brain abnormality or neurological disorder or are said to be idiopathic (without any clear cause).
II. Types of Seizures
A. Partial seizures
2. They may be further divided into simple partial and complex partial
B. Generalized seizures
1. Involve larger areas of the brain, often both hemispheres (sides), from the onset. They are further divided into many subtypes. The more common types include tonic-clonic (grand mal), absence (petit mal), and myoclonic seizures.
a. Tonic-clonic (grand mal)
2) Sustained muscle contraction (tonic), followed by alternating muscle contractions and relaxation (clonic)
b. Absence (petit mal)
III. Signs and Symptoms
A. Symptoms vary depending on the type of seizure
1. Partial seizure
2. Generalized seizure
a. Absence seizures (petit mal): characterized by staring, subtle body movements, and brief lapses of awareness
b. Tonic-clonic seizures (grand mal): most common form of generalized seizures. They are also the most widely recognized epileptic seizure. In a tonic-clonic seizure, the person loses consciousness, the body stiffens, and the person falls to the ground. This is followed by jerking movements. After a minute or two, the jerking movements usually stop and consciousness slowly returns.
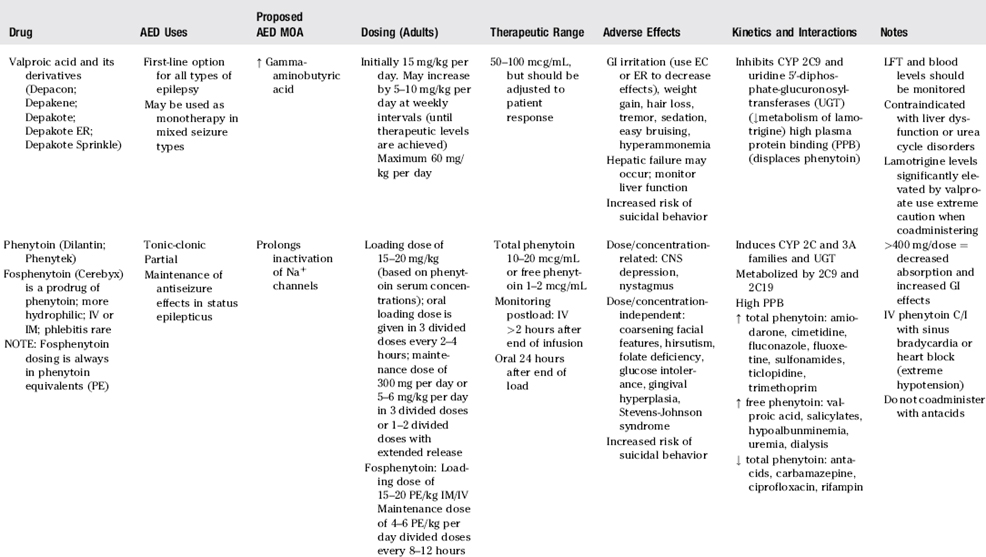
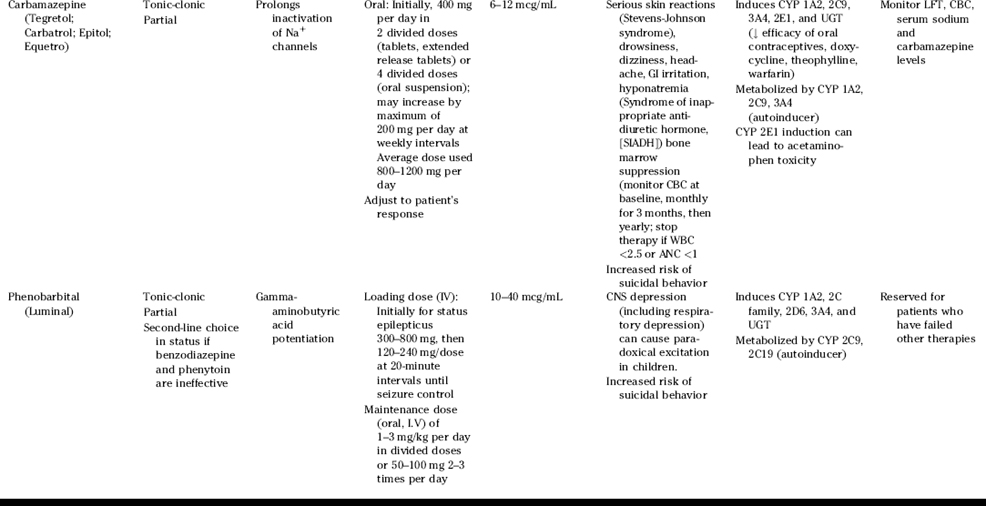
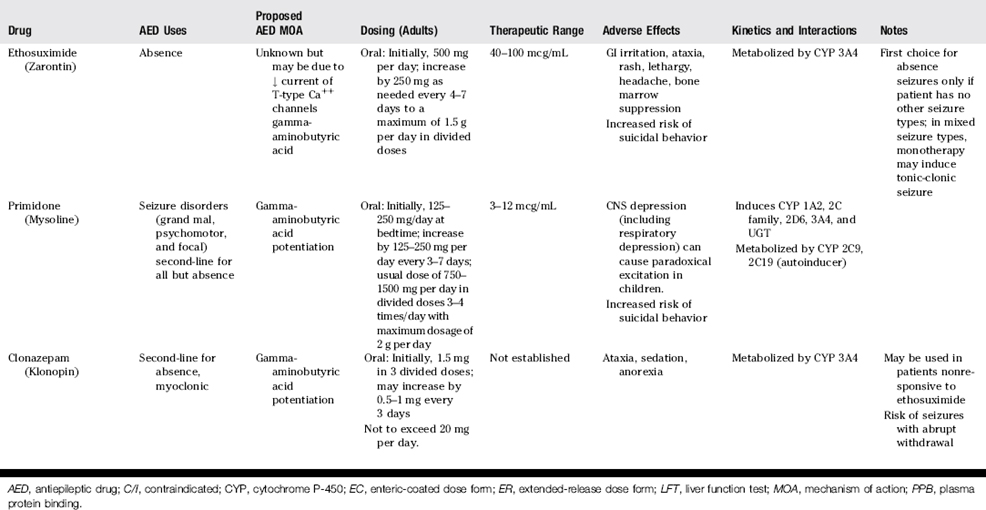
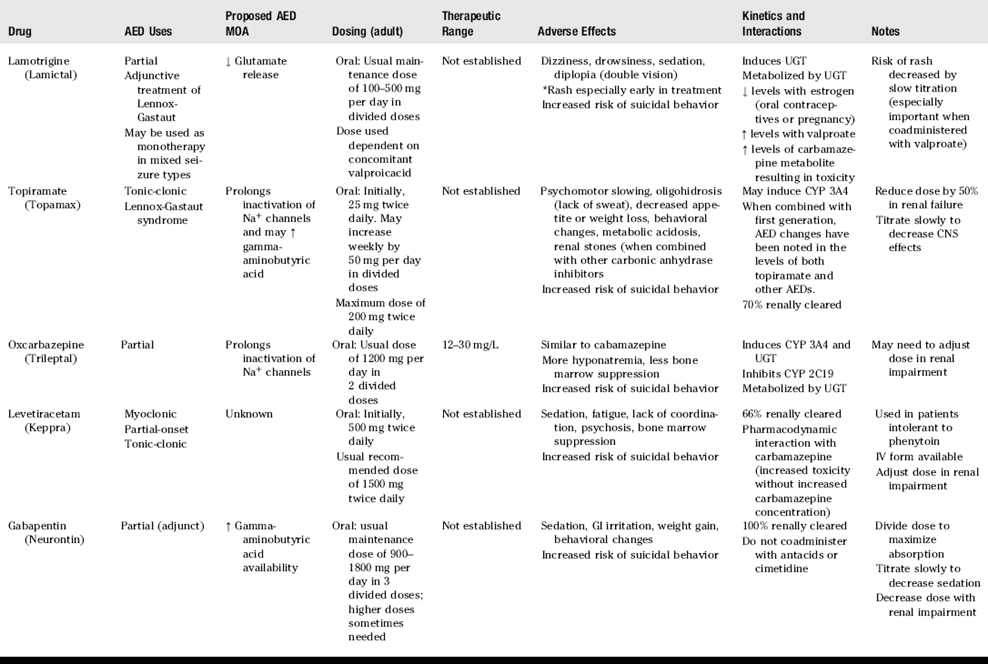
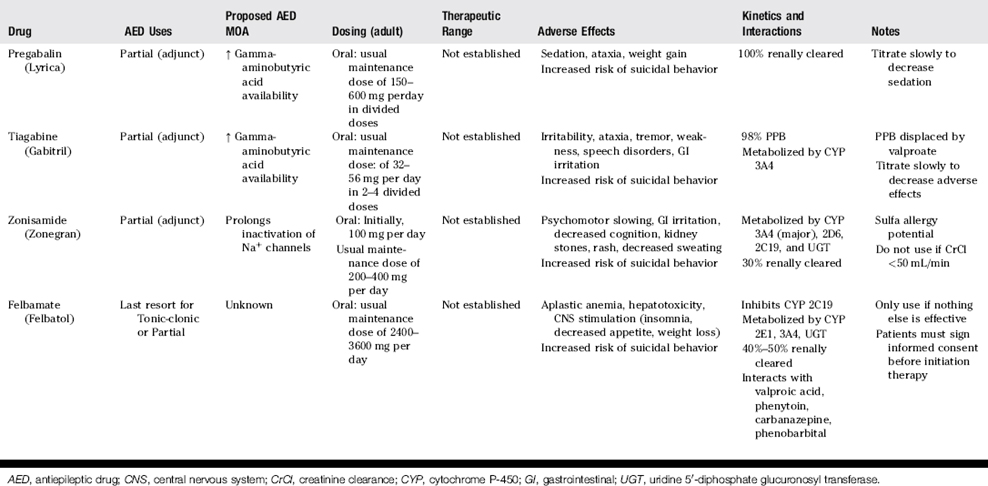
IV. Treatment (Tables 22-1 and 22-2)
A. Anticonvulsant medications are the treatment choice for epilepsy and seizure disorders. Treatment with one anticonvulsant agent is the goal, if possible.
