Chapter 72 Seafood Toxidromes*
At least three-quarters of the world’s population lives within 10 miles (16 km) of the coast. One of many reasons why populations congregate near the sea is the abundance of food beneath the ocean’s surface. Seafood provides a significant percentage of protein in the diets of many cultures. Presently, 200 to 240 million tons of fish are harvested each year, with 50% of the total coming from coastal regions. Per capita fish consumption has increased in recent decades. Americans consume 7.3 kg (16.4 lb) of fish per person per year.185 The ocean is one of our last plentiful food resources. International trade has dramatically increased year-round availability of assorted seafoods, many of which come from distant geographic locations.441
Data on food-borne disease outbreaks in the United States demonstrate that by vehicle of transmission for foodborne-disease outbreaks, finfish and shellfish represent 5.0% and 2.0%, respectively.79 Some 90% of outbreaks of seafood-related illnesses and 75% of individual cases come from contaminated raw molluscan seafood (e.g., oysters, clams), histamine poisoning (scombroid), and ciguatoxin found in reef fish species.340 In general, marine toxins are heat stable and largely unaffected by cooking. Marine poisoning causes mostly gastrointestinal and neurologic symptoms. Many marine toxins target voltage-gated sodium channels in myelinated and unmyelinated nerves, resulting in a range of peripheral neurologic effects.219
Monitoring Phytotoxin-Producing Marine Algae and Seafood Poisonings
Despite the increasing risk of human intoxication from contaminated seafood, standards and methods of screening and law enforcement vary worldwide.487 According to the U.S. Department of Agriculture, imports account for more than 55% of total U.S. seafood consumption. The largest sources of seafood imported into the United States are Canada, Asia, and Latin America. The U.S. Food and Drug Administration (FDA) has been criticized for inadequate inspection of all food imports.340 In 1995, the FDA switched to a new program for seafood safety known as the Hazard Analysis and Critical Control Point (HACCP) system. This program became mandatory for the seafood industry on December 18, 1997.151 The HACCP focuses on the following: (1) identification of sources and points of contamination; (2) levels of the hazard(s) of concern, transmission rate, and transport of microorganisms; and (3) the possibility of exposure of the consumer to the contaminant. HACCP concentrates on preventing hazards rather than relying on spot checks and random sampling of products. The most effective control strategies can then be implemented. For shellfish- and virus-associated diseases, data suggest that harvesting from unapproved sources is associated with more than 30% of outbreaks.292 Among imports, the biggest risks relate to histamines and scombroid poisoning, mainly from tuna and mahi-mahi that is imported from Argentina, Taiwan, and Ecuador. For foods traveling great distances, refrigeration is the most critical aspect of controlling illness. Although there has been progress in improving standards for imported seafood in the United States, only 5% to 7% of the 8500 firms importing seafood in the United States during 2002-2003 were inspected by regulators.113
The United States is the second largest importer of shrimp worldwide. Shrimp aquaculture currently accounts for approximately 30% of the world’s supply. The FDA has amended the food additive regulations to provide for the safe use of ionizing radiation for control of foodborne pathogens in fresh or frozen molluscan shellfish.152
Molluscan poisoning is mainly a problem with domestic seafood. In 1991, California was the first state to require restaurants that serve or sell Gulf Coast oysters to warn prospective customers about possible deleterious effects from Vibrio contamination, particularly Vibrio vulnificus.378 Other states have since adopted these warning regulations. Additionally, fishermen are now required to refrigerate oysters within six hours after harvesting from the Gulf of Mexico. Regulations require oyster lot tagging, labeling, and record retention to facilitate trace-back investigations of outbreaks. The United States and Canada allow the sale of oysters if there are less than 10,000 colony-forming units per gram (CFU/g) of Vibrio parahaemolyticus. However, in outbreaks in the Pacific Northwest in 1997 and New York in 1998, oysters had less than 200 V. parahaemolyticus CFU/g of oyster meat, suggesting that human illness can occur at lower levels.77
Approximately one-third of U.S. shellfish beds carry bans or limitations on harvesting because of high levels of fecal coliform bacteria. The fecal indicator system for shellfish-harvesting waters has been effective in protecting consumers against general types of bacteria in fecal contamination. However, several pathogenic bacteria are not predicted by the system. The efficacy of methods for virus recovery may range from 2% to 47%.507 The most promising of the new detection methods are based on molecular techniques. Deoxyribonucleic acid (DNA) hybridization and the polymerase chain reaction (PCR) have the advantages of specificity for particular pathogens, sensitivity, and speed (most assays are completed within a few hours). PCR has been used in shellfish to detect Salmonella, Vibrio species, and viruses, including hepatitis A virus and norovirus. High-performance liquid chromatography (HPLC) has also been used to detect and quantify many shellfish toxins.* Phytotoxin-producing marine algae are responsible for the syndromes of paralytic, neurotoxic, and diarrhetic shellfish poisoning. Closure of fisheries (product harvest areas) depends on the density of algae. In some cases, the decision to close a fishery is based on the toxicity level in shellfish; in others, algae in the water and toxin in shellfish must both be found. In Florida, more than 5000 cells/L of Ptychodiscus brevis must be detected before fisheries are closed. The quarantine level of saxitoxin (a neurotoxin found in marine dinoflagellates) varies between countries and ranges from 40 to 80 mg of toxin per 100 g (3.5 ounces) of seafood, as determined through mouse bioassay.20 The higher number is used in the United States, as monitored by the Interstate Shellfish Sanitation Conference and the FDA.
The maximal acceptable concentration of diarrhetic shellfish toxin (okadaic acid) also varies between countries because of lack of precise analytic methods for quantification. Countries with established regulations apply 4 to 5 mouse units or 20- to 25-mg equivalents of okadaic acid as an acceptance limit. In the United Kingdom, the Ministry of Agriculture, Fisheries, and Food shellfish surveillance program tests harvested shellfish weekly from April to October and sporadically during the winter for the presence of toxins.410 The United States, Canada, and Portugal monitor for domoic acid (the cause of amnesic shellfish poisoning) and use 2 mg/100 g of seafood as the threshold. Ciguatoxins are monitored infrequently because of difficulties associated with the assay. In French Polynesia, ciguatoxin at 0.06 ng/g of seafood as determined by mosquito bioassay is considered toxic; in the United States (Florida, Hawaii), detection of the toxin at any level by immunoassay renders the fish unmarketable. Two primary features render toxin surveillance difficult: performance problems of the assays and impracticality of surveying every fish.
Sustainable and Safe Seafood Initiatives
Recently, there have been numerous initiatives by private, nonprofit, organizations to promote practices that will result in sustainable fisheries, restoration of marine ecosystems, and safer seafood arriving to markets. These initiatives include the industry-centric FishWise (http://www.fishwise.org), which encourages sustainable use of fisheries by educational and certification programs primarily directed toward producers/harvesters, distributors, and retailers in the industry. In addition, FishWise publishes a periodically updated list of fish containing a low level of mercury that is useful for both consumers and industry (Box 72-1). Other initiatives, such as those by Blue Ocean Institute (www.blueocean.org), include a more consumer-based focus with educational outreach that includes smartphone applications that provide instant, color-coded guides to sustainable seafood.
Ichthyosarcotoxism
Ichthyocrinotoxication
Ichthyocrinotoxic fish poisoning is induced by ingestion of glandular secretions not associated with a specific venom apparatus; this usually involves skin secretions, poisonous foams, or slimes. Examples of these toxic fish are certain filefish, puffer fish, porcupinefish, trunkfish, boxfish, cowfish, lampreys, moray eels, and toadfish (Box 72-2). Cyclostome poisoning results from ingestion of the slime and flesh of certain lampreys and hagfishes. Pahutoxin and homopahutoxin have been isolated from secretions of the Japanese boxfish Ostracion immaculatus.159
BOX 72-2 Representative Ichthyocrinotoxic Fish Hazardous to Humans
Ichthyotoxic skin secretions may cause a bitter taste.177 Ingestion of ichthyocrinotoxins causes gastrointestinal symptoms within a few hours of ingestion, characterized by nausea, vomiting, dysenteric diarrhea, tenesmus, abdominal pain, and weakness. Most victims recover within 24 hours; however, some individuals have symptoms for up to 3 days. Therapy is supportive and based on symptoms. Additionally, some slime, such as “grammistin” from the soapfish (Rypticus saponaceus of the family Grammistidae), can cause contact irritant dermatitis.204 This dermatitis is managed with cool compresses of aluminum sulfate and calcium acetate (Domeboro). All suspect fish should be washed carefully with water or brine solution and skinned before being eaten.
Ichthyohepatotoxication
Ichthyohepatotoxic fish carry the toxin predominantly in the liver. The remainder of the fish may be nontoxic. Fish that are always toxic fall into two basic groups: (1) Japanese perch–like fish (e.g., mackerel, seabass, porgy, sandfish) and (2) tropical sharks (e.g., requiem fish, sleeperfish, cowfish, great white shark, catfish, hammerhead, angelfish, Greenland fish, dogfish).361 In addition, some skates and rays, whose phylogeny is similar to that of sharks, harbor ichthyohepatotoxins.
Ingestion of the Japanese perch–like fish group causes onset of symptoms within the first hour, with maximal intensity over the ensuing 6 hours.436 Symptoms include nausea, vomiting, headache, flushing, rash, fever, and tachycardia. No fatalities have been reported.
Ingestion of tropical shark liver (and occasionally of the musculature), such as that of the Greenland shark (Somniosus microcephalus), results in “elasmobranch poisoning” (Box 72-3).25 Symptoms are noted within 30 minutes of ingestion and include nausea, vomiting, diarrhea, abdominal pain, malaise, diaphoresis, headache, stomatitis, esophagitis, muscle cramps, arthralgias, paresthesias, hiccups, trismus, hyporeflexia, ataxia, incontinence, blurred vision, blepharospasm, delirium, respiratory distress, coma, and death. Recovery varies from several days to weeks. If only the flesh is eaten, the symptoms are mild and gastroenteric, with spontaneous resolution.
BOX 72-3 Representative Poisonous Sharks (Elasmobranchs) Hazardous to Humans
In 1993, 200 people in Madagascar were poisoned after ingesting a single shark identified as Carcharhinus leucas. They all experienced symptoms, and 30% died. Two liposoluble toxins were isolated from the shark liver and named carchatoxin-A and carchatoxin-B.46 Trimethylamine oxide, found in shark liver and flesh, has also been implicated in shark poisoning.13 A similar syndrome has occurred in sled dogs that ingest large quantities of shark flesh.
Ichthyootoxication
Ichthyootoxic fish possess toxic gonads that may vary in toxicity with the reproductive cycle. The musculature is generally nontoxic. Examples are sturgeon, alligator gar, salmon, pike, minnow, carp, catfish, killifish, perch, and sculpin. Sea urchins may be toxic during the reproductive period.25 This toxicity is exemplified by Paracentrotus lividus (Europe), Tripneustes ventricosus (West Africa), and Diadema antillarum (West Indies). Heat does not inactivate the toxin.
Ichthyoallyeinotoxication
Ichthyoallyeinotoxic fish induce hallucinatory fish poisoning. These are predominantly reef fish of the tropical Pacific and Indian reefs; they carry these heat-stable toxins mainly in the head, brain, and spinal cord and in lesser amounts in the musculature. Typical species include surgeonfish, chub, mullet, unicornfish, goatfish, sergeant major, grouper, rabbitfish, rock cod, drumfish, rudderfish, and damselfish. Hallucinatory mullet poisoning has been described as a seasonal condition that occurs only during the summer months in restricted areas on the Hawaiian islands of Kauai and Molokai.206 Symptoms can develop within 5 to 90 minutes of ingestion and include dizziness, circumoral paresthesias, diaphoresis, weakness, incoordination, auditory and visual hallucinations, nightmares, depression, dyspnea, bronchospasm, brief paralysis, and pharyngitis.25 No fatalities have been reported. Various toxins, including indoles akin to lysergic acid diethylamide (LSD), have been implicated, the sources being in algae and plankton eaten by the fish.428 Heating the fish does not appear to lessen the severity of poisoning.
