Seasonal and Perennial Allergic Conjunctivitis
Introduction
Seasonal allergic conjunctivitis (SAC) and perennial allergic conjunctivitis (PAC) are the common and mild acute forms of ocular allergy, usually accompanied by seasonal allergic rhinitis,1 with SAC comprising 25% to 50% of the total cases of allergic conjunctivitis.2 Several authors have emphasized that ocular allergies, especially SAC, are underdiagnosed, thus underestimating their true prevalence.3 Although SAC and PAC are relatively mild conditions, rarely causing permanent visual impairment, their effects on the quality of life can be profound, with significant morbidity.4
The seasonal incidence of SAC is closely related to the cycles of released plant-derived airborne allergens, or aeroallergens. The allergens that produce SAC vary from one geographic area to another, but tree, grass, and ragweed pollens are the most common encountered allergens. PAC is more likely to occur year-round, although about 79% of patients may still have seasonal exacerbations. Some have theorized that warming trends, accompanying long-term climate change, may cause greater exposure times to seasonal allergens, with subsequent effects on allergic eye disease prevalence.5
The majority of PAC and SAC affect both young and middle-aged people of both sexes.6
Pathophysiology
Both SAC and PAC are type I (immediate) immunoglobulin E (IgE)-mediated hypersensitivity reactions, due to environmental airborne allergens, divided into two phases, with the mast cell (MC) playing a central role. A reaction occurs when a sensitized individual is exposed to a specific antigen. IgE has a strong affinity for MCs, predominantly MCTC phenotype, triggering its degranulation. The number of MCs present within the conjunctiva stroma may be increased up to 60% in patients with SAC compared to normal patients.7
The reaction involves a very complex series of immunological events, coordinated by various mediators, initiated by the allergen. An allergen such as pollen reacts with specific IgE antibodies bound to a sensitized MC, triggering cross-linkage of the IgE molecules and an influx of calcium ions into the MC. This causes the MC to degranulate and release preformed inflammatory mediators, such as histamine, which causes the signs and symptoms associated with the early-phase response in sensitized individuals. There are two components of MC activation. The first is the release of preformed mediators, including histamine. The second is the synthesis of arachidonic acid and the subsequent metabolic cascade, resulting in the production of prostaglandins and leukotrienes. The released histamine binds H1 and H2 receptors on the target tissue cell surfaces. Binding to the H1 receptor results in the primary allergic symptoms of itching, burning, and stinging sensation and tearing, while binding to the H2 receptor releases leukotrienes and prostaglandins, stimulating mucus production and also increasing vascular permeability.7 This early-phase response is immediate and lasts clinically for 20–30 minutes.
MC degranulation also initiates a series of cellular and extracellular events, which lead to the late-phase response, including production of prostaglandins, thromboxanes and leukotrienes derived from arachidonic acid.8 MCs also release cytokines and chemotactic factors which induce the production of IgE from B cells, enhance production of Th2 lymphocytes, attract eosinophils and activate vascular endothelial corneal and conjunctival cells to release chemokines and adhesion molecules. The chemokines and adhesion molecules mediate the infiltration of eosinophils, basophils, neutrophils and Th2 lymphocytes to the site of inflammation, coupled with the newly formed mediators and sustained MC activation, resulting in the late-phase response. This may occur 3–12 hours after the initial reaction, and symptoms can continue up to 24 hours.9
After the MCs are activated, cytokines are released. These cytokines attract eosinophils, lymphocytes, and neutrophils. Eosinophil infiltration of the conjunctiva is present in about 43% of patients with SAC, and about 25–84% of patients with PAC. Degranulating eosinophils release toxic proteins, including eosinophil major basic protein and eosinophil cationic protein. These proteins have cytotoxic effects and further enhance MC degranulation. These products of eosinophils are toxic to the corneal epithelium and, if present chronically, may result in ulceration. The late-phase response is characterized by an influx of multiple inflammatory cells, including eosinophils, basophils, neutrophils, and macrophages, along with CD4+ and CD8+ cells. Conjunctival epithelial cells may also prolong the allergic inflammatory response by releasing chemotactic mediators. The year-round symptoms associated with PAC are the result of chronic MC activation and Th2 lymphocyte infiltration.10,11
In summary, acute allergy is caused by IgE-mediated MC degranulation, whereas chronic allergies are also associated with continuous activation of MC but with predominance of mediators, such as eosinophils and Th2-generated cytokines.12
Clinical Findings of SAC and PAC
Individuals with SAC typically have symptoms of acute allergic conjunctivitis for a defined period of time, usually of short duration, that is, when the predominant airborne allergen is present. Typically, persons with SAC are symptom-free during the winter months in cooler climates because of the decreased airborne transmission of some allergens, such as pollen. Molds, house dust, and animal dander may also participate in the disease process. The severity of symptoms varies depending on the type of allergen, its concentration, and time of exposure.4 Dry eye facilitates allergen contact with the ocular surface since the capability of the tears to ‘wash away’ the allergen is usually compromised.13 The most significant symptom in SAC is itching. Patients usually complain of intense itching of the eyes, sometimes along with a burning sensation and tearing.14 Discharge is usually serous, clear and watery, but with a ropy characteristic.