B. When initiating therapy for epilepsy, drugs should be chosen based on seizure type(s) and drug side effect profiles.
C. AED and oral contraceptives
1. Many AED induce the metabolism of estrogen. If breakthrough bleeding occurs, the ethinyl estradiol component of the oral contraceptive should be increased to 50 mcg/day per active pill.
V. Medications Associated with Decreasing Seizure Threshold
C. Antimicrobials/antivirals: in general, seizures are more likely with these agents when dosage adjustments are not made for renal impairment or other clinical parameters (e.g., imipenem, penicillins)
VI. Status Epilepticus
B. Prolonged, repetitive seizure activity that lasts more than 20–30 minutes, during which time the patient is unconscious. Status epilepticus is a medical emergency with a significantly poor outcome. It can result in death if not treated aggressively. Its causes include improper use of certain medications, stroke, infection, trauma, cardiac arrest, illicit drug overdose (such as cocaine or methamphetamine), and brain tumor.
C. Treatment: The goal of treatment always should be immediate diagnosis and termination of seizures. For an AED to be effective in status epilepticus, the drug must be administered intravenously (or rectally, as with diazepam, if IV access not immediately accessible) to provide quick access to the CNS without the risk of serious systemic and neurologic adverse effects.
PATIENT PROFILE
Current medical problem: BM is sent to the hospital by his neurologist due to complaints of increasing seizure frequency over the past week despite stated compliance with his medication. His phenytoin level on admission is 5 mcg/mL. While he is in the emergency department, he has another seizure.
PATIENT PROFILE QUESTIONS
1. After an initial dose of lorazepam 4 mg IV, the emergency physician orders fosphenytoin 100 mg phenytoin equivalents (PE) to be given immediately in the emergency department to help raise the phenytoin level to the appropriate range (10–20 mcg/mL). The pharmacist prepares a standard intravenous infusion containing 25 mg PE per mL of fosphenytoin. If the infusion should be given no faster than 150 PE/min, how many milliliters can be given in 1 minute to deliver the dose safely, but quickly?
2. Once the patient is stabilized on the neurology unit, the neurologist decides to add carbamazepine to the existing phenytoin regimen. His phenytoin level is now 13 mcg/mL. Carbamazepine suspension is ordered with an initial dose of 200 mg PO twice daily. What are appropriate instructions to the nursing staff?
3. After several days, the neurologist is ready to send BM home. He changes the prescription of carbamazepine suspension to tablets. What is the appropriate dosage adjustment for the change in dosage forms?
4. At discharge, BM’s carbamazepine level is 9 mcg/mL. Four weeks later, BM has a seizure, and a repeat drug concentration panel reveals his phenytoin level is 13 mcg/mL and his carbamazepine level is 4 mcg/mL. A review of the pharmacy profile and a discussion with his mother reveals that the patient appears to have been compliant with his medications. What is the most likely reason for the change in carbamazepine concentrations?
REVIEW QUESTIONS
(Answers and Rationales on page 377.)
4. A 7-year-old girl is diagnosed with absence seizures. Which of the following is the most appropriate initial therapy?
13. Which of the following statements is true regarding drug interactions of anti-seizure medications?
17. Which of the following is the appropriate laboratory parameter to evaluate for phenytoin toxicity?
19. What is the appropriate initial management of a patient presenting with acute barbituate overdose?
20. Which of the following seizures varies in presentation depending on which part of the cortex is affected, lasts between 20-60 seconds, and does not impair the patient?s state of consciousness?
23. A patient with asthma is taking prednisone for a recent exacerbation. For a newly diagnosed seizure disorder, she is started on phenytoin. Two weeks later, she returns to the clinic and complains of increased asthma symptoms. What is the likely mechanism?