Specific Fish-Related Toxic Syndromes
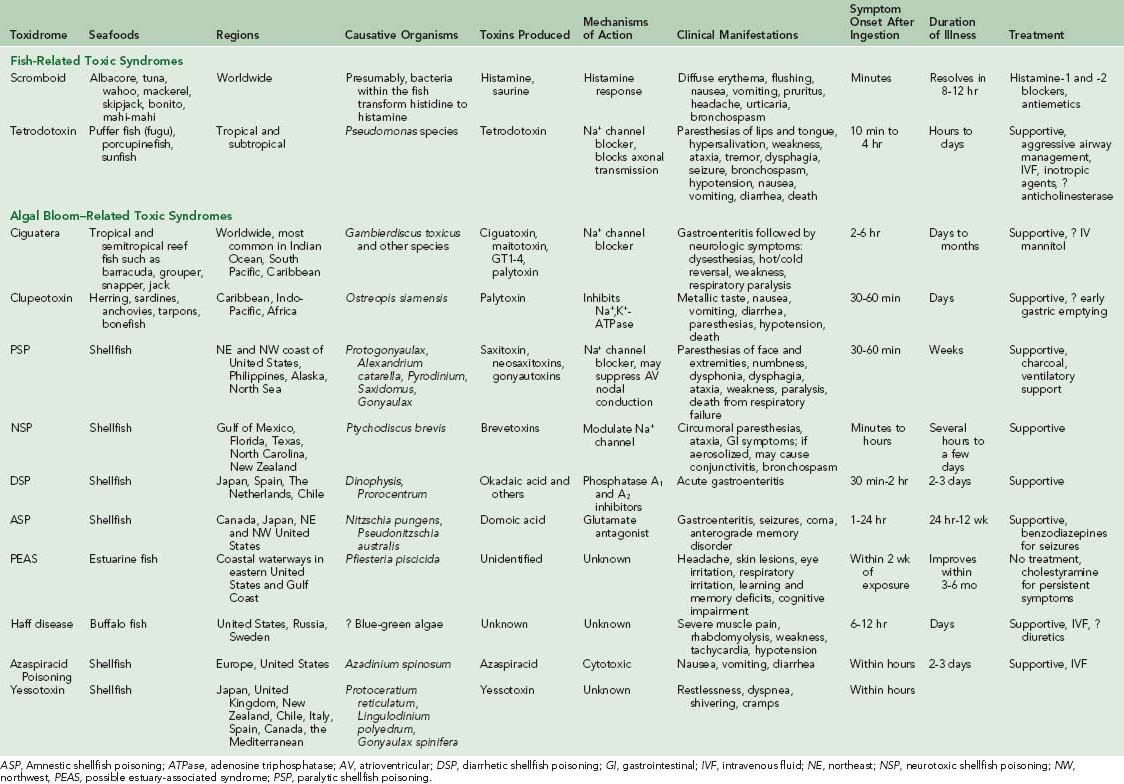
Three specific toxic syndromes related to fish consumption are scombroid, tetrodotoxin (puffer fish) poisoning (both described in Table 72-1), and grass carp gallbladder poisoning.
Scombroid
Scombroid, the most commonly reported seafood poisoning in the United States, occurs after eating fish with high levels of accumulated histamine or other biogenic amines. The first report of scombroid poisoning was published in 1830 and involved five sailors who consumed bonito fish, a member of the Scombridae family, hence the name of the syndrome.276 Other members of the family Scombridae include albacore, bluefin and yellowfin tuna, mackerel, saury, needlefish, wahoo, and skipjack. Non-Scombridae fish that produce scombroid include mahi-mahi (dolphin-fish), kahawai, sardine, black marlin, pilchard, anchovy, herring, amberjack (yellowtail or kahala), and the Australian ocean salmon Arripis truttaceus.313,417,433,462 Most of these fish species are rich in free histidine in their muscle tissues.216 Scombroid poisoning accounts for 3% of food-related outbreaks reported to the Centers for Disease Control and Prevention (CDC) in Atlanta.80 Underreporting is likely because of the short duration of illness and its resemblance to an allergic reaction. Because greater numbers of previously considered nonscombroid fish are now recognized as “scombrotoxic,” Prescott377 has suggested that the syndrome be more appropriately called pseudoallergic fish poisoning.
Pathophysiology
During conditions of inadequate preservation or refrigeration, the musculature of dark-fleshed or red-muscled fish undergoes bacterial decomposition.33,361 The normal surface bacteria Proteus morganii, Klebsiella pneumoniae, Aerobacter aerogenes, Escherichia coli, Alcaligenes metalcaligenes, and others have been implicated in the putrefactive process, which includes decarboxylation of the amino acid L-histidine to histamine and saurine (a phosphate salt of histamine).462 This most often occurs when fish is held at ambient or high temperatures for several hours.113 The term saurine originated because of the association of scombrotoxism with saury, a Japanese dried fish delicacy.214 Because of this process, “scombrotoxin” was initially thought to be histamine, which is commonly found in large amounts in the flesh of the fish usually implicated. Evidence initially suggesting that histamine may be the causative toxin of scombroid fish poisoning was presented in an investigation of a small outbreak.327 The urinary excretion of histamine and its metabolite, N-methylhistamine, was measured in three persons in this series who had scombrotoxism after ingestion of marlin. There was no increase in the principal metabolite of prostaglandin D2 (a mast cell secretory product considered to indicate release of histamine from mast cells), supporting the hypothesis that the excess histamine was from the fish rather than endogenously produced in the victims. Histamine levels greater than 20 to 50 mg/100 g are frequently noted in scombrotoxic fish, and it is not unusual to record levels in excess of 400 mg/100 g.417 However, it is possible that some other compound may be responsible for scombroid symptoms, because the syndrome cannot be reproduced solely by administration of equal or even massive doses of histamine by the oral route. Histamine is rapidly inactivated by enzymes in the gastrointestinal tract and on first pass through the liver, with very little reaching systemic circulation. Other compounds, such as cadaverine or putrescine, may be present in the decomposed fish flesh and may either facilitate the absorption or inhibit the gastrointestinal or hepatic degradation of histamine.396,462 Whatever the causative toxin, it is heat stable and not destroyed by cooking. Affected fish typically have a sharply metallic or peppery taste but may be normal in appearance and color. Not all persons who eat a scombrotoxin- or histamine-contaminated fish become ill, possibly because of uneven distribution of decay within the fish.
Clinical Presentation
The effects of scombroid fish poisoning occur within minutes after consumption of the fish. The symptoms are similar to an allergic reaction (which it is not) and typically include headache, diffuse erythema, sense of warmth without elevation in core temperature, nausea, vomiting, diarrhea, abdominal cramps, conjunctival injection, pruritus, dizziness, and burning sensation in the mouth and oropharynx.30,246,313 Flushing of the head, neck, and upper torso is characteristic. Severe effects, such as bronchospasm, generalized urticaria, hypotension, palpitations, and dysrhythmias, have been reported but are not frequent.174,214 In most healthy victims, the syndrome is self-limited, resolving within 6 to 12 hours. In rare cases, symptoms can persist beyond 24 hours.216 In patients with preexisting respiratory or cardiac disease, the effects of the poisoning can precipitate more severe illness.49,313 Scombroid reactions may be markedly more severe in patients taking isoniazid (INH) because of this compound’s blockade of gastrointestinal tract histaminase.485 Death has never been reported after scombroid poisoning. Assays of histamine and its metabolite in urine samples of scombroid-poisoned patients demonstrated elevated levels compared to controls, although histamine measurement is neither common clinical practice nor recommended. Histamine levels poorly correlate with clinical manifestations and do not affect management decisions.
Treatment
Gastric decontamination for scombroid poisoning is not indicated because symptoms occur rapidly and vomiting can be a primary effect of the toxin. Symptoms can be lessened or controlled with administration of histamine-1 (H1) receptor antagonists, such as diphenhydramine or hydroxyzine, administered initially in doses of 25 to 50 mg orally or intravenously. Histamine-2 (H2) receptor antagonists (e.g., cimetidine, famotidine) have also been shown to relieve most of the symptoms; perhaps a combination of H1 and H2 receptor antagonists would be most effective.44,188 Vomiting is usually controlled by an antihistamine, but occasionally requires addition of a specific antiemetic, such as ondansetron. The persistent headache of scombroid poisoning may respond to cimetidine or a similar drug if standard analgesics are not effective.18 Intravenous fluids and inhaled bronchodilators should be used as needed. Vasopressors are rarely necessary because hypotension is usually mild and responds to intravenous fluid administration. Corticosteroids are generally not indicated, because this illness is a toxic reaction and not immune mediated.
Prevention
The only effective method for prevention of scombroid fish poisoning is consistent temperature control at <−40° F (≤4.4° C) at all times between catching and consumption.113 It has been difficult to reduce the occurrence of scombroid poisoning in the United States; recreational catches likely plays a major role.216 No fish should be consumed if it has been handled improperly or has the smell of ammonia. Fresh fish generally has a sheen or oily rainbow appearance; “dull” packaged fish should be avoided. If an episode of scombroid poisoning is recognized, it is important to report it promptly to local public health authorities to prevent additional exposures, particularly if the food was served in a public eating establishment.215
Tetrodotoxin Poisoning
Tetrodotoxin (TTX) is a potent neurotoxin found in a variety of creatures and has been isolated from animals of four different phyla, including puffer fish, California newt, blue-ringed octopus, poison dart frogs, ivory shell, and trumpet shell. TTX is characteristic of the order Tetraodontiformes.449 The suborder Tetrodontoidei contains three families of fish (Tetraodontidae, Diodontidae, and Canthigasteridae), including puffer fish (toadfish, blowfish, globefish, swellfish, balloonfish, toado) and porcupinefish. Sunfish (Mola species) are members of the suborder Moloidei. Tetrodotoxin was named around 1911 after searching for the active ingredient in fugu ovaries.156 Isolation of the chemical was achieved in the 1950s. In the 1970s, the major toxin in certain poison dart frogs was identified as TTX. Crystalline TTX was isolated in 1978. The puffer fish is one of the better-recognized species that contains TTX. These fish can be found in both fresh and salt water and can inflate their bodies to a nearly spheric shape using air or seawater.193 Human TTX poisonings have also occurred after consumption of gastropod mollusks.523 Envenomation from the blue-ringed octopus is rare.150
Puffer fish poisoning has been recognized for millennia. Ancient Asian literature documents the dangers of eating puffer fish.193 There are references to puffer fish in hieroglyphics of the ancient Egyptian dynasty of 2700 BC. Scholars suggest this fish was known to be poisonous during Egyptian times. Mosaic sanitary laws against eating fish without fins and scales may have been derived to avoid fish containing TTX; the TTX-containing fish in the region inhabited by the Israelites were scaleless.193
Captain James Cook, the British explorer, recorded in 1774 his experience after eating a piece of liver from a puffer fish purchased from a native fisherman during his voyages in the Pacific Ocean.495 Before preparing the fish for eating, it was described and drawn. Cook tasted the liver and wrote of a vivid feeling of extraordinary weakness and numbness.193 There has been some contention that TTX (also known as puffer powder) was used as a component of Haitian voodoo potion in the zombie ritual.475 This has been challenged on grounds, among others, that under the usual conditions of extreme alkaline storage, any TTX in a “zombie potion” would be decomposed irreversibly into pharmacologically inactive products.243,526
In humans, the most common exposure to TTX is through the ingestion of fugu, a special preparation of puffer fish.73 Sporadic cases have been reported in the United States.84 In Japan, chefs must undergo a rigorous certification process before they are allowed to prepare fugu. Fillet of the puffer fish contains very minute concentrations of TTX. Fugu is served raw with paper-thin slices placed into an ornate configuration. The presence of small quantities of TTX gives the desired effect of slight oral tingling. Importation of fugu into the United States is illegal, but smuggling has resulted in cases of poisoning. At least 50 of the more than 100 species of these fish have been involved in poisonings of humans or may be intermittently toxic.395 Many nonfish species also contain TTX (Box 72-4).