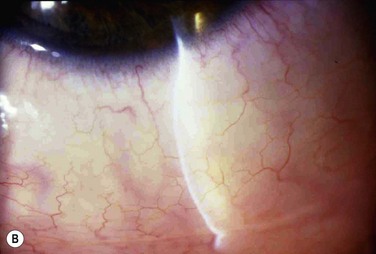
Signs in SAC include lid edema, conjunctival hyperemia and injection, and chemosis. Chemosis may be apparent in the bulbar and lower tarsal conjunctiva, giving to it a ‘milky’ or pale pink appearance. Some patients refer to a dramatic unilateral bulging of the conjunctiva, frequently described as the acute formation of a ‘bubble’ in the eye, mainly when patients rub their eyes. In reality, the conjunctiva balloons, due to intense and acute infiltration of cells and fluids, causing the chemosis (Fig. 13.1). The conjunctival chemosis can be very intense and may even cause unstable tear film and consequently corneal dellen (Fig. 13.2). These conditions tend to disappear with the resolution of the chemosis. Rarely, SAC and PAC affect the cornea, but the presence of punctate keratitis or dellen might lead to symptoms of pain, photophobia and blurred vision. SAC and PAC usually result in few to no sequelae.15
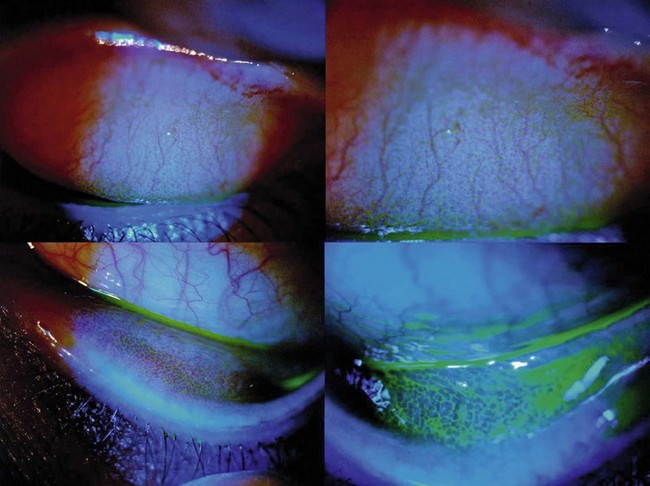
PAC is less common than SAC and, as patients are chronically exposed to allergen, symptoms and signs occur year-round. The most common triggers are mold spores, animal dander, and dust mites usually found in the household. Patients may also be sensitive to seasonal allergen with a superimposed offender to their symptoms. Symptoms and signs in PAC are similar to those in SAC but are usually milder and with longer duration. Because of the prolonged exposure, the conjunctiva may become boggy, chronically red, and irritated. Papillary hypertrophy along the tarsal conjunctival surface (Fig. 13.3) may occur with chronic exposure to allergens in PAC. The discharge is whitish but thick, and even stringy.4
Diagnosis of SAC and PAC
The diagnosis of SAC and PAC is generally based on clinical history and careful biomicroscopic examination.16 Important features of the history include a personal or family history of atopic disease, such as allergic rhinitis, bronchial asthma, and/or atopic dermatitis. As cited earlier, patients with PAC are more likely to also have perennial rhinitis.1
Perhaps the most important symptom is itching. Without itching, the diagnosis of allergic conjunctivitis is suspect. With the intense itching, the diagnosis of SAC and PAC is very likely, but one should also consider dry eye, toxic conjunctivitis, contact dermatitis, blepharitis, and other forms of allergic conjunctivitis in the differential diagnosis.17 In these other disorders, itching is usually mild and occasional. It is worthwhile to pinpoint the location of itching. For example, patients who complain of ocular itching may be describing symptoms related to the skin of their eyelids. Careful questioning can distinguish itching of the conjunctiva from itching of the eyelid skin. Moreover, patients with dry eye tend to have mild itching located in the nasal inner part of the bulbar conjunctiva, due to allergen accumulation in the area of tear drainage.13
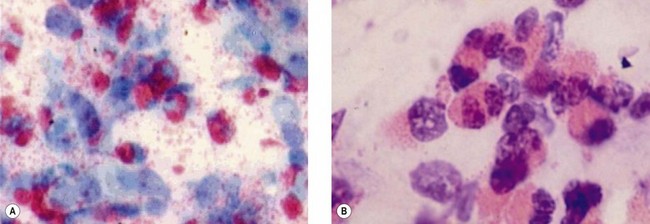
Superficial conjunctival scrapings may help to establish the diagnosis by revealing characteristic eosinophils (Fig. 13.4), which are not normally present on the conjunctiva. However, eosinophils are observed in the most severe cases, but are generally present in the deep layers of the substantia propria of the conjunctiva. For this reason, the absence of eosinophils on conjunctival scraping does not rule out the diagnosis of allergic conjunctivitis.18 Even the presence of one eosinophil or eosinophilic granules is consistent with a diagnosis of allergy. About 25% of patients with diagnosed SAC have eosinophils on cytological examination.8
The diagnosis can also be made by performing the conjunctival provocation tests, which consist of instilling offending pollen into the conjunctival sac, producing the typical symptoms of SAC. Conjunctival provocation tests are rarely necessary for the diagnosis of SAC and PAC, and it has rather proven to be a reliable method to evaluate ocular therapeutics.19,20 There is also a possible involvement of nasal allergy in some patients with allergic conjunctivitis, such as SAC and PAC, and therefore, there may be value to a nasal challenge with allergen combined with registration of the ocular features.1
