43 Sciatic Nerve Block
Proximal sciatic nerve block is a versatile regional anesthetic for lower extremity surgery. It is usually combined with femoral nerve block for more complete anesthesia of the leg. The sciatic nerve (L4 to S3) is the largest nerve in the body, with a transverse diameter of more than 17 mm on ultrasound scans.1 However, despite its large size, the sciatic nerve can be difficult to visualize in the gluteal region and proximal thigh. Sonographic features of the regional anatomy are essential to identifying the nerve.
Suggested Technique
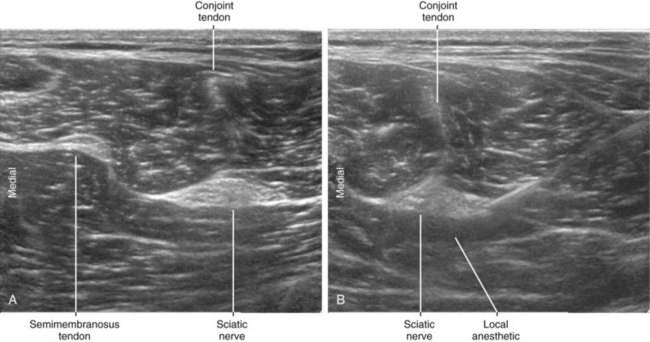
Anatomic variation of the sciatic nerve in the subgluteal region primarily consists of identification of separate contributions from the common peroneal and tibial nerves.2,3 This indicates proximal division of the sciatic nerve by the piriformis muscle. If the anomaly is correctly identified, multiple-injection technique guided by ultrasound provides complete sciatic block.
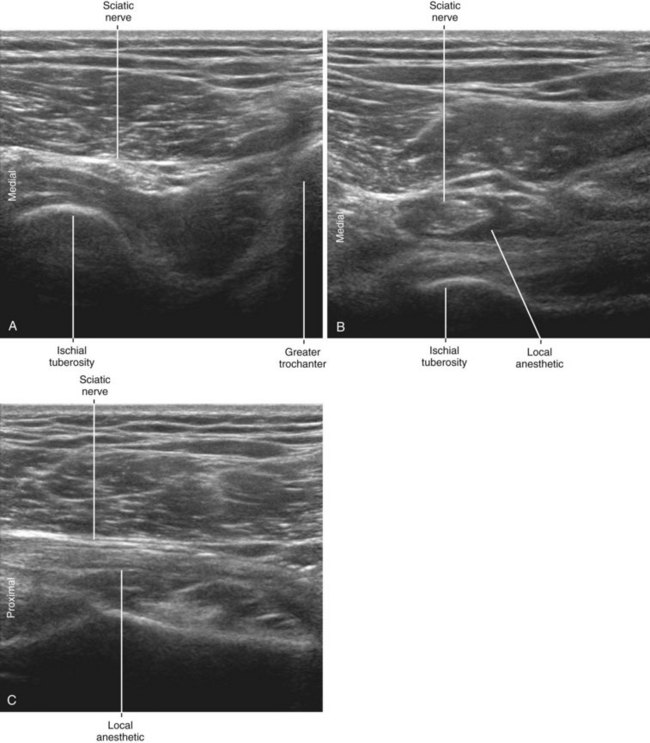
The sciatic nerve lies between the greater trochanter (lateral) and the ischial tuberosity (medial). These bony reference points are useful proximal landmarks for sciatic block in the gluteal region.4 In some patients the inferior gluteal artery can be identified on the medial side of the proximal sciatic nerve.