BOX 72-4
Non-Tetraodontiformes Containing Tetrodotoxin
Many years ago, when TTX was thought to be found exclusively in pufferfish, it was controversial whether TTX was endogenous. It is now known that TTX is accumulated through the food chain, in a several-step process starting with marine bacteria as the primary source of TTX.342 TTX may be produced by Pseudomonas species that live on the skin of the puffer fish.533 This would explain the transmittal of toxicity between toxic and nontoxic fish through skin contact. Other investigators have found that Vibrio and other species isolated from the intestines of puffer fish produce TTX.502 The exact origin of TTX in the food chain, however, remains unknown. The distribution of TTX in pufferfish appears to be species-specific. In general, the liver and ovaries have the highest toxicity, followed by intestines and skin.342 Female fish are considered more toxic than are males because there are especially high concentrations of TTX in ovaries. Musculature is less toxic, but still may contain a significant amount of TTX. The toxin is heat stable and not inactivated by freezing. There occurs seasonal variation of TTX concentration, with peak levels during spawning season. TTX is likely accumulated as a biologic defense agent.342
Pathophysiology
Tetrodotoxin blocks the action potentials in nerves by binding to the pores of the voltage-gated, fast sodium channels in nerve cell membranes. TTX has a unique nonprotein structure and is widely used as a research tool to study sodium channels. Mouse bioassays demonstrate that the minimal lethal dose of TTX by intraperitoneal injection is 8 to 20 mg/kg.328 The interaction of TTX with the sodium channel is thought to be stoichiometric, with each TTX molecule interfering with one channel. TTX affects the spike-generating process of sodium channels, not the resting or steady-state voltage.242
TTX interferes with both central and peripheral neuromuscular transmission. Although it is not a depolarizing agent, in animals it causes depression of the medullary respiratory mechanism, intracardiac conduction, and myocardial and skeletal muscle contractility. At the microcellular level, the mechanism of action of TTX is linked to the axon rather than to the nerve endplate. TTX blocks axonal transmission by interfering with sodium conductance within the depolarized regions of the cell membrane, perhaps by acting at a metal cation binding site in the sodium channel, without affecting presynaptic release of acetylcholine or its effects on the neuromuscular junction.4,207 There is no apparent effect on potassium permeability.393 Saxitoxin, implicated in paralytic shellfish poisoning, has essentially the same action as does TTX on the nerve membrane, although it is believed to have a discrete receptor.246 The poison in freshwater puffers may be composed of TTX or saxitoxin, the predominant toxin depending on the species. The LD50 (dose at which 50% die) for mice is 10 mg/kg when TTX is administered by intraperitoneal, intravenous, or subcutaneous routes.473
Animal studies suggest that TTX has a peripheral effect that results in vasodilation independent of α- or β-adrenergic receptors.226,245,292 Further studies suggest a dose-dependent action. At low doses, systemic blood pressure is lowered, although perfusion pressure is initially maintained. Higher doses of TTX result in a profound fall in blood pressure.242 Experiments with animal models using TTX from blue-ringed octopi demonstrate similar profound hypotension. Agonists (norepinephrine or phenylephrine) have been the most effective agents in raising blood pressure in models of TTX poisoning.150
Clinical Presentation
Clinical manifestations typically develop within 30 minutes of ingestion but may be delayed by up to 4 hours. During a 2002 outbreak in Bangladesh of 37 people (from eight families) who were poisoned from inadequately prepared puffer fish, 31 of the victims developed symptoms within two hours and eight died.2 Death has been recorded within 17 minutes of exposure. The extent and type of symptoms vary according to the individual and amount of TTX ingested. Usually, paresthesias of the lips and tongue are followed by several signs as mild as diaphoresis, to life-threatening, such as hypotension, respiratory failure, and coma.84 Other commonly described symptoms include weakness, headache, body paresthesias, and gastrointestinal symptoms such as nausea, vomiting, and abdominal pain. Hypersalivation, ataxia, cyanosis, dysphagia, aphonia, dyspnea, blurred vision, bronchorrhea, and bronchospasm have also been described.2,84,93 Early miosis may progress to mydriasis with poor pupillary light reflex.473 A disseminated intravascular coagulation-like syndrome is heralded by petechial skin hemorrhages that can progress to bullous desquamation and diffuse stigmata of prolonged coagulation. Hypotension can be profound and may be refractory to treatment. Bradycardia and atrioventricular node conduction abnormalities may be present. Complete cardiovascular collapse with respiratory paralysis precedes death. Normal consciousness may be maintained until shortly before death.156,473 In some older reports, 60% of victims died, most within the first 6 hours. Survival past 24 hours is a good prognostic sign.
Treatment
Treatment of TTX is primarily supportive with aggressive airway management and assisted ventilation.429 Decontamination should be considered with 1 g/kg of activated charcoal given as soon as practical following presentation. Atropine may be used to treat bradycardia in conjunction with adequate oxygenation (SaO2 > 92%). Intravenous fluid resuscitation should be initiated for hypotension; however, use of vasopressors may be required to maintain perfusion. α-Agonists such as phenylephrine or norepinephrine are more likely to be effective. No antidote is currently available to treat TTX poisoning; however, studies are ongoing.
Cholinesterase inhibitors, such as edrophonium and neostigmine, have been used to treat victims of TTX poisoning with mixed results. Some case reports have suggested subjective improvement in neurologic symptoms after administration of cholinesterase inhibitors.90,473 A recent case series suggested that neostigmine may help overcome respiratory muscle paralysis, which is the predominant cause of death.90 Other case reports noted no improvement after infusion of these compounds.2,301,470 Antihistamines and steroids have also been utilized without clear benefit.301
Grass Carp Gallbladder Poisoning
Fish gallbladder has long been used as a folk remedy in China and southeast Asia. In a case series of 17 patients from Vietnam, the most common reason for ingestion was for symptoms of arthritis.522 The toxin is found in the bile of freshwater fish of the family Cyprinidae. Grass carp (Ctenopharyngodon idellus) accounts for 80% of freshwater gall bladder poisoning in China.267 Serious illness is attributed to the nephrotoxic and hepatotoxic properties of a toxin found in the bile.85 The toxic ingredient is 5-α-cyprinol sulfate, a 27-carbon salt, which is heat stable and not destroyed by ethanol.18,263 Most cases have occurred in Hong Kong, Taiwan, and South Korea. Two cases were reported in the United States in immigrants who ate raw gallbladders from carp caught in Maryland.70 One of the patients required hemodialysis for acute renal failure.
Several hours after ingestion, abdominal pain, nausea, vomiting, and watery diarrhea develop. This can be accompanied by marked elevations in concentrations of liver enzymes (aspartate and alanine aminotransferases).118 The hepatitis is usually self-limited, although fulminant liver failure has been reported in one patient. It was unknown if this patient had underlying liver disease prior to the intoxication.522 Nephrotoxicity occurs in moderate to severe poisonings and may be profound, leading to oliguric or nonoliguric renal failure within 48 to 72 hours after ingestion.398,522 Renal and liver biopsies demonstrate acute tubular necrosis and hepatocellular injury. With appropriate supportive care, including dialysis, patients typically recover. Acute renal failure accounts for more than 80% of deaths, although mortality rate has declined, likely due to advances in intensive care and renal salvage therapy.267
Poisonings Associated With Algal Blooms
Although there are thousands of species of microalgae that form the base of the food chain, fewer than 60 species are toxic or harmful. These toxic species may cause significant kills of fish and shellfish, mortality among seabirds and marine mammals, and human illnesses and death. Algal toxins have resulted in more than 500,000 incidents per year, with an overall mortality rate of 1.5% on a global basis.501 In the United States, harmful algal blooms now threaten virtually every coastal state, and the number of toxic species is increasing. Algae can reproduce rapidly, even to the point of discoloring the sea, producing “red tides.”441 Several distinct clinical syndromes exist: ciguatera fish poisoning, clupeotoxic fish poisoning, paralytic shellfish poisoning, neurotoxic shellfish poisoning, diarrhetic shellfish poisoning, amnestic shellfish poisoning, possible estuary-associated syndrome, and Haff disease (see Table 72-1). Beside these more well-known syndromes, several newer syndromes have been characterized recently, including azaspiracid toxins, yessotoxin and palytoxin.
Most dinoflagellate toxins are neurotoxins, causing toxicity via their interaction with voltage-sensitive ion channels or specific receptors associated with neurotransmitter release. Some block the channel pore physically and prevent ion conductance (hydrophilic low-molecular-mass toxins and large polypeptide toxins). Others alter voltage-dependent gating through binding to intramembranous receptor sites (alkaloid toxins and related lipid-soluble toxins) or intracellular sites (polypeptide toxins).501
Ciguatera
The name ciguatera is derived from the Spanish name cigua for the sea snail Turbo pica found in the Caribbean Spanish Antilles.26,466 This neurotoxic syndrome has been recognized throughout history, with one of the earliest cases having probably been reported in the 4th century when Alexander the Great refused to allow his soldiers to eat fish, and another during the Tang Dynasty in China.443 One of the earliest written records of suspected ciguatera poisoning is from the journal of Captain William Bligh, who described symptoms consistent with ciguatera in 1789 after eating mahimahi.443 In addition, it was also quite possibly ciguatera that was illustrated by Captain James Cook while sailing on the Resolution in the South Pacific in 1774.358
Ciguatera Fish Poisoning (CFP) is an important cause of foodborne disease and is endemic throughout subtropical and tropical regions of the Indo-Pacific and Caribbean. More than 400 species of fish have been implicated to cause CFP. In the United States, CFP is a prominent nonbacterial food poisoning associated with fish, second only to scombroid, with cases having been reported in many states.80,166,209,325,497 Outbreaks of ciguatera are greatest between the months of April and August. In endemic areas, the incidence is estimated to be between 500 and 600 cases per 10,000 people.269 Worldwide, ciguatera may affect more than 50,000 persons each year. Most cases in the United States occur in Hawaii and Florida, with the incidence in Florida estimated to be five cases per 10,000 people.138 The true incidence of CFP is difficult to ascertain because of underreporting. It is believed that only 2% to 10% of CFP cases are reported to health authorities.155 Outbreaks of ciguatera have been associated with ingestion of warm-water, reef-dwelling fish caught in the zone between the latitudes of approximately 30 and 35 degrees.29,194 In addition, the advent of flash-freezing and shipping of fish around the world has accounted for several cases of ciguatera in nonendemic areas.209
The most frequently implicated reef fishes are listed in Box 72-5. Of reported cases, 75% (except in Hawaii) involve the barracuda, snapper, jack, or grouper. Hawaiian carriers of the toxin include parrot-beaked bottom feeders and surgeonfishes, particularly those inhabiting waters with high dinoflagellate populations, such as those with disturbed coral reefs.225 Other fish that have been reported as ciguatoxic are listed in Box 72-6. Ciguatera has also been reported after ingestion of farm-raised salmon.126 There is one report of ciguatera from consumption of jellyfish.537
BOX 72-5
Frequently Implicated Reef Fish in Ciguatera Poisoning
From Gilbert DN, Moellering RC, Sande MA: The Sanford guide to antimicrobial therapy, ed 34, 2007, Sperryville, Va, Antimicrobial Therapy Inc., pp 98-99.
Pathophysiology
The blue-green and free algal dinoflagellate Gambierdiscus toxicus is thought to be responsible for producing ciguatoxins.443 G. toxicus adheres to dead coral surfaces and marine algae that are consumed by smaller herbivorous fish.176,269 Although G. toxicus is very likely responsible for the majority of ciguatoxins encountered in fish, the cyanobacterium Trichodesmium erythraeum can produce water- and lipid-soluble precursors to the toxins that may generate ciguatera syndrome.137 Other dinoflagellates, such as Prorocentrum concavum, Prorocentrum mexicanum, Prorocentrum rhathymum, Gymnodinium sanguineum, and Gonyaulax polyedra, may generate toxins that play a role in ciguatera syndrome.373,471
Larger reef fish eat the contaminated smaller fish, thereby becoming vectors as ciguatoxin is bioconcentrated up the food chain. As fish within the food chain become larger and older, the toxin is accumulated.102,204,214,361 Although the entire fish is toxic, the viscera (particularly the liver) and roe are considered to carry the highest concentrations of toxin.28 No plankton feeders have so far been reported to be ciguatoxic.
It has been suggested that proliferation of toxic algae may be triggered by contamination of water from a number of sources, including industrial wastes, golf course runoff, metallic compounds, ship wreckage, or other pollutants.194 In the Marshall Islands (Micronesia), consequent to nuclear testing, the incidence of toxin-producing plankton has tripled.382 Similar observations have been made with respect to various military activities (dumping and explosives) in the Line Islands and Gilbert Islands (Kiribati, Central Pacific), Hao Atoll (Tuamotu Archipelago, French Polynesia), Gambier Islands (French Polynesia), and others.392 Yet another cause of toxic dinoflagellate proliferation may be transfer and dumping of ballast water from large oceangoing vessels.
Ciguatera is associated with more than five toxins, including fat-soluble quaternary ammonium compounds (ciguatoxins), a water-soluble component (maitotoxin, from the Tahitian vernacular name maito for the striated surgeonfish Ctenochaetus striatus), a maitotoxin-associated hemolysin (lysophosphatidylcholine, or lysolecithin), and a ciguatoxin-associated adenine triphosphatase (ATPase) inhibitor.197,281,287,402 Scaritoxin (isolated from Scarus gibbus) is similar to the fat-soluble component and is specific to parrotfishes.86 Lipid-extracted toxins from G. toxicus have been designated GT-1, GT-2, and GT-3; a water-soluble toxin is designated GT-4.122,318 Chemical analysis of ciguatoxins demonstrates that they closely resemble brevetoxin C (from P. brevis) and okadaic acid, isolated from marine sponges and the dinoflagellate Prorocentrum lima.148,331 Identification of okadaic acid from the Caribbean dinoflagellate P. concavum lends support to the notion that this toxin may be more significant in ciguatera poisoning than previously thought. Another compound, named prorocentrolide, has also been found in reef-dwelling fish with okadaic acid and has been implicated in diarrhetic shellfish poisoning, another common fish-borne illness.148,213
Three major ciguatoxins (CTX-1, CTX-2, and CTX-3) are usually found in the flesh and viscera of ciguateric fishes. Each is found in variable concentrations, which may account for inconsistency of reported clinical signs and symptoms.287 CTX-2 is a diastereomer of CTX-3.286 Ciguatoxins may result from oxidation of gambiertoxins, possibly through the cytochrome system in the liver of fish.288 The lipid components have been characterized as crystalline, colorless, heat-stable compounds of approximate 1100 daltons molecular weight, with functional hydroxyl and quaternary nitrogen groups.
