Sebaceous and sweat glands – Acne, rosacea and other disorders
Acne
 increased sebum excretion – seborrhoea (greasy skin)
increased sebum excretion – seborrhoea (greasy skin)
 pilosebaceous duct hyperkeratosis and comedone formation
pilosebaceous duct hyperkeratosis and comedone formation
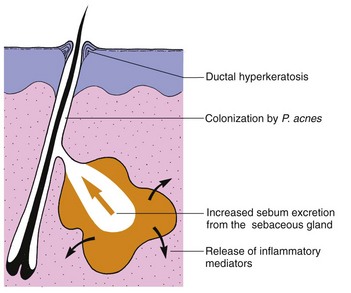
In acne, the androgen-sensitive pilosebaceous unit (p. 4) shows a hyper-responsiveness that results in increased sebum excretion. Factors in sebum induce comedones, and P. acnes initiates inflammation through chemical mediators inducing enzymes (e.g. lipase) and prostaglandins (Fig. 1).
Clinical presentation
Comedones are either open (blackheads: dilated pores with black plugs of melanin-containing keratin) or closed (whiteheads: small cream-coloured, dome-shaped papules). They appear at about the age of 12 years and evolve into inflammatory papules (Fig. 2), pustules or cysts (Fig. 3). The sites of predilection – the face, shoulders, back and upper chest – have many sebaceous glands. The severity of acne depends on its extent and the type of lesion, with cysts being the most destructive.
Acne usually persists until the early twenties, although in a few patients, particularly women, the disease continues into the fifth decade. Scars may follow healing, especially of cysts or abscesses. Scars may be ‘ice-pick’, atrophic (Fig. 4) or keloidal.
Some variants of acne are seen:
 Acné excoriée: due to squeezing, affects depressed or obsessional young women.
Acné excoriée: due to squeezing, affects depressed or obsessional young women.
 Chloracne: caused by systemic toxicity of certain aromatic halogenated industrial chemicals.
Chloracne: caused by systemic toxicity of certain aromatic halogenated industrial chemicals.
 Conglobate: a mass of burrowing abscesses and sinuses with scarring.
Conglobate: a mass of burrowing abscesses and sinuses with scarring.
 Cosmetic: pomade and cosmetic-induced comedonal and papular acne (mainly seen in the USA).
Cosmetic: pomade and cosmetic-induced comedonal and papular acne (mainly seen in the USA).
 Drug-induced: by systemic steroids, androgens and topical steroids.
Drug-induced: by systemic steroids, androgens and topical steroids.
 Infantile: mostly found on the faces of male infants; cause unknown.
Infantile: mostly found on the faces of male infants; cause unknown.
 Physical: occlusion by the back of a wheelchair or on a violinist’s chin.
Physical: occlusion by the back of a wheelchair or on a violinist’s chin.
Management
Local treatment is adequate for mild acne and is used with systemic drugs for more severe cases.
 Benzoyl peroxide (Panoxyl, Brevoxyl) cream or gel, applied twice a day, works by reducing the number of P. acnes. It may cause irritation, contact allergy and bleach clothing.
Benzoyl peroxide (Panoxyl, Brevoxyl) cream or gel, applied twice a day, works by reducing the number of P. acnes. It may cause irritation, contact allergy and bleach clothing.
 Tretinoin (Retin-A gel) is good at reducing the number of comedones, but may be irritant.
Tretinoin (Retin-A gel) is good at reducing the number of comedones, but may be irritant.
 Antibiotics, e.g. clindamycin alone (Dalacin T) or with benzoyl peroxide (Duac), erythromycin alone (Stiemycin) or with zinc (Zineryt), can be used for mild or moderately severe acne.
Antibiotics, e.g. clindamycin alone (Dalacin T) or with benzoyl peroxide (Duac), erythromycin alone (Stiemycin) or with zinc (Zineryt), can be used for mild or moderately severe acne.
 Other topical agents, e.g. azelaic acid, isotretinoin and adapalene.
Other topical agents, e.g. azelaic acid, isotretinoin and adapalene.
Rosacea
Clinical presentation
Rosacea has an equal sex incidence. Although commonest in middle age, it also affects young adults and the elderly. The earliest symptom is flushing. Erythema, telangiectasia, papules, pustules (Fig. 5) and, occasionally, lymphoedema involve the cheeks, nose, forehead and chin. Rhinophyma, hyperplasia of the sebaceous glands and connective tissue of the nose (Fig. 5), and eye involvement by blepharitis and conjunctivitis are complications. Sunlight and topical steroids exacerbate the condition. Rosacea persists for years, but usually responds well to treatment. Rosacea lacks the comedones of acne and occurs in an older age group. Contact dermatitis, photosensitive eruptions, seborrhoeic dermatitis and lupus erythematosus often involve the face but are more acute or scaly, or lack pustules.
Other disorders
Hidradenitis suppurativa is an unpleasant chronic inflammatory condition of the infundibulum of hair follicles (p. 4) in the apocrine sweat gland areas of the axillae, groin and perineum. Nodules, abscesses, cysts and sinuses form and scarring results (p. 114). Treatment is with topical antiseptics, a prolonged course of a systemic antibiotic or retinoid, surgical excision or infliximab. Conglobate acne may coexist.
Hyperhidrosis (excess sweating) due to eccrine gland overactivity is usually emotional in origin. Twenty per cent aluminium chloride in alcohol is often effective. Iontophoresis is used for the hands (p. 23) and Botox injection for the axillae (p. 114).
Sebaceous and apocrine disorders
Acne
 Due to increased sebum excretion, comedone formation, P. acnes and inflammation.
Due to increased sebum excretion, comedone formation, P. acnes and inflammation.
 Presentation: comedones, pustules, cysts and scars seen over the face, chest and trunk.
Presentation: comedones, pustules, cysts and scars seen over the face, chest and trunk.
 Treatment: topical treatments include benzoyl peroxide and tretinoin; systemic treatments include antibiotics, e.g. tetracyclines or erythromycin, co-cyprindiol and isotretinoin.
Treatment: topical treatments include benzoyl peroxide and tretinoin; systemic treatments include antibiotics, e.g. tetracyclines or erythromycin, co-cyprindiol and isotretinoin.