The standard clinical test for the diagnosis of type I hypersensitivity reaction is the intradermal skin test. Cutaneous tests, such as the scratch or prick, and more rarely, the intracutaneous injections, may be utilized to determine the antigens causing the hypersensitivity. The prick test is the preferred method because it is more sensitive, less variable, and more comfortable to patients than the intracutaneous test.21
The radioallergosorbent test (RAST), a blood test, may also help to define the allergens. Elevated IgE levels in serum (RAST, ELISA) and in tear fluid are present in almost all patients with SAC and PAC.22
Treatment of SAC and PAC
Treatment of SAC and PAC includes reducing the amount of allergen exposure.17 One important goal of treatment is to prevent transformation of SAC to a chronic inflammatory process.
Because SAC usually involves allergens, such as tree, grass, and ragweed pollens, patients should avoid outside activities until late afternoon or after a heavy rain, when pollen levels are lower. SAC tends to be worse in warm, dry weather and to lessen with rain and cool temperatures. Patients should also keep windows in their home and car closed to lessen exposure to pollen. Hair and clothes should be washed after being outdoors. Patients should also be aware that pollen can also be transported indoors on people and pets. Wearing glasses or goggles can also serve as a barrier to allergens.17
As already mentioned, allergens in PAC are usually mold spores, animal dander, dust mites, and are predominantly found in the household. Therefore, carpets must be cleaned, changed or removed, as well as children’s stuffed animals, soft toys, and curtains. The mattress top and sides must also be cleaned and enclosed in plastic bags or other dust mite proof cover. Sheets, pillows and blankets should be washed in hot water (130°F or 54°C). Pillows and the base of the bed must be vacuumed regularly. Pets should be kept out of the bedroom, and the bathroom should be kept clean and dry to inhibit mold growth. While it is better to stop dust mites at the source, reducing the dust levels in the air could be an adequate strategy. Air purifiers that use HEPA filtration are more effective and safer. Most filters remove 50–70% of material. HEPA filters will remove up to 99% of the material; not just dust mite feces, but also all types of other allergens, such as animal dander, dust, pollen, cockroach feces, etc.23
Supportive treatment of both conditions includes cold compresses to decrease inflammation, avoidance of eye rubbing and the use of preservative-free artificial tears to wash or dilute allergens and inflammatory mediators away from the ocular surface. Artificial tear solutions should be kept in the refrigerator, since the use of cold drops produces vasoconstriction ameliorating symptoms and signs. There are several pharmacologic agents for the treatment of SAC and PAC, and their use will depend on the disease severity (Table 13.1).3
Table 13.1
Treatment options for SAC and PAC
| Agent | Mechanisms of Action | Drugs |
| Topical vasoconstrictor | Vasoconstriction reducing chemosis and edema | Naphazoline, oxymetazoline |
| Antihistamines | Histamine receptors blockage | Azelastine, emedastine, epinastine, levocabastine |
| Mast cell stabilizers | Decrease degranulation of conjunctival mast cells preventing release of histamine | Cromolyn sodium, lodoxamide |
| Dual acting agents | Histamine receptor antagonist and mast cell stabilizer | Alcaftadine, bepotastine, olopatadine, nedocromil, ketotifen |
| Non-steroidal anti-inflammatory drugs | Inhibition of prostaglandin and thromboxane production | Ketorolac tromethamine |
| Corticosteroids | Inhibition of phospholipase and arachidonic acid formation | Loteprednol, fluorometholone, prednisone acetate, dexamethasone |