Ciguatoxins are potent Na+ channel toxins and exert their effects by activating voltage-sensitive Na+ channels. The Na channels open at resting membrane potentials, leading to spontaneous firing of neurons, giving rise to the neurologic signs and symptoms of ciguatera.219 One mechanism of their action may be that they falsely occupy calcium receptor sites that modulate sodium pore permeability in neural, muscle, and myocardial membranes.35 This effect could allow increased membrane permeability to sodium and cause sustained depolarization. Electrophysiologic studies of the sural and common peroneal nerves in humans with ciguatera, demonstrating reduced light touch, pain, and vibratory sensation in the extremities, showed prolongation of the absolute refractory, relative refractory, and supernormal periods. These findings indirectly suggest that CTX may abnormally prolong sodium channel opening in nerve membranes.63 This influx of sodium is antagonized by the presence of TTX.40
In vitro studies have also shown that scaritoxin causes release of norepinephrine and acetylcholine and increases sodium channel permeability.460 Maitotoxin as well may trigger release of norepinephrine and stimulate cellular uptake of calcium and has been hypothesized to stimulate cholinergic receptors by inhibiting acetylcholinesterase.40,428 However, evidence suggests that highly purified ciguatoxin preparations may not have anticholinesterase effects in vivo.280
Hypertension occurring with ciguatera can be suppressed in animal models with phentolamine (an α-antagonist), suggesting α-adrenergic receptor activity. Although purified ciguatoxin appears to have cardiac stimulatory effects (increasing heart rate and output), maitotoxin is a myocardial depressant in vitro, which may explain the variation in clinical presentation. Isolated human atrial trabeculae show concentration-dependent positive inotropy with CTX-1 that is not reversed with mannitol.285 Cardiac calcium conduction effects have been implicated in the activity of maitotoxin, because its action is inhibited in the presence of verapamil, magnesium ions, or low-calcium-concentration solutions. In mice, injection of maitotoxin can induce marked increase in total calcium content of the adrenal glands and rise in plasma cortisol concentration.464 When injected into mice, ciguatoxin targets the heart, adrenal glands, and autonomic nervous system.466 Ciguatoxin and CTX-4c (a derivative), administered in repeated doses, cause the mouse heart to suffer septal and ventricular interstitial fibrosis, accompanied by bilateral ventricular hypertrophy.468 Ciguatoxin is a potent substance, with an LD50 in mice of 0.45 mg/kg in purified form. Maitotoxin is even more potent, with an LD50 of 0.13 mg/kg in mice. It is interesting to note that ciguatoxins can become toxic to fish in higher concentrations, thus potentially limiting the levels of these compounds carried by a fish.284 However, the toxin or toxins may reside in the skeletal muscle or other tissues of the fish in association with proteins that may be protective of the carrier.190
All identified toxins associated with ciguatera are unaffected by freeze-drying, heat, cold, and gastric acid and do not affect the odor, color, or taste of the fish. There is some evidence that cooking methods can alter the relative concentrations of the various toxins. For example, boiling fish flesh will remove water-soluble toxins, but frying or grilling the flesh may increase toxicity of lipid-soluble toxins as a result of releasing lipid-soluble components from the cellular compounds to which they are normally bound.136
Clinical Presentation
CFP is associated with gastrointestinal, cardiovascular, neurologic, and neuropsychiatric symptoms and signs. The meal containing ciguatoxins is generally unremarkable in taste and smell. Symptoms may develop within minutes of ingestion, although they generally occur within 2 to 6 hours after the meal. Almost all victims develop symptoms by 24 hours.26,138 The severity of symptoms seems to follow a dose-dependent pattern, with victims who eat larger portions of ciguatoxic fish experiencing more severe symptoms (Box 72-7). Additionally, there are variable concentrations of ciguatoxin within a fish, depending on the fish size, age and part consumed, with higher concentrations in the viscera, especially the liver, spleen, gonads, and roe.257,273
The most common initial symptoms reported in cases of ciguatera include acute gastroenteritis, with abdominal cramps, nausea, vomiting, and diarrhea.26 These symptoms rarely persist for longer than 24 hours but may require fluid resuscitation.138 Myriad other symptoms reported in ciguatoxic patients are listed in Box 72-7. Headache is a common symptom, and victims often complain of experiencing a metallic taste. In a well-described clinical outbreak affecting a group of scuba divers who consumed coral trout (Cephalopholis miniatus), the most common symptoms were weakness, cold sensitivity, paresthesias, a taste sensation of carbonation, and myalgias.2 Two men suffering from ciguatera poisoning had painful ejaculation with urethritis, which in turn may have induced dyspareunia (pelvic and vaginal burning) in their female partners after intercourse.271 In a North Carolina outbreak in 2007, six of the seven sexually active patients reported onset of painful intercourse beginning in the first few days after the onset of illness. Although sexual transmission of ciguatoxin has been documented, painful intercourse as a consequence of ciguatera fish poisoning is not commonly described.273 Neurologic symptoms seem to develop after initial gastrointestinal symptoms. Paresthesias and myalgias are typically seen within the first 24 hours and usually resolve by 48 to 72 hours after ingestion of ciguatoxins, although there have been reports of neurologic symptoms persisting for weeks to months.27,277,362,273
Many case reports of ciguatera describe symptoms of a sensory perception of “hot and cold reversal,” and loose, painful teeth. Although presence of these symptoms is suggestive of ciguatera, their absence does not exclude possibility of the disease.27 There have also been reports of a paradoxical reversal of temperature perception, resulting in cold feeling hot, rather than hot feeling cold.27 However, other reports demonstrated that gross temperature discernment remains intact and the description of paradoxical heat perception may be misleading.62 These authors describe the symptoms as intense, painful tingling or “electric shock” rather than true reversal of hot and cold perception.62 This peculiar symptom may have a delay in onset of 2 to 5 days, may last for months after ingestion, and is otherwise seen only with neurotoxic shellfish poisoning (brevetoxins), caulerpicin (from the green alga Caulerpa) toxicity, or turban shell poisoning.128,525 These symptoms are commonly associated with a polyneuropathy, predominately affecting sensory small fibers.403 Pruritus is another vague but often described sensation in victims of ciguatera. Onset of pruritus may be delayed for more than 24 hours but is rarely, if ever, seen in the absence of other symptoms.148,277 Pruritus may persist for weeks and be exacerbated by any activity that increases skin temperature (blood flow), such as exercise or alcohol consumption.277 Ciguatera-associated pruritus may occasionally become severe and may improve after treatment with histamine receptor antagonists. Delayed symptoms also include hiccups.
Tachycardia and hypertension are often described in ciguatera poisoning, in some cases after transient bradycardia and hypotension, which can be severe.87 Hallucinations, flushing, flaccid paralysis, and fever occur but are uncommon. More severe reactions tend to occur in persons previously stricken with the disease. Severely affected persons may report intermittent symptoms for up to 6 months, with a gradual diminution in frequency and intensity. There may be some regional variability to the symptoms of presentation.27,324 Reappearance or worsening of symptoms after alcohol consumption has been described.273 Other foods and behaviors associated with symptom recurrence include nuts, caffeine, port wine, chicken, other fish, and physical activity/exertion.155 Persons who have ingested parrotfish (scaritoxin) have been reported to suffer from classic ciguatera poisoning, as well as a second phase of toxicity 5 to 10 days after the initial onset, consisting of ataxia, dysmetria, and a resting or kinetic tremor.94 Although both gastrointestinal and neurologic effects are the hallmarks of ciguatera intoxication, there are regionally dependent differences in clinical presentation. Neurologic effects predominate in the Indo-Pacific region, whereas gastrointestinal symptoms predominate in the Caribbean.219 Consumption of Indian Ocean fish has led to a further syndrome characterized by hallucinations, incoordination, loss of equilibrium, depression, and nightmares. Sensitization with repeated exposure has been described, leading to more rapid onset of effects.219
Whether ciguatoxin crosses the placenta is not known, but exposures during pregnancy have resulted in normal fetal outcomes.413 Transmission via breast milk has been reported.248 In small children, symptoms of ciguatera poisoning may be no more specific than irritability, sleep disturbance, nausea, and vomiting.508 Other reported symptoms include carpopedal spasm, ptosis, and inconsolability.
An overall death rate of 0.1% to 12% has been reported with ciguatera, but the lower percentage seems more likely with modern supportive care. Death is usually attributed to respiratory paralysis.237
Diagnosis
The diagnosis of ciguatera poisoning is based on clinical symptoms. Differential diagnosis includes paralytic shellfish poisoning, eosinophilic meningitis, type E botulism, organophosphate insecticide poisoning, TTX poisoning, and psychogenic hyperventilation.27,391 Temperature-related dysesthesia has also been reported in neurotoxic shellfish poisoning (NSP) from consumption of shellfish contaminated with brevetoxin. Therefore, NSP should be considered in the differential diagnosis. Unreliable folklore used in the past to aid in predicting ciguatoxic seafood includes the advice that a lone fish (separated from the school) should not be eaten. Other myths include ants and turtles refuse to eat ciguatoxic fish, that a thin slice of ciguatoxic fish does not show a rainbow effect when held up to the sun, and that a silver spoon tarnishes in a cooking pot with ciguatoxic fish.100 Ciguatoxin may be detected in the flesh of fish by two immunoassay techniques, a mouse bioassay where a sample of the fish is injected intraperitoneally into a mouse, and a rapid IgG assay.209 Rapid immunoassays have largely replaced using mice and other archaic tests (e.g., feeding fish to a mongoose or cat to observe for neurologic symptoms or death). HPLC is also available for ciguatoxins and okadaic acid. Unfortunately, tests for ciguatoxin are still of limited clinical benefit because most institutions do not have the equipment needed for their performance. Also, multiple individuals presenting with the same symptomatology that is consistent with CFP after consuming the same fish strongly supports the diagnosis.
Treatment
If possible, a piece of the implicated fish should be obtained in the event that analysis for ciguatoxins can be performed. Treatment of ciguatera poisoning is primarily supportive. Intravenous hydration with crystalloid and electrolyte replacement may be necessary for dehydration. Severe or refractory hypotension may require a vasopressor. Antiemetics such as ondansetron may be beneficial. Atropine has been shown to be effective in patients with symptomatic bradycardia or excess cholinergic stimulation.148 Gastric decontamination is rarely indicated, because presentation is usually delayed and gastroenteritis has already occurred. Activated charcoal may bind some of the toxin in the gastrointestinal tract, but this is not useful when presentation is more than 1 to 2 hours after exposure.
Many traditional remedies have been used for centuries to treat ciguatera. Edrophonium, neostigmine, corticosteroids, pralidoxime, ascorbic acid, pyridoxine (vitamin B6), salicylic acid, colchicine, and vitamin B complex have all been tried with variable success; however, there is no current clinical support for these modalities.324 Local anesthetics (e.g., lidocaine, tocainide) have also been administered for treatment of ciguatera.64,270 These agents are effective blockers of sodium influx and may antagonize the sodium channel effects of ciguatoxin. In addition, amitriptyline has been used for its sodium channel blocking effects, as well as its potent antimuscarinic effects.54,59,114 Nifedipine has been used to counteract the cellular uptake of calcium caused by maitotoxin, and to relieve headache.59 Although there is limited experience with most of these therapies, they may be beneficial in cases refractory to supportive care alone.
