Chapter 23 Scrotal Pain
1 Do infants and toddlers get testicular torsion?
Pinto KJ, Noe HN, Jerkins GR: Management of neonatal testicular torsion. J Urol 158:1196–1197, 1997.
2 What are some of the important factors in the patient’s history that suggest testicular torsion?
Kamaledeen S, Surana R: Intermittent testicular pain: Fix the testes. BJU Int 91:406–408, 2003.
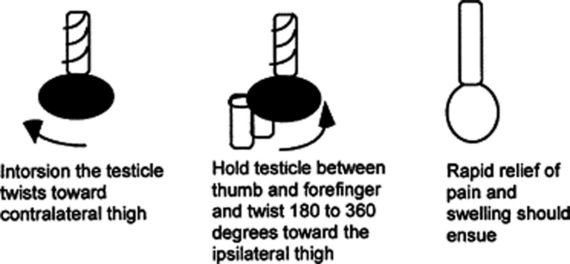
4 What is manual detorsion?
In general, the prognosis is excellent if the testis is detorsed within 3 hours of symptom onset. Manual detorsion in the emergency setting can allow the testicle to remain viable until emergency surgery can be performed. Although the testicle can twist in either direction, it more commonly twists medially, toward the contralateral thigh. In the manual detorsion procedure, one holds the affected testicle between thumb and forefinger and untwists 360 degrees toward the ipsilateral thigh (Fig. 23-1). If relief is noted, the testicle should be rotated another 360° or more, since the usual twist is 720°. The direction can be reversed if more pain or swelling occurs after the initial maneuver. The trick is not to be shy or reserved while performing this procedure; it will hurt while it is being done, but if done correctly will greatly relieve symptoms almost immediately. Sedation and analgesia may be warranted to facilitate the detorsion procedure. Surgical correction (bilateral orchiopexy) is still necessary after this maneuver; however, the emergency detorsion procedure can help salvage the affected testicle.
Cattolica EV: Preoperative manual detorsion of the torsed spermatic cord. J Urol 133:803–805, 1985.
6 What is torsion of the appendix testis?
8 Are there any rare entities causing scrotal pain or swelling that would be impressive to mention on rounds?
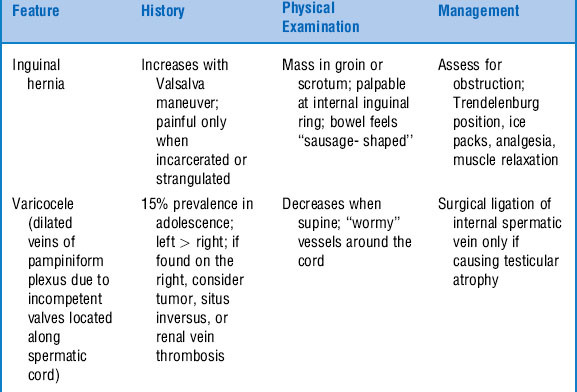
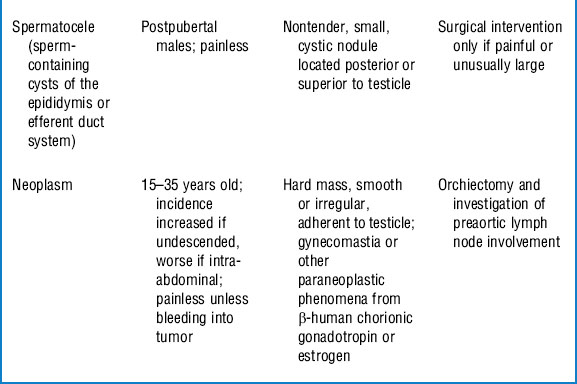
9 How can I differentiate among the variety of painless scrotal masses?
The most common painless scrotal masses are inguinal hernia, hydrocele, varicocele, spermatocele, and testicular tumor. Table 23-1 describes the features of each of these entities.
Skoog SJ: Benign and malignant pediatric scrotal masses. Pediatr Clin North Am 44:1229-1250, 1997.