| Immunomodulators | Inhibition of eosinophilic infiltration in conjunctiva (cyclosporine) or inhibition of T-cell action (tacrolimus) | Cyclosporine, tacrolimus |
Topical vasoconstrictors, alone or in combination with antihistamines, may provide short-term relief, mainly in SAC. The antihistamine is effective for the acute onset and reduces pruritus, while the decongestant reduces chemosis, eyelid edema, and redness via vasoconstriction. Examples of vasoconstrictors are naphazoline24 and oxymetazoline.25 However, vasoconstrictors may cause rebound conjunctival injection and inflammation, and they are ineffective in severe ocular allergy.
Antihistamine eye drops are prescribed for the relief of acute symptoms and signs of SAC and PAC by blocking the histamine receptors in the conjunctiva. These medications do not affect other proinflammatory mediators, such as prostaglandins and leukotrienes, which remain uninhibited. A number of topical antihistamines are available, including azelastine,26 emedastine,27 epinastine,28 and levocabastine.29 Systemic antihistamines may also relieve symptoms and signs of eye allergy. Second-generation H1 antihistamines, such as cetirizine and loratadine, are much more selective for peripheral H1 receptors, as opposed to the central nervous system H1 receptors, cholinergic receptors, and some H2 receptors that cause cardiac arrhythmia. This selectivity significantly reduces the occurrence of adverse drug reactions, such as drowsiness, dry eye30 and dry mouth.31
Topical mast cell stabilizers decrease the degranulation of conjunctival MCs, preventing the release of histamine and other chemotactic factors.32 However, the drug does not relieve existing symptoms and has no role in the treatment of the acute phase of SAC; mast cell stabilizers should be used on a prophylactic basis, mainly in cases of PAC. They need to be used long term (treatment effect usually requires continued use over 5 to 7 days) or in conjunction with other classes of medications, such as antihistaminics. Examples of MC stabilizers are cromolyn sodium33 and lodoxamide.34
Dual-acting agents exert multiple pharmacological effects, such as histamine receptor antagonist action, stabilization of MC degranulation and, subsequently, suppression of activation and infiltration of eosinophils. Examples are alcaftadine,31 bepotastine,35 olopatadine,36 nedocromil,37 and ketotifen.38
Nonsteroidal anti-inflammatory drugs (NSAIDs) act on the cyclooxygenase metabolic pathway and inhibit production of prostaglandins and thromboxanes. They have no role in blocking mediators formed by the lipoxygenase pathway, such as leukotrienes.39 Example of an NSAID that is approved for allergic indications is ketorolac tromethamine.40,41
Corticosteroid eye drops are very effective in treating SAC and PAC, but the numerous adverse effects, such as secondary infection, elevated intraocular pressure, and formation of cataract, make their use judicious and selective.42 Corticosteroids act at the first step of the arachidonic acid pathway by inhibiting phospholipase and arachidonic acid formation. Therefore, the anti-inflammatory and immunosuppressive effects of corticosteroids are broad and non-specific. Corticosteroids exist in various forms and concentrations. Steroids, such as loteprednol and fluorometholone, have less potency in the eye but fewer ocular adverse effects.43 In contrast, prednisolone acetate and dexamethasone are more potent but have a higher incidence of adverse effects. Topical steroids must be prescribed only for a short period of time and for severe cases that do not respond to other options of therapy. Pulse dosing of topical steroids may be employed, followed by maintenance with an MC stabilizer.23 There is some evidence supporting the ability of intranasal corticosteroids, used by patients with seasonal allergic rhinitis, to reduce allergic conjunctivitis symptoms.44 Fluticasone aqueous nasal spray has been effective in relieving nasal symptoms in adolescents and adults with seasonal allergic rhinitis.45 Patients using corticosteroids should be closely monitored.