Mannitol has become the most widely applied therapy in severe cases of ciguatera poisoning.52,444 Most reports of its success are based on limited data with small numbers of patients.131,354,359,509 One series described successful treatment with mannitol in 24 victims of ciguatera poisoning. Each was infused with up to 1g/kg of a 20% mannitol solution intravenously over 30 minutes. None of the victims received more than 250 mL.354 The mechanism by which mannitol might be effective in abating the neurologic symptoms from ciguatera poisoning is unknown, but suggested theories have included acting as a free radical scavenger, competitive inhibitor of ciguatoxin at the cell membrane, and promoting a decrease in Schwann cell edema.359,509 It is also possible that the osmotic action of mannitol may render ciguatoxin inert.354,359 Curiously, mannitol therapy seems to have no beneficial effect on mice administered a sublethal intraperitoneal dose of ciguatoxin (CTX-1).289 A more recent double-blinded, randomized study on mannitol therapy found no difference in resolution of symptoms when compared with saline.403 Of note, therapy was not initiated until an average of 19 hours after exposure in the mannitol group and 40 hours after exposure in the saline group. In humans, the empiric observation is that mannitol has greater benefit if administered early in the course of illness, so the delay may have diminished the effect in this study. One concern with administration of mannitol in the setting of ciguatera is that patients may present dehydrated. In these cases, patients should be adequately rehydrated before administration of mannitol. During recovery from ciguatera, it is recommended that victims exclude fish, shellfish, alcoholic beverages, and nuts and nut oils from their diet, as these could result in an exacerbation of the syndrome.427 Gabapentin has been used successfully in the treatment of chronic symptoms after ciguatera poisoning, but symptoms seem to recur after cession of therapy in some patients.362
Prevention
For travelers, common sense dictates avoiding any fish that local fishermen and residents do not eat, or fish caught in areas known to be endemic for ciguatera. Any level of Caribbean ciguatoxin ≥0.1 ppb of fish tissue is thought to be a health risk.273 Because of the accumulation of toxin, all oversized fish of any predacious reef species (such as jack, snapper, barracuda, grouper, or parrot-beaked bottom feeder) should be suspected to be toxic. Moray eels should never be consumed. Internal organs of implicated fish seem to concentrate the toxin and should therefore be avoided. Natural events, such as hurricanes and earthquakes, have been associated with increased incidence of ciguatera, presumably because of reef disturbance. El Niño storms may also affect the incidence of ciguatera in the Pacific.29
Clupeotoxic Fish Poisoning
Clupeotoxic fish poisoning involves plankton-feeding fish that ingest blue-green algae and dinoflagellates. This poisoning is distinguished from ciguatera on the basis of the severity and high fatality rate of clupeotoxic fish poisoning and identification of the implicated clupeoid fish. These fish of the order Clupeiformes are found in tropical Caribbean, Indo-Pacific, and African coastal waters. Toxicity is reported to increase during warm summer months. Viscera are considered to be highly toxic. Previously, the toxin was poorly characterized as a result of the infrequency of the syndrome and rare access to toxic animals. The first case to shed light on clupeotoxism was reported in a Madagascar woman who died after eating a sardine, Herklotsichthys quadrimaculatus.352 This same sardine has been implicated in clupeotoxism in Fiji and the Philippines.527,529 The causative toxin was identified as palytoxin (PTX) or its analog, which distinctly differed from ciguatoxin. Palytoxin is an extremely poisonous nonprotein agent of low molecular weight that has been isolated from various zoanthid soft corals of the genus Palythoa, and subsequently from many other organisms such as seaweed and shellfish.189,501 Palytoxin was found in the dinoflagellate Ostreopsis siamensis, which caused blooms along the coast of Europe, resulting in extensive death of edible mollusks and echinoderms, and human illness.501 Since the structure of PTX was reported in 1981, numerous PTX-like substances have been described from various marine organisms.115 Palytoxin has been found in mackerel (Decapterus macrosoma), filefish (Altera scripta), freshwater pufferfish (Tetraodon sp.), triggerfish (Melichtys vidua), and several species of crab (Demania reynaudii, Demania alcalai, Lophozozymus pictor).6,115,157,258 PTX poisoning was recently suspected after cowfish (Lactoria diaphana) ingestion.421 Other examples include the families Clupeidae (herrings and sardines), Engraulidae (anchovies), Elopidae (tarpons), Albulidae (bonefishes), and Pterothrissidae (deep-sea slickheads).25,316
Pathophysiology
The benthic dinoflagellate O. siamensis was presumed to be the probable toxin source.352,524 As with ciguatoxin, the poison typically does not impart any unusual appearance, odor, or flavor to the fish. The exact mechanism of PTX toxic effects remains to be elucidated. However, in vitro studies have demonstrated multiple effects. PTX appears to increase cell permeability to sodium in neuronal cells by converting the sodium-potassium ATPase pump to a permeable channel to monovalent cations, allowing potassium efflux and sodium influx. The subsequent membrane depolarization may open voltage-dependent calcium channels in synaptic nerve terminals, cardiac cells, and smooth muscle cells. Additionally, there is increased intracellular calcium concentration through the sodium–calcium exchanger. Ultimately, the increase in intracellular calcium stimulates release of neurotransmitters from nerve terminals, histamine from mast cells, and vasoactive agents from the vascular endothelium.343,501 PTX may also increase cytosolic hydrogen concentration.501
Clinical Presentation
Symptoms of palytoxin exposure vary greatly, depending on the route of exposure. This was originally described using several animal species and various routes of exposure.506 Deaths have occurred due to PTX injection in animals and ingestion in humans. However, a variety of additional symptoms have been observed to be caused by dermal, ocular, and inhalational exposure in humans. Ingestion in humans reportedly causes abdominal cramps, nausea, diarrhea, limb paresthesias, muscle spasm, and respiratory distress. Of this cluster of symptoms, the predominant physical findings appear to be respiratory distress and extreme tonic muscle contractions. Severe debility leading to death may occur within 15 minutes of the onset of symptoms.194 Mortality has been reported to be as high as 45%. One of the most commonly reported complications appears to be rhabdomyolysis, with peak creatine kinase levels typically occurring 24 to 36 hours after symptom onset.115,349 A postmortem examination in one case after ingestion of Sardinella marquesensis (Marquesan sardine) flesh and viscera demonstrated enterocolitis and the sequelae of hypotension and acute heart failure.316
Inhalational exposure has also been described. In the summer of 2005, a massive proliferation of the tropical microalga Ostreopsis spp. broke out along the Mediterranean coastline of Liguria, near Genoa, Italy. Approximately 200 people experienced fever, conjunctivitis, and respiratory distress after exposure to this marine aerosol. Palytoxin and a new analog, ovatoxin-A, were later identified.95 Dermal exposures have also been described, specifically with handling of PTX-containing marine zoanthids sold in the home aquarium trade.210,343 There is a great deal of conflicting information regarding the risks of PTX exposure from store-bought aquarium zoanthids. Numerous unconfirmed anecdotal stories can be found by affected individuals online at coral reef hobbyist forums. PTXs are not found in all commercially available zoanthid species, but clearly occur in potentially dangerous concentrations in a select few.115
Prevention
Clupeotoxic fish should be avoided, especially during summer months. These fish are indigenous to the Caribbean, African coastal, and Indo-Pacific waters. The viscera of suspicious fish can be fed to experimental animals to see if an illness is generated. Because a rapid and sensitive hemolysis neutralization assay for palytoxin is available, its presence in toxic seafood should become easier to determine.41 Persons handling zoanthid coral should wear protective gloves to decrease the risk of local and systemic toxicity.
Paralytic Shellfish Poisoning
Shellfish have been implicated in poisonings for centuries, if not millennia. Epidemics of shellfish toxicity have been linked to the proliferation of dinoflagellates and other small marine organisms that are responsible for red tides or blooms in oceans around the world. The Bible refers to red tides in Exodus 7:20–21, where “the waters that were in the rivers were turned into blood, and the fish that was in the rivers died; and the river stank.” The Red Sea was so named by ancient Greeks for its red appearance in certain seasons when red tides occurred. Red tides are described in the Iliad and were first recognized by North American Indians as luminescence or “flickering” of ocean waves.68
Perhaps the first published description in the Western world of a patient with clinical findings suggestive of paralytic shellfish toxicity dates back to 1689. An article from a French journal named Ephemeredes des Curieux de la Nature described a young woman who had ingested mussels.89,192 The description notes that her symptoms included fever, chest pain, respiratory insufficiency, nausea, seizures, and tachycardia. She had emesis induced, bringing up the mussels, and eventually recovered. For years after this report, the incidence and cause of paralytic shellfish toxicity were undocumented throughout the world, but epidemics were known to occur in certain seasons and under certain conditions. Improvements in monitoring and public health reporting have demonstrated patterns of occurrence. Gessner and Middaugh168 described 54 outbreaks of paralytic shellfish poisoning (PSP) in Alaska occurring in 117 individuals between 1973 and 1992. The California Paralytic Shellfish Poisoning Prevention Program has been so successful that it has been a model of surveillance for many other countries.369 PSP has been a reportable condition in California since 1927, with more than 500 cases and 30 deaths reported since that time. In California, there is an annual 6-month quarantine (May through October) on locally harvested mussels, clams, and oysters.
Of the several types of neurologic diseases occurring after ingestion of shellfish, PSP is one of the most common. This syndrome is most frequently reported during the summer months when water temperature is highest, but it also has been recorded from May to November.178,192 Some authors suggest that the toxin responsible for PSP may be present in significant concentration in some shellfish, such as the Alaskan butter clam, in some areas year round, and that shellfish harvested from untested waters of these regions never be consumed.167 The most commonly implicated varieties of shellfish include mussels, clams, oysters, and scallops.168,192,244 Lobster hepatopancreas toxicity has also been noted.140 Although almost all outbreaks have been described from shellfish consumption, 13 cases of PSP were diagnosed in Florida in 2002 after ingestion of puffer fish containing saxitoxin, rather than TTX, were caught in the waters off Titusville.78 To distinguish these puffer fish poisonings from those caused by TTX, this food poisoning syndrome is becoming known in the literature as saxitoxin puffer fish poisoning (SPFP).140
Pathophysiology
The major toxin sources of PSP include marine dinoflagellates of the genera Alexandrium (formerly Gonyaulax), Gymnodinium, and Pyrodinium. Bacterial origins of the toxin have also been proposed.140
Dinoflagellates produce a number of toxins, the most commonly identified of which is saxitoxin. If a single organism predominates, it can discolor the water, creating a black, blue, pink, red, yellow, brown, or luminescent “tide.”96 Organisms can multiply rapidly from a concentration of 20,000/L to more than 20 million/L. These plankton can release massive amounts of toxic metabolites into the water, at times leading rapidly to enormous mortality in various bird and marine populations, including large mammals such as dolphins and even whales. Large numbers of dead animals on the beach suggest a colored tide. The trend to increased numbers and magnitude of blooms is empirically attributable to many factors, including coastal development, dumping of sewage, fertilizer runoff, and ocean warming. Kills by the dinoflagellate Ptychodiscus (formerly Gymnodinium) brevis are estimated at 100 tons of fish per day. The problem is markedly increasing in Europe.488
A limited number out of the approximately 1200 species of dinoflagellates has been implicated in human toxic syndromes.401 PSP has been linked to the dinoflagellate Protogonyaulax, species catanella (U.S. Pacific coast) species tamarensis var. excavata (U.S. Atlantic coast and Europe), and Gymnodinium catenatum (northwestern Spain).312,461 These creatures are relatively fastidious and prefer to bloom in warm, sunlit water of low salinity. Some algal organisms may release their toxin in the form of microscopic cysts, which can overwinter at the sediment–water interface. In mollusks, the greatest concentration of toxin is found in the digestive organs (e.g., the dark hepatopancreas), gills, and siphon.415 Toxic benthic dinoflagellate cysts may be transported by dredging operations, potentially introducing a dinoflagellate population into a new region.530
Although the origin of PSP toxins is assumed to be dinoflagellates, the toxins have been isolated in both marine and freshwater bivalves that are not associated with dinoflagellates. It has not been determined how this has occurred.346 The bacterium Moraxella isolated from Protogonyaulax tamarensis has been shown to produce PSP toxins in culture. Toxin production can increase in nutritionally deficient environments.259
The paralytic shellfish toxins identified to date are 18 related tetrahydropurine compounds produced mainly by dinoflagellates of the genus Alexandrium. These include saxitoxin, neosaxitoxin, and the gonyautoxins (GTX1, GTX2, GTX3, GTX4, GTX5), with the best characterized being saxitoxin.161 Saxitoxin (C10H17N7O4) takes its name from Saxidomus giganteus, the Alaskan butter clam. P. brevis is a toxic dinoflagellate that produces a milder toxin. Other dinoflagellates considered poisonous to animals or humans include Gonyaulax acatenella, Pyrodinium phoneus, Pyrodinium bahamense var. compressa, Gonyaulax monilata, Gonyaulax polyhedra, Gymnodinium veneficum, and Exuviaella ariae-lebouriae.353 S. giganteus and the Washington clam (Saxidomus nuttalli) may carry the toxin in their neck parts for up to 2 years; however, no physical characteristic distinguishes a carrier animal.
Unfortunately, a direct human serum assay to identify the toxin responsible for PSP is not readily available to clinicians. PSP is assessed in foodstuff using a mouse bioassay, in which a 20-g mouse is injected with 1 mL of an acid extract of the shellfish, and the time taken for the animal to die is recorded. One mouse unit (mu), or 0.18 mg, is the amount of injected saxitoxin that kills a test mouse in 15 minutes.488 In most countries, the action level for closure of a fishery is 400 mu/100 g shellfish. Polyclonal enzyme-linked immunosorbent assays (ELISAs) that measure saxitoxin, neosaxitoxin, and gonyautoxins 1 and 3 may be refined soon as reasonable screening techniques. Other testing methods under investigation include a sodium channel–blocking assay, spectrometry, thin-layer chromatography, and fluorometric HPLC.161,300 An automated tissue culture (neuroblastoma cell) bioassay may become a valid alternative to live animal testing.233
Saxitoxin (STX) and related compounds are water-soluble and heat and acid stable. At least 24 saxitoxin-like congeners have been identified with an array of hydroxyl, carbamyl, and sulfate substitutions on the backbone structure, also with large variation in potency.191,140 Like TTX, they can be destroyed to a certain extent in an alkaline medium but not by ordinary cooking. Saxitoxins are chemically distinct from TTX, but both act on site 1 of the voltage-dependent sodium channel, blocking influx of sodium into excitable cells and restricting signal transmission along nerve and muscle membranes.268 Although the threshold levels for causing illness in humans are not definitively known, it has been suggested that ingestion of 200 to 500 mg would cause at least mild symptoms; 500 to 2000 mg, moderate illness; and more than 2000 mg, serious or fatal illness. However, serious symptoms have been reported after ingestion of less than 100 mg of saxitoxin in adults. During peak red tide seasons, each mussel may accumulate up to 50,000 mu of saxitoxin. Mussel concentrations of saxitoxin have been determined to be too high for consumption when seawater dinoflagellate counts are as few as 200/mL.415 A saxitoxin concentration of greater than 75 to 80 mcg/100 g foodstuff is considered hazardous to humans. In the 1972 New England red tide, the concentration of saxitoxin in blue mussels exceeded 9000 mg/100 g foodstuff. After cases of PSP in Massachusetts, saxitoxin concentrations of 24,400 mg/100 g were recorded in raw mussels. With oral ingestion of saxitoxin, the LD50 for mice is 263 mg/kg. It has been estimated that as little as 0.5 to 1 mg of saxitoxin can be fatal in humans.415
Clinical Presentation
The onset of symptoms of paralytic shellfish poisoning is rapid. Within 30 to 60 minutes of ingesting toxic shellfish, victims complain of paresthesias, numbness, vertigo, and tingling of the face, tongue, and lips. Cranial nerve dysfunction, including dysarthria, dysphonia, dysphagia, and even blindness, can occur.168,192,214,312 Other early symptoms include lightheadedness, floating sensation, ataxia, weakness, hyperreflexia, incoherence, sialorrhea, thirst, abdominal pain, nystagmus, dysmetria, headache, diaphoresis, sensation of loose teeth, chest pain, and tachycardia. Neurologic symptoms progress to involve the extremities and trunk over the first 1 to 2 hours. Weakness of the limbs may begin anytime after the sensory changes, and gradually progresses to ataxia, inability to use the extremities, and finally paralysis. Reflexes are frequently normal throughout progression of the disease, and patients remain awake and alert. Death results from respiratory failure with diaphragmatic and chest wall muscle paralysis.
