SEIZURE
A seizure (“fit”; epilepsy) represents vigorous involuntary muscle activity and altered consciousness associated with abnormal electrical discharges within the brain. It may be caused by a number of underlying disorders, which include structural abnormalities of the brain (scars, birth defects), injury, tumor, infection, bleeding (stroke), uncontrolled hypertension, lack of oxygen, abnormal blood chemistries (calcium, sodium, glucose), and “recreational” drug abuse (including drug or alcohol withdrawal).
Most seizures have been grouped into various classifications, which include the following types:
Partial. This seizure is initiated in a focal, or “restricted,” part of the outermost layer (cortex) of the brain. Consciousness may (complex seizure) or may not (simple seizure) be impaired.
Generalized. This seizure involves the cortex of the brain in a symmetrical and synchronous manner, and may lead to “automatic,” “absent,” or profoundly agitated behavior patterns.
Grand mal (“big illness”). In this type of generalized seizure disorder, the victim classically becomes unconscious and has violent repetitive muscle activity with tongue biting, grunting, eye deviation to one side, difficulty breathing, and occasional loss of bladder or bowel control. Following the seizure, the victim will be confused or combative for a time (10 to 60 minutes) as he slowly returns to normal. He may sleep for a while after a seizure.
Status epilepticus. This is defined as prolongation of the seizure activity for a period that exceeds 1 to 2 minutes, or as multiple seizures without a return of normal consciousness between fits. Status epilepticus is a true medical emergency.
Petit mal (“little illness”). This is an “absence” attack generally seen in a child; in it, he seems to be daydreaming, distracted, or confused. It is not associated with violent, abnormal physical behavior.
Psychomotor (temporal lobe). This is an episode of patterned abnormal behavior, such as lip smacking, olfactory hallucinations, vulgar speech, or repetitive movements such as arm waving. The origin of the electrical activity is thought to reside in the temporal lobe of the brain.
TREATMENT FOR SEIZURE
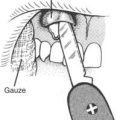
1. Protect the airway (see page 22). If the victim vomits, do your best to clear the mouth and nose of debris. Turn the victim on his side. He may suddenly bite down and hold his teeth clenched, so take care not to get your fingers caught in the mouth. A padded object that cannot be bitten through (such as a leather wallet edge) may be used as a bite block to keep the teeth apart and prevent tongue biting, but take extreme care not to obstruct the airway. Do not place a hard object in the mouth that might break the teeth. Take care not to force the tongue backward into the throat. Never try to pour liquids into the mouth of a seizing victim.
2. Protect the cervical spine (see page 37).
3. Protect the victim from injuring himself during the seizure. This may be done with cushions, a sleeping bag, or constant repositioning of the victim. If he needs to be physically restrained, keep him on his side. Loosen all clothing around the neck.
4. In most cases, a grand mal seizure will only last 30 seconds to 2 minutes and will be self-limited. The victim will be confused for a few minutes to an hour after the seizure, and should be watched closely for recurrence or difficulty in breathing. If the victim continues to seize or does not wake up between seizures (status epilepticus), he must be transported to a medical facility as soon as possible for drug administration. Any victim who does not fully awaken, who awakens but has never previously had a seizure, or who appears weak or feverish after a seizure should be rapidly evacuated.
5. When the victim awakens, determine if he has ever had a seizure before and whether he is supposed to be taking anticonvulsants. The most common cause of a seizure is failure to take prescribed antiseizure medication(s). If the victim has been delinquent, he should take his medicine as soon as possible. For an adult, common medications are phenytoin sodium (Dilantin) 300 to 400 mg per day, phenobarbital 30 to 60 mg three times a day, or diazepam (Valium) 5 to 10 mg three to four times a day. Never administer an oral medication to anyone unless he is awake and capable of purposeful swallowing.
6. A possible cause of unconsciousness or seizure in a person who suffers from diabetes is low blood sugar (hypoglycemia). If a diabetic suffers a seizure, he should be given sugar as soon as possible. This may be difficult to do away from the hospital, because intravenous injection will be required if the victim cannot swallow. If a diabetic feels weak, sweaty, dizzy, or nauseated, he should immediately ingest a sugar-containing beverage, food (see page 142), or concentrated liquid glucose (Glutose: one tube contains 25 g). If the victim is unconscious, sugar granules or small squirts of Glutose can be placed under the tongue, where they can be passively swallowed.