Immunomodulatory agents, such as cyclosporine (0.05% to 2% drops)46 and tacrolimus (0.03% ointment)47 have demonstrated efficacy in the treatment of ocular allergy. Cyclosporine A is an immunosuppressant that acts by inhibiting eosinophilic infiltration by interfering with the type IV allergic reactions in the conjunctiva. Tacrolimus acts mainly by inhibiting the action of T cells. Both agents are associated with fewer side effects and are preferred over chronic use of corticosteroids in the treatment of allergic conjunctivitis. Immunomodulatory agents are reserved for more severe forms of allergic conjunctivitis, such as vernal and atopic keratoconjunctivitis and have limited indications in cases of SAC and PAC.
Allergen-specific immunotherapy is an effective treatment used to induce immunologic tolerance when the allergen is well known. The primary objectives of allergen-specific immunotherapy are to decrease the symptoms triggered by allergens and to prevent recurrence of the disease in the long term.3 It is indicated in patients who have evidence of specific IgE antibodies to clinically relevant allergens. Skin prick testing is the preferred method of testing for specific IgE antibodies and identification of allergen for the immunotherapy. Candidates for immunotherapy include those who: (1) have symptoms that are not well controlled by pharmacological therapy or avoidance measures, (2) require high doses of medication, multiple medications, or both to maintain control of their disease, (3) experience adverse effects of medications, or (4) wish to avoid the long-term use of pharmacological therapy.48
It is important to note that in the treatment of acute or chronic forms of allergic eye diseases, patient compliance may not be ideal, given the false impression of poor efficacy of treatment.49
References
1. Pelikan, Z. Seasonal and perennial allergic conjunctivitis: the possible role of nasal allergy. Clin Experiment Ophthalmol. 2009;37:448–457.
2. Bielory, L. Ocular allergy. Mt Sinai J Med. 2011;78:740–758.
3. Bilkhu, PS, Wolffsohn, JS, Naroo, SA. Non-pharmacological and pharmacological management of seasonal and perennial allergic conjunctivitis. Cont Lens Anterior Eye. 2012;35:9–16.
4. Friedlaender, MH. Ocular allergy. Curr Opin Allergy Clin Immunol. 2011;11:477–482.
5. Ziska, L, Knowlton, K, Rogers, C, et al. Recent warming by latitude associated with increased length of ragweed pollen season in central North America. Proc Natl Acad Sci USA. 2011;108:4248–4251.
6. Rosario, N, Bielory, L. Epidemiology of allergic conjunctivitis. Curr Opin Allergy Clin Immunol. 2011;11:471–476.
7. Offiah, I, Calder, VL. Immune mechanisms in allergic eye diseases: what is new? Curr Opin Allergy Clin Immunol. 2009;9:477–481.
8. Kari, O, Haahtela, T, Laine, P, et al. Cellular characteristics of non-allergic eosinophilic conjunctivitis. Acta Ophthalmol. 2010;88:245–250.
9. Katelaris, CH, Bielory, L. Evidence-based study design in ocular allergy trials. Curr Opin Allergy Clin Immunol. 2008;8:484–488.
10. Choi, SH, Bielory, L. Late-phase reaction in ocular allergy. Curr Opin Allergy Clin Immunol. 2008;8:438–444.
11. Leonardi, A, Fregona, IA, Plebani, M, et al. Th1- and Th2-type cytokines in chronic ocular allergy. Graefes Arch Clin Exp Ophthalmol. 2006;244:1240–1245.
12. Leonardi, A, Curnow, SJ, Zhan, H, et al. Multiple cytokines in human tear specimens in seasonal and chronic allergic eye disease and in conjunctival fibroblast cultures. Clin Exp Allergy. 2006;36:777–784.