Although some victims have nausea, vomiting, or diarrhea, lack of gastroenteritis and thus early self-decontamination may in part explain why mortality from PSP approaches 25% in some older series.26,505 More recent reports cite a lower incidence of fatalities, probably because of improvements in supportive care. Hypotension can result from direct action of the toxin on vascular smooth muscle, although both diastolic and systolic hypertension have been reported.242,167 Toxicity is generally not delayed more than 10 to 12 hours, with a median onset of 3 hours. Prognosis is good for individuals surviving past 12 hours, but weakness can persist for weeks after recovery. Children seem to be more sensitive to saxitoxin than are adults. In milder cases, alcohol ingestion appears to increase toxicity. Saxitoxin is very similar structurally to TTX and shares a common mechanism of action. Intoxication causes superimposable symptoms, and these two syndromes can be differentiated only by their area of distribution or by isolation and identification of the specific toxin.145
Treatment
No antidotes are currently available for saxitoxin or paralytic shellfish poisoning. The victim should be closely observed in the hospital for at least 24 hours for respiratory insufficiency. Airway patency and respiratory support are of utmost importance, and even patients with severe symptoms of PSP often do well if expeditiously supported with mechanical ventilation. Although gastric emptying has been advocated by some authors when shellfish suspected of containing saxitoxin are ingested, airway collapse can be rapid and induction of emesis should not be attempted.214 These toxins bind well to charcoal, and an oral dose of charcoal should be administered if this can be done safely.85 Some clinicians suggest that atropine administration may worsen symptoms of PSP and should be avoided, because saxitoxin and its derivatives may have antimuscarinic effects.414 Several studies have suggested that acidity may enhance the potency of saxitoxin, leading some authors to speculate that serum alkalinization might be of benefit to victims, although the efficacy of this practice has yet to be established.9,203,307,356
At least one human case report and some animal data have implied that dialysis or hemoperfusion may benefit some victims of severe PSP.26,377 Other reports are less optimistic, as in vitro trials have demonstrated that dialysis is not effective in removing saxitoxin.132,203 Some clinicians have suggested enhancing renal clearance with diuresis, but no study supports this practice. Maintaining normal urine output should suffice in most cases.
Prevention
The most important aspect of managing PSP is prevention. Although leeching of shellfish in freshwater for several weeks followed by vigorous cooking may remove up to 70% of the toxin, such procedures are recommended only for persons stranded on desert islands. It has been said that one should not eat shellfish in the northern hemisphere in months that contain the letter r. It has become more apparent with changing ocean conditions that shellfish in many parts of the world may be contaminated throughout the year because of high water concentrations of Gonyaulax. Most coastal agencies monitor dinoflagellate concentrations off the shores of developed countries and restrict shellfish harvesting during high-risk periods. In addition, harvesting management strategies, such as harvesting parts of the organisms known to be safe and discarding the parts of the organism that may pose a threat, are in place.140 Many outbreaks of this illness have occurred on isolated islands where public health monitoring is infrequent and intensive care medicine resources scarce. Saxitoxin found in southern puffer fish off the coast of Florida is much more concentrated within the muscle than in the liver; therefore, even careful preparation of these puffer fish fillets would not prevent intoxication to consumers.268
Neurotoxic Shellfish Poisoning
P. brevis is a toxic dinoflagellate that creates a colorful tide when it blooms. Ingestion of shellfish contaminated with P. brevis can induce a milder version of PSP known as neurotoxic shellfish poisoning (NSP). The condition resembles ciguatera toxin poisoning in symptoms and does not have a major paralytic component. Death has not been reported in humans. Symptoms include circumoral paresthesias and paresthesias of the extremities, dizziness and ataxia, muscle aches, and gastrointestinal symptoms. The median incubation time for this illness is 3 hours, and it lasts several hours to a few days.326 Most NSP outbreaks have occurred on the Gulf of Mexico, west coast of Florida, coastal Texas, North Carolina, and New Zealand.326,434
Unlike other shellfish poisons, NSP can cause a respiratory irritation syndrome. When large blooms of P. brevis occur near the shoreline, wind and wave action can aerosolize the toxin; if sea breezes blow the aerosolized toxin onshore, rapidly reversible conjunctivitis, rhinorrhea, and bronchospasm with nonproductive cough can occur in sensitive individuals.214 Severe respiratory distress is uncommon. The effects are similar to those of muscarinic stimulation.
P. brevis produces at least 10 toxins, known as brevetoxins.23,24 Brevetoxins (designated PbTx-1 to PbTx-10) are potent, lipid-soluble, cyclic polyether compounds that bind to and modulate voltage-gated sodium channel activity. Brevetoxins produce acute neuronal injury and death in rat cerebellar neurons.37 In a canine model, brevetoxins produce depolarization of tracheal and bronchial smooth muscle.383 Intratracheal brevetoxin instillation in rats resulted in systemic distribution of brevetoxin, which suggests that the initial respiratory irritation and bronchoconstriction may be only part of the toxicologic syndrome with brevetoxin inhalation.34
Brevetoxins are potent ichthyotoxins associated with large numbers of dead birds, fish, and mammals. In 1996, 149 manatees died along the southwest Florida coast; brevetoxin was implicated as the primary cause of the epizootic.50 Signs and symptoms of intoxication in fish include violent twisting and corkscrew swimming, defecation and regurgitation, pectoral fin paralysis, caudal fin curvature, loss of equilibrium, quiescence, vasodilation, convulsions, and fatal respiratory failure.24 An enzyme immunoassay, based on antibodies to PbTx-3, has been developed to detect these brevetoxins.476,515 A micellar electrokinetic capillary chromatography (MEKC) detection method allows measurement of brevetoxin at trace levels and is 100-fold better than previous chromatographic or electrophoretic methods.418
Diarrhetic Shellfish Illness
Diarrhetic shellfish poisoning is a rapid-onset illness with gastrointestinal symptoms, which although they are typically severe, are self-limited. Ingestion of shellfish contaminated with dinoflagellates belonging to the genus Dinophysis (Dinophysis fortii, Dinophysis acuminata, Dinophysis norvegica, and Dinophysis acuta) or Prorocentrum (P. lima and Prorocentrum minimum) causes diarrhetic shellfish poisoning (DSP). Lipid-soluble toxins accumulate in shellfish fatty tissues and the hepatopancreas of mussels. They exert their effects mainly on the human small intestine, leading to diarrhea and degenerative changes of the absorptive epithelium.309,488 Symptoms include rapid onset (30 minutes to 2 hours) of diarrhea, nausea, vomiting, abdominal pain, and chills. Rarely, symptoms are delayed up to 12 hours. The syndrome is self-limited and resolves after 2 to 3 days. From 1976 to 1982, DSP was diagnosed in at least 1300 persons in Japan. The period of greatest toxicity appears to be May to August. In 1981, more than 5000 cases were reported in Spain.528 Other outbreaks have occurred in The Netherlands and Chile.196 In 1993, a particularly bad episode occurred in Spain with unusual symptoms; analyses revealed a complex toxin profile with both PSP and DSP toxins present.162
DSP toxins include okadaic acid (OA), OA diolester, dinophysistoxins (DTX-1 to DTX-4), and pectenotoxins.3,306,486,511,528 OA was first isolated from a sponge (Halichondria okadai) in the Pacific.452 It is a specific and potent inhibitor of protein synthesis and inhibits phosphatases A1 and A2 in vitro. OA induces diarrhea because it increases phosphorylation of proteins, which either controls sodium secretion of intestinal cells or influences permeability of cell membranes.99,121 It is a potent tumor promoter in mouse cells and can act as a genotoxin.146 Other DSP toxins exert various effects in experimental animals: pectenotoxins induce liver necrosis, and yessotoxins (from the Japanese scallop Patinopecten yessoensis) induce intracytoplasmic edema in cardiac muscle.465,467 Minimal doses of OA and DTX-1 necessary to cause DSP symptoms are 40 mg and 36 mg, respectively.198 Metals (e.g., aluminum, copper, lead, mercury, cadmium) in concentration at or below acceptable levels in mussels synergistically increase cytotoxicity of low concentrations of OA in cultured cells.477
Increasing incidents of phytoplankton blooms with a danger of toxin release have necessitated the search for new diagnostic methods that can detect toxin quickly and reliably. A variety of techniques, including a radioimmunoassay using antibodies raised in rabbits, a competitive ELISA, idiotypic anti-idiotypic competitive immunoassay, rapid tissue culture assays, and cytotoxicity assays, can identify the presence of OA.91,103,283,419,482 A unified bioscreen for detection of diarrhetic shellfish toxins and microcystins (as from blooms of the cyanobacteria Microcystis aeruginosa) uses capillary electrophoresis coupled with a liquid chromatography–linked protein phosphatase bioassay.47 A protein phosphatase A2 inhibition assay has been shown to be rapid, accurate, and reproducible; it can detect concentrations as low as 0.063 ng/mL in aqueous solutions and 2 ng/g in mussel digestive glands.481 The Japanese quarantine standard is 200 ng of OA per gram of shellfish tissue. Four times this amount of toxin has been identified in northeastern Pacific Ocean mussels. Okadaic acid and related toxins are potent tumor-growth promotors and immunosuppressants in animals, but the effect of exposure in humans is unknown.110
Amnestic Shellfish Poisoning
Domoic acid is produced in nature by the phytoplankton algae Pseudonitschia spp., which are widely distributed across the world.266 Domoic acid, the toxin responsible for amnestic shellfish poisoning (ASP), is an excitatory neurotransmitter first described in Japan in 1958 and isolated from the red algae Chondria armata.457 The first documented human outbreak of poisoning with this compound was in 1987 from Prince Edward Island, Canada, when more than 150 people became ill after ingesting cultured blue mussels, Mytilus edulis, later found to be contaminated with domoic acid (DA).232,363,463,521 Four of these individuals died, and the clinical description of persistent memory impairment in many survivors prompted the nickname of amnestic shellfish poisoning.149 The source of the toxin in these cases was found to be Nitzschia pungens, a diatom that had been ingested by the mussels before humans ate them.30,447 The mussels concentrate the toxin in the hepatopancreas.
Epidemics of domoic acid poisoning have been prominent in other marine life, especially sea birds.48,504,518 A large number of dead and distressed pelicans and cormorants were noted in Monterey Bay, California, in September 1991.518,519 Autopsies performed on the dead birds demonstrated they had consumed large quantities of anchovies from the bay. Subsequent testing showed the anchovies contained high levels of domoic acid. This was the first report documenting the presence of domoic acid in the United States. Water samples taken in the area identified significant quantities of the diatom Pseudonitzschia australis, which when grown in a laboratory environment were able to produce domoic acid.164,518 Three species of Pseudonitzschia are now known to produce domoic acid.
Domoic acid has also been detected in Gulf shellfish (Gulf Coast oyster, Crassostrea virginica) and phytoplankton in the Gulf of Mexico, although no outbreaks of amnestic shellfish poisoning have been recorded in this region. The toxic N. pungens forma multiseries has also been confirmed in Korea, Japan, Oslofjord, Scandinavia, the northeastern and northwestern United States, eastern and western Canada, and eastern South America.123
In the fall of 1991, the latest reported epidemic of domoic acid poisoning occurred in Washington State.251 More than 20 people who consumed razor clams were affected. Subsequent testing confirmed the presence of domoic acid in razor clams along the coasts of both Washington State and Oregon, although mussels tested in these areas were virtually free of toxin. Dungeness crabs collected from these waters were also found contaminated with domoic acid. Many contaminated filter-feeding marine organisms such as shellfish and finfish have been identified as DA vectors. However, in terms of human health risks, species such as market squid, scallops, mussels, and razor clams are of most concern because of their demand by the seafood-consuming public.