Key Points
| Sciatic Nerve Block (Subgluteal) | The Essentials |
|---|---|
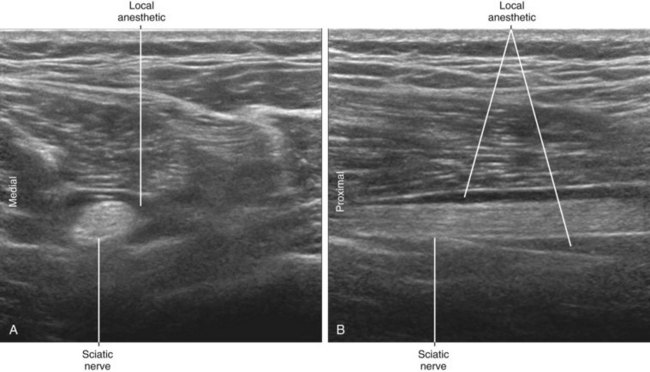
| Anatomy | The PAs run over the anterior side of the SN (the AM side). The conjoint ST-Bc tendon points to the medial side of the SN. The SM tendon lies medial to the SN. The SN is about 6 by 18 mm in diameter. |
| Image orientation | The SN lies lateral to the ischiocrural tendons. |
| Positioning | Lateral |
| Operator | Standing on the side of the patient |
| Display | Across the table |
| Transducer | Medium-frequency linear, 50-mm footprint |
| Initial depth setting | 40 to 60 mm |
| Needle | 20 to 21 gauge, 70 to 90 mm in length |
| Anatomic location | Begin by scanning the subgluteal region near posterior midline. If imaging is difficult, can trace SN proximally from popliteal fossa. |
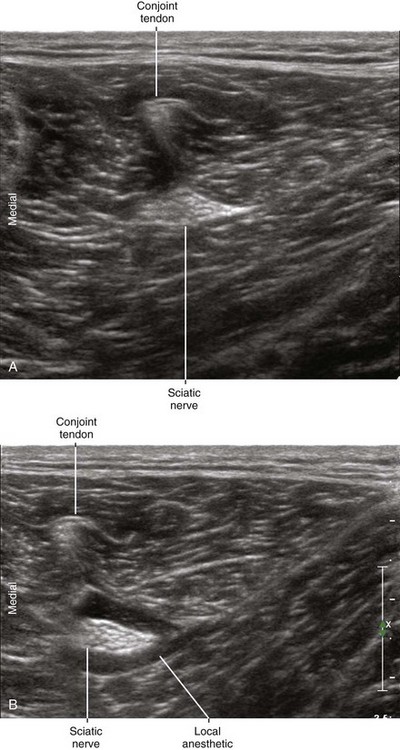
| Approach | SAX view of SN, in-plane from the lateral side Place the needle tip between the SN and PA. |
| Sonographic assessment | The injection should track along the SN (LAX). |
| Anatomic variation | Proximal division of SN by the piriformis muscle (5%-10%) This may require separate injections. Different nerve morphologies (commonly oval or triangular shape) |
Clinical Pearls
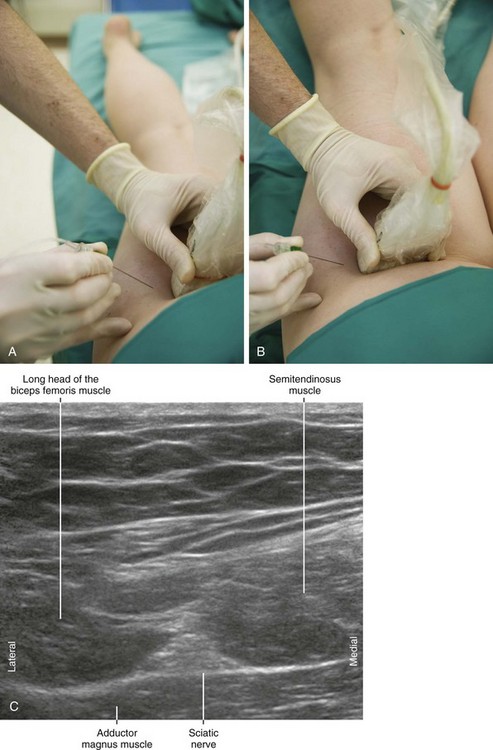
• A number of patient positions can be used to approach proximal sciatic nerve block. Prone position is favored because of the stable imaging for in-plane technique from the lateral aspect of the thigh. Another relatively easy alternative is the lateral position with a hip bump to provide stability.
