Scuba Diving–Related Disorders
The disorders related to scuba diving include those caused by environmental exposure (see Chapters 3 and 50), dysbarism, nitrogen narcosis, contaminated breathing gas, decompression sickness (DCS), and hazardous marine life (see Chapters 52 and 53) (Box 51-1).
Dysbarism
Mask Squeeze
Treatment
1. No treatment is necessary because the manifestations are self-limited.
2. Orbital hemorrhage is a rare complication and is associated with diplopia, proptosis, and visual loss. Prompt referral should be made for magnetic resonance imaging and ophthalmologic care. Recompression therapy is not indicated.
Ear Canal Squeeze
Treatment
1. If a remediable occlusion exists, correct it.
2. If inflammation of the external canal occurs without tympanic membrane rupture, instill eardrops suitable for the treatment of otitis externa (a fluoroquinolone combined with a steroid component) as directed for 2 to 3 days.
3. If the tympanic membrane is perforated, seek otolaryngologic evaluation. Do not allow further diving until the membrane has healed. Instill fluoroquinolone otic drops.
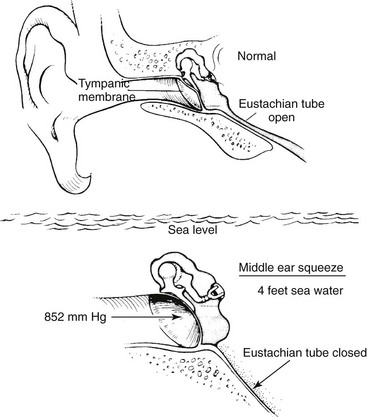
Middle Ear Squeeze (Barotitis Media)
If air cannot enter the middle ear via the (contracted or blocked) eustachian tube during an underwater descent, the existing air in the middle ear space contracts, creating a relative vacuum and pulling the tympanic membrane inward (Fig. 51-1).
Signs and Symptoms
Treatment
1. Before tympanic membrane rupture, administer an oral decongestant and a long-acting topical decongestant nasal spray such as oxymetazoline. In a severe case, if the tympanic membrane is intact, a short course of prednisone (50 mg PO, tapered over 7 days) may be helpful. An antihistamine may be administered if there is an allergic component.
2. Repeated gentle autoinflation of the middle ear by use of the Frenzel maneuver may help to displace any collection of middle ear fluid through the eustachian tube.
3. For tympanic membrane rupture, administer an antibiotic such as amoxicillin/clavulanate for 7 days. In addition, administer fluoroquinolone otic drops. Suspend all diving activities until the tympanic membrane is fully healed or has been surgically repaired and eustachian tube function allows easy autoinflation.
Barosinusitis
Treatment
1. Give oral and topical decongestants (mucosal vasoconstrictors) such as pseudoephedrine and oxymetazoline.
2. Administer an analgesic as appropriate.
3. If an episode of sinus squeeze has occurred, particularly with epistaxis, and the patient subsequently develops symptoms of sinusitis (pain, fever, tenderness over the affected sinus, nasal discharge), administer an appropriate antibiotic such as amoxicillin/clavulanate or azithromycin.
Pulmonary Barotrauma of Ascent (Pulmonary Overpressurization Syndrome)
Signs and Symptoms
1. History of rapid and uncontrolled ascent to the surface before onset of symptoms
2. Pneumomediastinum: gradually increasing hoarseness or “brassy” voice, neck fullness, substernal chest pain several hours after diving
3. Subcutaneous emphysema (crepitus) possible
4. In severe cases, possible chest pain, dyspnea, bloody sputum, dysphagia
Arterial Gas Embolism
Signs and Symptoms
1. Cardiac: chest pain related to myocardial ischemia, arrhythmias, or cardiac arrest
a. Possibly confusing pattern, as showers of bubbles randomly embolize cerebral circulation
b. Manifestations often typical of acute stroke (cerebrovascular accident), although hemiplegia infrequent
c. Most often observed signs: loss of consciousness, monoplegia or asymmetric multiplegia, focal paralysis, paresthesias or other sensory disturbances, convulsions, aphasia, confusion, blindness or other visual field defects, vertigo, dizziness, headache
d. Rare signs: sharply circumscribed areas of glossal pallor
Treatment
1. Transport the patient for recompression treatment in a hyperbaric (oxygen) chamber.
a. If an aircraft is used, do not expose the patient to significant cabin altitude. Ideally the aircraft will be pressurized to sea level.
b. In an unpressurized aircraft, maintain the flying altitude as low as possible, not to exceed 300 m (984.3 ft) above sea level.