13. Hom, MM, Nguyen, AL, Bielory, L. Allergic conjunctivitis and dry eye syndrome. Ann Allergy Asthma Immunol. 2012;108:163–166.
14. Kosina-Hagyo, K, Veres, A, Fodor, E, et al. Tear film function in patients with seasonal allergic conjunctivitis outside the pollen season. Int Arch Allergy Immunol. 2012;157:81–88.
15. Trocme, SD, Sra, KK. Spectrum of ocular allergy. Curr Opin Allergy Clin Immunol. 2002;2:423–427.
16. Mantelli, F, Lambiase, A, Bonini, S. A simple and rapid diagnostic algorithm for the detection of ocular allergic diseases. Curr Opin Allergy Clin Immunol. 2009;9:471–476.
17. Bielory, BP, O’Brien, TP, Bielory, L. Management of seasonal allergic conjunctivitis: guide to therapy. Acta Ophthalmol. 2012;90:399–407.
18. Wiszniewska, M, Pas-Wyroslak, A, Palczynski, C, et al. Eosinophilia in conjunctival tear fluid among patients with pollen allergy. Ann Allergy Asthma Immunol. 2011;107:281–282.
19. Nivenius, E, Van der Ploeg, I, Gafvelin, G, et al. Conjunctival provocation with airborne allergen in patients with atopic keratoconjunctivitis. Clin Exp Allergy. 2012;42:58–65.
20. Mourao, EM, Rosario, NA. Adverse reactions to the allergen conjunctival provocation test. Ann Allergy Asthma Immunol. 2011;107:373–374.
21. Radcliffe, MJ, Lewith, GT, Prescott, P, et al. Do skin prick and conjunctival provocation tests predict symptom severity in seasonal allergic rhinoconjunctivitis? Clin Exp Allergy. 2006;36:1488–1493.
22. Leonardi, A, Fregona, IA, Gismondi, M, et al. Correlation between conjunctival provocation test (CPT) and systemic allergometric tests in allergic conjunctivitis. Eye (Lond). 1990;4(Pt 5):760–764.
23. Bielory, L. Ocular allergy treatment. Immunol Allergy Clin North Am. 2008;28:189–224. [vii].
24. Dockhorn, RJ, Duckett, TG. Comparison of Naphcon-A and its components (naphazoline and pheniramine) in a provocative model of allergic conjunctivitis. Curr Eye Res. 1994;13:319–324.
25. Duzman, E, Warman, A, Warman, R. Efficacy and safety of topical oxymetazoline in treating allergic and environmental conjunctivitis. Ann Ophthalmol. 1986;18:28–31.
26. Canonica, GW, Ciprandi, G, Petzold, U, et al. Topical azelastine in perennial allergic conjunctivitis. Curr Med Res Opin. 2003;19:321–329.
27. Borazan, M, Karalezli, A, Akova, YA, et al. Efficacy of olopatadine HCI 0.1%, ketotifen fumarate 0.025%, epinastine HCI 0.05%, emedastine 0.05% and fluorometholone acetate 0.1% ophthalmic solutions for seasonal allergic conjunctivitis: a placebo-controlled environmental trial. Acta Ophthalmol. 2009;87:549–554.
28. Pradhan, S, Abhishek, K, Mah, F. Epinastine: topical ophthalmic second generation antihistamine without significant systemic side effects. Expert Opin Drug Metab Toxicol. 2009;5:1135–1140.
29. Takamura, E, Nomura, K, Fujishima, H, et al. Efficacy of levocabastine hydrochloride ophthalmic suspension in the conjunctival allergen challenge test in Japanese subjects with seasonal allergic conjunctivitis. Allergol Int. 2006;55:157–165.
30. Torkildsen, GL, Ousler, GW, 3rd., Gomes, P. Ocular comfort and drying effects of three topical antihistamine/mast cell stabilizers in adults with allergic conjunctivitis: a randomized, double-masked crossover study. Clin Ther. 2008;30:1264–1271.
31. Bohets, H, McGowan, C, Mannens, G, et al. Clinical pharmacology of alcaftadine, a novel antihistamine for the prevention of allergic conjunctivitis. J Ocul Pharmacol Ther. 2011;27:187–195.