Pathophysiology
Domoic acid was first isolated in 1958 following investigations on the antihelmintic and insecticidal activity of seaweed extracts. After the 1987 epidemic of neurotoxic illness in Price Edward Island, Canada, significant evaluation of the surviving victims was undertaken. Chemical analysis at various laboratories ruled out all other known toxic causes of the symptoms displayed by patients.521 Intraperitoneal injection of extracts of implicated mussels into mice produced a syndrome characterized by reproducible scratching followed eventually by death.363,463 The toxin was finally identified as domoic acid.
Domoic acid is a water-soluble, excitatory neurotransmitter and a glutamate receptor agonist. It is structurally related to kainic acid, a potent neurotoxic amino acid.351,408,463,521 This group of compounds is excitatory and acts on three types of receptors in the central nervous system (CNS), with those in the hippocampus being the most sensitive. Domoic acid seems to work by activating kainate receptors in the brain more potently than does kainic acid itself. The result of this stimulation is extensive damage to the hippocampus in victims of the poisoning, as well as less severe injury to portions of the thalamic and forebrain regions.312,387,463 There may also be non-N-methyl-D-aspartate (NMDA) mediated mechanisms.459
It was estimated that the mussels implicated in the Canadian outbreak of ASP contained a total amount of domoic acid in excess of 6 kg, with most being concentrated in the digestive glands.178,521 Other organisms known to produce domoic acid include the phytoplankton Alsidium corallinum and C. armata. Subsequent research suggests that other phytoplankton, such as Amphora coffeaeformis, can also produce domoic acid. Scientists continue to monitor shellfish and marine microorganisms to determine the presence of other sources. There are 10 isomers of DA identified to date; however, some of these have significantly lower toxicity than does the parent compound.279 Domoic acid is relatively stable and does not degrade at room temperature. Also, cooking will not increase the safety of the shellfish product if contaminated with DA.311 There is wide variation in tissue distribution and retention of DA; for example, razor clams have been shown to retain DA for up to a year and contain DA throughout all tissues, whereas a majority of the toxin is confined to the viscera in mussels and fish.279
Clinical Presentation
As a result of the Prince Edward Island event, numerous laboratory-based toxicity studies were performed in order to characterize the toxicity of DA. Multiple regimens that have been investigated include intraperitoneal, intravenous, intraarterial, intrauterine, and oral dosing and direct brain injections, making a direct comparison of DA toxicity between species difficult. Studies have been performed in monkeys, mice, rats, birds, and fish. The most notable clinical signs of toxicity include scratching and seizures in rodents, vomiting in monkeys, spiral-swimming in fish, and tremors and scratching behavior in birds.279,363,335
Humans involved in the Canadian epidemic of amnestic shellfish poisoning had initial symptoms of nausea, vomiting, abdominal cramps, and diarrhea 1 to 24 hours after ingestion.363,463 Neurologic symptoms initiated with memory loss began within 48 hours after ingestion and progressed in some victims to seizures, hemiparesis, ophthalmoplegia, and coma. Some victims displayed purposeless grimacing and chewing. Follow-up neuropsychological testing on affected patients displayed predominantly an anterograde memory disorder, with most other cognitive functions preserved.363 The most severely affected individuals also had some retrograde amnesia. Labile blood pressure and cardiac dysrhythmias were recorded in a few individuals, suggesting DA may be cardiotoxic.371 Elevations in blood urea nitrogen (BUN) and creatine phosphokinase were also noted in many victims and have been recorded in animals suffering DA poisoning, possibly resulting from exertional myopathies or tremors.363,519
The onset of symptoms in victims of the Prince Edward Island epidemic ranged from 15 minutes to 38 hours, with the average approaching 5 hours.363,463 Increased age was identified as a risk factor for both the severity of illness and memory loss. Males were found to be more susceptible.371 Most fatalities occurred in the oldest victims, with postmortem findings suggesting neuronal loss or necrosis, accompanied by astrocytosis.363 The most severe damage was to the hippocampus and amygdala, which are areas of the brain participating in memory functions. Lesions were also noted in the claustrum and the septal and olfactory regions. Retinal lesions have also been reported.371 No lesions were found in the motor nuclei of the brainstem. Hippocampal lesions in victims at autopsy resembled those seen in the brains of animals injected with kainic acid.363,312,432 A follow-up study on patients from the Montreal area suggested that bronchial secretions became so profuse in the hours after mussel ingestion that one-half of the severely affected individuals required endotracheal intubation.363 Pupillary dilation or constriction, and piloerection were also common findings. Approximately 10% of the involved patients demonstrated either persistent memory loss or other neuropathies. Of patients exhibiting neurologic toxicity, maximal effects were noted within the first 3 days after mussel ingestion, and maximal improvement in neurotoxicity occurred in 24 hours to 12 weeks after ingestion. Four and 6 months postexposure, several patients had distal atrophy with weakness of the extremities and hyporeflexia. Electromyography findings were consistent with an acute nonprogressive neuronopathy involving anterior horn cells or diffuse axonopathy predominantly affecting motor axons.371
Treatment
As with most other shellfish toxins, no antidote exists for amnestic shellfish poisoning. Based on the alleged mechanism of action of both domoic and kainic acid, it is possible that benzodiazepines may be beneficial in controlling some of the excessive hippocampal activity and seizures.351,519 Animal studies have suggested a lowered mortality in groups in which benzodiazepines are used after domoic acid exposure. There may also be a role of NMDA antagonists.38
Prevention
Many regulatory agencies worldwide have established biotoxin monitoring programs. Although monitoring programs have been effective at preventing human toxicity, chronic DA toxicity has been characterized in other mammalian species such as sea lions.279 To protect seafood consumers, authorities have established an action limit for DA of 20 mcg DA/g shellfish tissue. This is based on retrospective estimations of DA concentrations of 200 mcg DA/g mussel, which caused illness during the ASP outbreak and incorporates a safety factor of 10. This regulatory limit has been adopted by the United States, European Union, New Zealand, and Australia. Levels exceeding this limit trigger closure of the affected beaches and shellfish harvesting areas.279
Possible Estuary-Associated Syndrome
Pfiesteria piscicida is a toxic dinoflagellate that inhabits estuarine and coastal waters of the eastern United States and has been associated with fish kills and a human illness that has been labeled possible estuary-associated syndrome (PEAS). Since 1991, P. piscicida and other Pfiesteria-like species have been implicated in massive fish kills in estuaries of North Carolina, Maryland, and the Chesapeake Bay.175,180,423 P. piscicida is responsible for a fish disease formally known as ulcerative mycosis. Pfiesteria is primarily a benthic organism but can exist in at least 24 different life stages. Fish swimming into an area with Pfiesteria may be exposed to a toxin that is produced by the dinoflagellate. These fish develop characteristic ulcerative lesions and erratic swimming behavior. Pfiesteria have now been found in coastal waterways extending from Delaware to the Gulf Coast of Alabama.
Although it is not associated with seafood ingestion, PEAS is associated with seafood contact. The first report of adverse health effects in humans was described after an accidental laboratory exposure; investigators working with Pfiesteria developed respiratory and eye irritation, skin rashes, and cognitive and personality changes.175 During the 1990s, commercial fishermen who were exposed to waterways with Pfiesteria species reported similar symptoms.180,182,183,423 The route of exposure is unknown, although it is thought to be either by prolonged direct skin contact with toxin-laden water or via aerosols after breathing the air over areas where fish are dying from toxic Pfiesteria.
Individuals with high exposure complain of headache, skin lesions, skin burning on contact with water, eye irritation, upper respiratory tract irritation, muscle cramps, and neuropsychological symptoms, including increased forgetfulness and difficulties with learning and higher cognitive function.182 No consistent physical findings or laboratory abnormalities have been found. When skin lesions appear, they are erythematous, edematous papules on the trunk or extremities and resolve within a few days to a week after exposure. Thorough neuropsychological testing has documented deficits in higher cognitive function and learning and functional memory.182 The severity of the cognitive dysfunction was directly related to the degree of exposure. The exact nature of the neurocognitive deficit is unknown; however, rats exposed to water containing Pfiesteria toxins have shown significant learning impairments.281,282 Deficits may be expected to improve significantly within 3 to 6 months after cessation of exposure to affected waters.451 The natural history of PEAS is improvement in most symptoms without treatment; however, cholestyramine has been successfully used in patients with persistent symptoms.424 The clinical improvement seen in cases treated with cholestyramine may be due to interuption of enterohepatic circulation of the toxin, although this hypothesis has not been confirmed.425
Diagnosis of PEAS is difficult because the specific causal toxins have not yet been identified, and a biomarker of exposure has not been developed. Current recommendations for diagnosis include (1) development of symptoms within 2 weeks after exposure to estuarine water, (2) memory loss or confusion of any duration, or three or more symptoms from the complex as described in the preceding paragraph, and (3) no other cause for symptoms identified.76 A multiplex PCR is being developed for rapid identification of P. piscicida and other toxic Pfiesteria species.323 PEAS is not infectious and has not been associated with eating fish or shellfish caught in waters where P. piscicida has been found. Brief, direct water contact, including swimming, has not been associated with symptoms. No deaths have been associated with exposure to Pfiesteria species. People should avoid areas with large numbers of diseased, dying, or dead fish.
Haff Disease
Haff disease is a syndrome characterized by severe muscle pain and rhabdomyolysis after consuming fish. It was first described in 1924 around the shores of Königsberg Haff, a bay on the Baltic Sea.538 Further outbreaks have occurred in Sweden, Russia, and Brazil.36,127,426,435 Twenty-three cases in total have been reported in the United States, most associated with eating buffalo fish (Ictiobus cyprinellus) or crawfish, bottom-feeding species found in the Mississippi River and its tributaries. Two cases have been associated with ingestion of a salmon meal.272 Haff disease is most likely the result of a heat-stable toxin in blue-green algae that is eaten by fish; however, the toxin is currently unidentified.75
Haff disease manifests as generalized muscle pain and tenderness, rigidity, weakness, and rhabdomyolysis. Tachycardia, hypertension, tachypnea, and a drop in temperature can also occur. Elevated serum creatine kinase occurs with leukocytosis, myoglobinuria, and elevation of lactate dehydrogenase and other muscle enzymes. Symptoms generally appear approximately 18 hours after eating fish (range, 6 to 21 hours).75 Pathologically, there is neuromyodystrophy with necrosis in motor neurons of the brain and spine, coagulation necrosis of muscle, and myoglobinuric nephrosis. Treatment includes large volumes of intravenous fluids and diuretics to prevent renal failure from myoglobin toxicity. Diagnosis is based on clinical presentation, laboratory data, and food history.