2. Maintain the patient in a supine position.
3. Administer oxygen, 5 to 15 L/min, by nonrebreather mask.
4. Begin an intravenous infusion of isotonic solution to maintain urine output at 1 to 2 mL/kg/hr.
5. Obtain help with the treatment of dive-related incidents 24 hours a day by calling the Divers Alert Network at Duke University (919-684-9111).
6. If it is available, administer lidocaine intravenously per protocol as an adjunct to recompression therapy.
Nitrogen Narcosis
Signs and Symptoms
1. Usually becomes apparent at depths between 21 and 31 m (68.9 and 101.7 feet)
2. Light-headedness, loss of fine sensory discrimination, giddiness, euphoria
Contaminated Breathing Gas
The pressurized air within a scuba tank may be contaminated with oil or carbon monoxide.
Decompression Sickness
Signs and Symptoms
1. Symptoms developing in the first hour after surfacing from a dive, with some patients noticing symptoms within 6 hours after diving; rarely, symptoms not noted until 24 to 48 hours after diving
2. Musculoskeletal DCS or “limb bends”: periarticular joint pain most common symptom
a. Shoulders and elbows most often affected
b. Pain usually described as dull ache deep within the affected joint, but also characterized as sharp or throbbing
c. Pain worse with joint movement, or “grating” sensation
d. Vague area of numbness surrounding the affected joint
f. Variably present diagnostic feature: pain temporarily relieved by inflation to 150 to 250 mm Hg of sphygmomanometer cuff placed around the joint
3. Neurologic DCS: back pain, girdling abdominal pain, extremity heaviness or weakness, paresthesias of extremities, anal sphincter weakness or fecal incontinence, loss of bulbocavernosus reflex, bladder distention and urinary retention, paralysis, hyperesthesia or hypoesthesia, paresis, scotomata, headache, dysphagia, confusion, visual field deficit, spotty motor or sensory deficits, disorientation, mental dullness
5. Cutaneous: pruritus, mottling, local or generalized hyperemia, marbled skin (cutis marmorata)
6. “Chokes”: dyspnea, substernal pain made worse on deep inhalation, nonproductive cough, cyanosis, tachypnea, tachycardia
7. Vasomotor DCS: weakness, sweating, unconsciousness, hypotension, tachycardia, pallor, mottling, decreased urine output
Treatment
1. Transport the patient for recompression treatment in a hyperbaric (oxygen) chamber.
2. If an aircraft is used, do not expose the patient to significant cabin altitude. Ideally, the aircraft will be pressurized to sea level.
3. In an unpressurized aircraft, maintain the flying altitude as low as possible, not to exceed 300 m (984.3 feet) above sea level.
4. Maintain the patient in a supine position.
5. Administer oxygen, 5 to 15 L/min, by nonrebreather mask.
6. Begin an intravenous infusion of isotonic solution to maintain urine output at 1 to 2 mL/kg/hr.
7. Obtain help with the treatment of dive-related incidents 24 hours a day by calling the Divers Alert Network at Duke University (919-684-9111).
Flying After Diving
1. Observe a minimum surface interval of 12 hours between the last dive and flying in a commercial jet.
2. Divers who make daily, multiple dives for several days or who make dives that require decompression stops are advised to attempt to attain an interval of at least 18 hours between diving and flying. However, it would seem prudent to extend the interval to 24 hours or longer to minimize the risk for DCS.
Absolute Contraindications for Diving
The following conditions are felt to be absolute contraindications for diving:
2. Acute asthma with abnormal pulmonary function
3. Cystic or cavitary disease of the lungs
4. Obstructive or restrictive lung disease
5. Epilepsy or seizure disorder
7. Symptomatic coronary artery disease
8. Chronic perforated tympanic membrane