32. Lambiase, A, Micera, A, Bonini, S. Multiple action agents and the eye: do they really stabilize mast cells? Curr Opin Allergy Clin Immunol. 2009;9:454–465.
33. James, IG, Campbell, LM, Harrison, JM, et al. Comparison of the efficacy and tolerability of topically administered azelastine, sodium cromoglycate and placebo in the treatment of seasonal allergic conjunctivitis and rhino-conjunctivitis. Curr Med Res Opin. 2003;19:313–320.
34. Das, D, Khan, M, Gul, A, et al. Safety and efficacy of lodoxamide in vernal keratoconjunctivitis. J Pak Med Assoc. 2011;61:239–241.
35. Williams, JI, Kennedy, KS, Gow, JA, et al. Bepotastine Besilate Ophthalmic Solutions Study Group. Prolonged effectiveness of bepotastine besilate ophthalmic solution for the treatment of ocular symptoms of allergic conjunctivitis. J Ocul Pharmacol Ther. 2011;27:385–393.
36. Shimura, M, Yasuda, K, Miyazawa, A, et al. Pre-seasonal treatment with topical olopatadine suppresses the clinical symptoms of seasonal allergic conjunctivitis. Am J Ophthalmol. 2011;151:697–702. [e2].
37. Alexander, M, Patel, P, Allegro, S, et al. Supplementation of fexofenadine therapy with nedocromil sodium 2% ophthalmic solution to treat ocular symptoms of seasonal allergic conjunctivitis. Clin Experiment Ophthalmol. 2003;31:206–212.
38. Torkildsen, GL, Abelson, MB, Gomes, PJ. Bioequivalence of two formulations of ketotifen fumarate ophthalmic solution: a single-center, randomized, double-masked conjunctival allergen challenge investigation in allergic conjunctivitis. Clin Ther. 2008;30:1272–1282.
39. Swamy, BN, Chilov, M, McClellan, K, et al. Topical non-steroidal anti-inflammatory drugs in allergic conjunctivitis: meta-analysis of randomized trial data. Ophthalmic Epidemiol. 2007;14:311–319.
40. Yaylali, V, Demirlenk, I, Tatlipinar, S, et al. Comparative study of 0.1% olopatadine hydrochloride and 0.5% ketorolac tromethamine in the treatment of seasonal allergic conjunctivitis. Acta Ophthalmol Scand. 2003;81:378–382.
41. Schechter, BA. Ketorolac tromethamine 0.4% as a treatment for allergic conjunctivitis. Expert Opin Drug Metab Toxicol. 2008;4:507–511.
42. Bielory, BP, Perez, VL, Bielory, L. Treatment of seasonal allergic conjunctivitis with ophthalmic corticosteroids: in search of the perfect ocular corticosteroids in the treatment of allergic conjunctivitis. Curr Opin Allergy Clin Immunol. 2010;10:469–477.
43. Ilyas, H, Slonim, CB, Braswell, GR, et al. Long-term safety of loteprednol etabonate 0.2% in the treatment of seasonal and perennial allergic conjunctivitis. Eye Contact Lens. 2004;30:10–13.
44. Bielory, L. Ocular symptom reduction in patients with seasonal allergic rhinitis treated with the intranasal corticosteroid mometasone furoate. Ann Allergy Asthma Immunol. 2008;100:272–279.
45. LaForce, CF, Dockhorn, RJ, Findlay, SR, et al. Fluticasone propionate: an effective alternative treatment for seasonal allergic rhinitis in adults and adolescents. J Fam Pract. 1994;38:145–152.
46. Utine, CA, Stern, M, Akpek, EK. Clinical review: topical ophthalmic use of cyclosporine A. Ocul Immunol Inflamm. 2010;18:352–361.
47. Garcia, DP, Alperte, JI, Cristóbal, JA, et al. Topical tacrolimus ointment for treatment of intractable atopic keratoconjunctivitis: a case report and review of the literature. Cornea. 2011;30:462–465.
48. Moote, W, Kim, H. Allergen-specific immunotherapy. Allergy Asthma Clin Immunol. 2011;7(Suppl. 1):S5.
49. Mishra, GP, Tamboli, V, Jwala, J, et al. Recent patents and emerging therapeutics in the treatment of allergic conjunctivitis. Recent Pat Inflamm Allergy Drug Discov. 2011;5:26–36.