Blue-Green Algae
Blue-green algae are worldwide freshwater cyanobacteria that may proliferate rapidly in a bloom, discoloring the surface of the water and spoiling its odor and taste. Terrestrial, fresh, brackish, and sea-water cyanobacteria produce toxins that are acute and chronic hazards to human and animal health and are responsible for isolated, sporadic animal fatalities each year. Typical algal species include M. aeruginosa, Anabaena flos-aquae, Nodularia spumigena, Nostoc, Oscillatoria agardhii, and Aphanizomenon flos-aquae.98,139,336,394
During conditions of a bloom (warm stagnant water, frequently enhanced by phosphorus and nitrogen fertilizers), the toxins are concentrated enough to become a significant hazard to wild and domestic animals and have been responsible for the death of livestock and dogs.98,135,202,338,489 In most species of toxic cyanobacteria, the toxins are cyclic heptapeptides called microcystins, or cyanoginosins. More than 60 cyanobacterial toxins have been isolated from blue-green algae.98,430 The toxins are of multiple configurations and include alkaloids, polypeptides, and lipopolysaccharides (endotoxins).440
Anatoxin-a and homoanatoxin-a are potent nicotinic agonists that act as postsynaptic, depolarizing neuromuscular blocking agents. Along with saxitoxin, these toxins cause animals to collapse quickly from neuromuscular paralysis, with features of staggering, muscle fasciculations, gasping, and convulsions.201 Anatoxin-a(s) (“second” anatoxin-a) is an anticholinesterase that causes demonstrable cholinergic toxicity in animals.67,201 Anatoxin-a and anatoxin-a(s) are both derived from Anabaena flos-aquae. Nodularins and microcystins cause hepatotoxicosis. Cylindrospermopsin is a protein synthesis inhibitor and induces necrotic tissue injury of multiple organs. Cyanobacterial lipopolysaccharide endotoxins are responsible for gastroenteritis and skin irritations.98 In mice, administration of microcystin-LR causes rapid hepatocellular necrosis with hemorrhagic shock.107,469
Human exposure to blue-green algae blooms has resulted in allergic reactions, skin irritations, gastroenteritis, pulmonary consolidation, and liver damage.98,364 A person who swims through a bloom may suffer local effects, such as conjunctivitis, facial swelling, or papulovesicular dermatitis. Ingestion of contaminated water causes dysenteric diarrhea, with green slimy stools. This may be associated with elevation of γ-glutamyl-transpeptidase and alanine aminotransferase levels. Inhalation of toxins is a probable exposure route; microcystin-LR and anatoxin-a cause significant toxicity in mice via intranasal aerosol exposure.149 In 1996, more than 50 people with associated liver damage died at a hemodialysis clinic in Brazil. Microcystins are thought to have been present in the water used for hemodialysis.98,130
Azaspiracid Shellfish Poisoning (AZP)
Azaspiracid poisoning (AZP) was first described in 1995 in the Netherlands after an outbreak of severe vomiting and diarrhea from ingestion of mussels from Ireland. Although the symptoms were typical of diarrhetic shellfish poisoning (DSP), concentrations of DSP toxins in these shellfish were found to be very low. Therefore, an alternate, and in this case novel, causative agent was sought.484 The toxin was originally named “Killary-toxin” based on the origin of these shellfish from Killary Harbour, Ireland. This unique toxin was later renamed to azaspiracid (AZA) based on its chemical structure. Over the last decade, several analogues of this structurally distinct, heat-stable marine toxin have been identified. Shellfish contaminated with azaspiracids have been document in several European countries, and recently in the United States.254
Pathophysiology
The producing organism was originally thought to be Protoperidinium crassipes. However, it is now known to be produced by the small dinoflagellate Azadinium spinosum.239 Limited availability of the pure toxins has impeded the necessary investigations of AZP. Initially, AZA1 was isolated from the Killary mussels. Investigations have shown that AZA1 is cytotoxic to many cell types, including liver, lung, pancreas, thymus, spleen, and especially small intestine. These effects are time and concentration dependent.484 There has been identification of several analogs of AZA. Some studies indicate that AZAs might have different targets. For example, AZA4 inhibits plasma membrane calcium channels.158
Clinical Presentation
The symptoms of AZP appear within hours of ingestion and include nausea, vomiting, severe diarrhea, and stomach cramps. The illness persists for 2 to 3 days. To date, no long-term effects have been reported.484 Most information regarding AZA toxicology has been obtained from in vitro and in vivo experiments. Mice injected with low doses of AZA developed slowly progressive paralysis, difficulty breathing, and listlessness. Large oral doses in mice demonstrated widespread organ damage, particularly necrosis in the lamina propria within the small intestine.158 AZP remains a rare illness, although it is likely that there is underreporting because of the short duration and benign coarse of illness.
Diagnosis
Levels of AZA vary significantly among mussels harvested from a given region. The European Commission regulatory limit is 0.16 mg/kg shellfish. Previous reports have determined the presence of AZA by liquid chromatography–mass spectrometry/mass spectrometry.254 Other detection methods, such as ELISA, have been developed for AZA but are not commercially available.484
Prevention
Several incidents of human intoxication were the impetus for implementation of a national surveillance program that monitors weekly the levels of AZA in shellfish from all production areas in Ireland. There have since been no further reports of AZP incidents associated with Irish shellfish. In 2008, an outbreak occurred in France and Ireland following accidental dispatch to consumers of AZA-contaminated shellfish that were held in quarantine following AZA confirmation.158
Yessotoxin (YTX)
Yessotoxins (YTX) were first isolated in 1986 from the Japanese scallop P. yessoensis and Norwegian mussels. They have since been observed in several countries, including New Zealand, Chile, Italy, Spain, the United Kingdom, and Canada.7 Recently, YTX has been identified in French shellfish originating from the Mediterranean.7 Yessotoxin and its analogues are produced by the dinoflagellates Protoceratium reticulatum, Lingulodinium polyedrum, and Gonyaulax spinifera.480,483 YTX and its analogues were initially included in the diarrhetic shellfish poisoning (DSP) toxins group. However, they have recently been classified and regulated separately, because they do not share the same mechanism of action and only have been shown to be toxic to mice by intraperitoneal injection.480,483 Similar to other marine toxins, the principal vectors for YTXs are scallops and mussels, which can accumulate large quantities of YTX, particularly in the hepatopancreas, because of their filter feeding nature.
More than 100 YTX analogs have been reported from shellfish and microalgae, although the structures of only about 40 of them have been identified. Although no reports of human poisoning induced by yessotoxins have been recorded, YTX-contaminated shellfish have been reported worldwide.357 In a mouse model, intraperitoneal injection of lethal doses of YTX or homoYTX caused symptoms similar to those of paralytic shellfish poisoning, with restlessness, dyspnea, shivering, jumping, and/or cramps.21 Several studies have demonstrated a range of median lethal dose values (LD50) from 80 to 750 mcg/mL.480 The target organ of YTX appears to be the cardiac muscle, where ultrastructural changes in mitochondria and myofibrils have been demonstrated.480 Other YTX analogs cause fatty degeneration of liver and pancreas. Oral administration in mice does not seem to cause behavioral change or death. However, changes in the cardiac muscle were observed with repeated oral dosing. These changes resolved by 90 days.483 Although the mechanism of action of YTX remains to be elucidated, it appears to exert a modest indirect effect on calcium channels.480
Due to the high number of existing analogues of YTX, methods of detection and quantification are complex. Mouse bioassay is the official method accepted to detect YTXs. However, it is time consuming and expensive, and lacks specificity.357 Several other methods of detection available include functional assays, structural assays, and chemical methods. However, some of these methods have not been validated and the gold standard for detection has yet to be determined.
Other Shellfish and Invertebrate Poisonings
Callistin Shellfish Poisoning
The Japanese Callista clam (Callista brevisiphonata) is toxic during the spawning months of May to September, at which time cholinergic compounds in the ovaries are increased. The intoxication resembles cholinergic crisis, with both muscarinic and nicotinic components. Within an hour of ingestion of the heat-stable toxin, patients may experience generalized pruritus, urticaria, erythema, facial numbness and paralysis, hypersalivation, diaphoresis, fever, chills, nausea, vomiting, diarrhea, bronchorrhea, bronchospasm, and constrictive dyspnea.25 Therapy is supportive, and recovery is usually complete within 2 days. In severe cases of cholinergic crisis, particularly with marked bradycardia, atropine (0.5 mg or more intravenously every 5 minutes, titrated to dry secretions, with adequate ventilation) may be administered.
Venerupin Shellfish Poisoning
The Japanese lake-harvested oyster (Crassostrea gigas) and clam (Tapes semidecussata) occasionally feed on toxic dinoflagellate species of the genus Prorocentrum, posing the greatest risk during the months of December through April.25,195 The heat-stable toxin induces rapid onset of gastrointestinal distress, headache, and nervousness, which are followed more than 48 hours by hepatic dysfunction, manifested by elevation of liver enzymes, leukocytosis, jaundice, and profound coagulation defects. Delirium and coma may ensue, and death occurs in 33% of victims. Therapy is supportive and based on symptoms. Any victim who shows early symptoms of gastroenteritis should be placed on a low-protein diet and monitored for 48 to 72 hours for signs of liver failure. There is not yet clinical experience with exchange transfusion, chemotherapy, hemoperfusion, or liver transplantation in the management of profound liver failure associated with this disorder.
Tridacna Clam Poisoning
Giant clams of the species Tridacna maxima are eaten in French Polynesia.25 This species can cause poisoning characterized by nausea, vomiting, diarrhea, paresthesias, tremor, and ataxia. Severe cases can be fatal. The toxin appears to be concentrated in the mantle and viscera of the clam. Therapy is supportive.
Whelk Poisoning
In Japan, poisoning has followed ingestion of mollusks of the genera Neptunea, Buccinum, and Fusitriton (whelks, or ivory shells). The toxin is located in the salivary glands and has been characterized as tetramine.12 Tetramine (trimethylammonium) is a naturally occurring quaternary ammonium compound that has been identified in anemones, gorgonians, jellyfishes, and mollusks.11 Symptoms include headache, dizziness, nausea, vomiting, blurred vision, and dry mouth. No fatalities have been reported. Therapy is supportive.25
Ivory Shell Poisoning
Human intoxications have followed consumption of the ivory shell Babylonia japonica, which is widely distributed along the coastline of Japan. The toxin, surugatoxin, is located in the midgut of the animal and reputed to be produced by a gram-negative bacterium on which the snail feeds. Surugatoxin and ivory shell toxins appear to have autonomic ganglionic blocking action. Symptoms include abdominal pain, diarrhea, nausea, vomiting, oral paresthesias, syncope, and seizures.196 TTX has also been identified in B. japonica.
Abalone Poisoning
Abalone poisoning follows ingestion of the viscera of certain Japanese abalone (tsunowata, or tochiri), particularly from the Island of Hokkaido, where Haliotis discus and Haliotis sieboldi are found. Symptoms include severe urticaria, erythema, pruritus, edema, and skin ulceration. The reaction appears to be of a photosensitive nature, as the lesions are confined to areas of ultraviolet exposure. The toxin may be derived from chlorophyll contained in the seaweeds on which the abalone feed.25 Therapy is supportive.
Cephalopod Poisoning
In certain areas of Japan, intoxications have resulted from ingestion of squid and octopus. Symptoms develop within 10 to 20 hours and consist of nausea, vomiting, diarrhea, abdominal pain, headache, weakness, paralysis, and seizures. Although most victims recover within 48 hours, deaths have occurred.25 Therapy is supportive.
Sea Hare Poisoning
Sea hares are marine gastropod mollusks prevalent in certain South Pacific waters, including Fiji. Aplysia species have been considered to be toxic since Roman times. Aplysia juliana secretes an antibacterial and antineoplastic protein found in the water-soluble fraction of a fetid secretion lethal to crabs. Human poisoning has been reported after ingestion of Dolabella auricularia (known as “veata” in Fiji).399,438 The symptoms begin approximately 30 minutes after eating and include prickling skin sensation, vomiting, diarrhea, shaking, tremors, fasciculations, arthralgias, dyspnea, visual disorientation, altered sensorium, and fever. The course of illness may exceed a week. It has been suggested that sea hare poisoning in humans might be a form of subacute organobromine intoxication.
Ingestion of the sea hare Aplysia kurodai was associated with acute liver damage with sustained elevations of aminotransferases. Microscopic findings in a liver biopsy specimen revealed characteristic apoptotic hepatocytes accompanied by mitotic hepatocytes. Bioactive substances in the sea hare might induce such apoptosis of hepatocytes in the liver.400
Anemone Poisoning
In the South Pacific, ingestion of the green or brown anemones Radianthus paumotensis or Rhodactis howesii (mata-malu samasama) has been associated with severe illness and death. Accidental deaths generally involve small children, whereas adults may be the unfortunate recipients of improperly cooked anemone or even may be intentionally stricken in acts of suicide. The toxic substances are found in the nematocysts and the tentacles. Anemones have been used for criminal purposes in the South Pacific.25 Physiobranchia douglasi is poisonous eaten raw but is reputedly safe if cooked.196
A toxic protein has been isolated from the sea anemone Urticina piscivora. It is a potent cardiac stimulatory protein and potent hemolysin on erythrocytes of the rat, guinea pig, dog, pig, and human, causing toxicity at concentrations as low as 10−10 M.97
Crab Poisoning
A number of toxins have been isolated from crab species, and there is marked similarity to PSP and TTX poisonings. Saxitoxin, neosaxitoxin, and gonyautoxins have been isolated from crab species in Okinawa and from Eriphia sebana and Atergatis floridus from Australian coral reefs.293–296 TTX and palytoxin have also been characterized from poisonous crabs.6 In Thailand, TTX was responsible for an epidemic involving 71 persons (two died) who ate toxic eggs from the horseshoe crab Carcinoscorpius rotundicauda.241 The poisonous mosaic crab L. pictor from the Indo-West Pacific region has caused several fatalities in the Philippines and Singapore. The toxins were concentrated in the gut and hepatopancreas, whereas the muscle was less toxic. Captive crabs lose toxicity almost completely by 24 days.
Coconut crab (Birgus latro) poisoning is manifested as nausea, vomiting, headache, chills, myalgias, and exhaustion, with occasional deaths. Asiatic horseshoe crabs (C. rotundicauda) are eaten in Thailand, where they cause mimi poisoning. Symptoms include nausea, vomiting, diarrhea, abdominal cramps, dizziness, palpitations, weakness, lower extremity paresthesias, aphonia, perioral burning, pharyngitis, sialorrhea, syncope, paralysis, and death. Again, the toxin appears highly similar to saxitoxin.88
Freshwater crabs are a potential source of human paragonimiasis, a parasitic disease that was prevalent in Asia until the 1960s.92 Paragonimiasis usually causes pulmonary disease with productive cough and bloody sputum. CNS involvement has also been reported.372 The disease is contracted by eating raw crab infected with the metacercariae of Paragonimus species. Areas known to be endemic are Vietnam, China, Japan, Korea, Ecuador, and Liberia.*