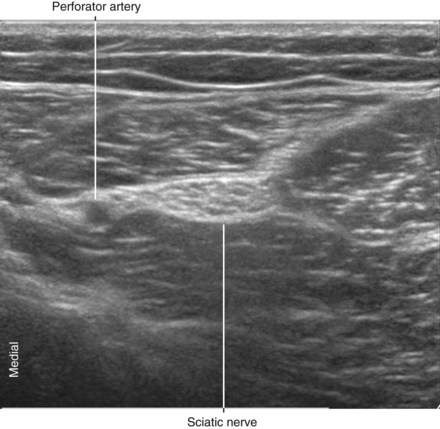
• When an accompanying artery is identified on the lateral side of the sciatic nerve, place the needle tip in the connective tissue between the nerve and the artery. This may require puncturing the connective tissue with the block needle and slowly injecting as the needle is withdrawn to identify the correct layer surrounding the nerve.
• The fascia surrounding the sciatic nerve in the subgluteal region is thick. This emphasizes the importance of correct needle tip positioning and local anesthetic distribution.
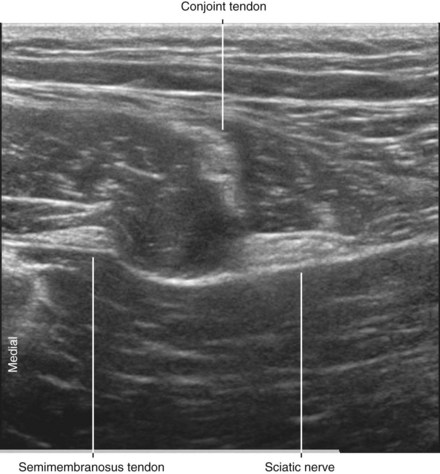
• The sciatic nerve lies lateral to the tendon of the semimembranosus muscle. The conjoint tendon of the biceps femoris and semitendinosus points to the medial aspect of the sciatic nerve because the nerve lies in the crease between these two muscles.5 Perforating arteries usually can be seen crossing the anterior side of the sciatic nerve through the intermuscular septum that separates the sciatic nerve from the adductor magnus muscle. Sometimes the sciatic nerve must be traced proximally from its bifurcation in the popliteal fossa.
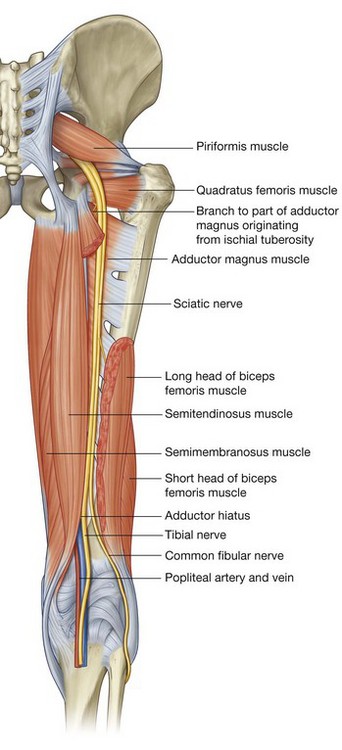
FIGURE 43-1 Course of the sciatic nerve.
(From Drake RL, Vogl W, Mitchell AWM. Gray’s anatomy for students. Philadelphia: Churchill Livingstone; 2004.)
1 Heinemeyer O, Reimers CD. Ultrasound of radial, ulnar, median, and sciatic nerves in healthy subjects and patients with hereditary motor and sensory neuropathies. Ultrasound Med Biol. 1999;25:481–485.
2 Benzon HT, Katz JA, Benzon HA, et al. Piriformis syndrome: anatomic considerations, a new injection technique, and a review of the literature. Anesthesiology. 2003;98:1442–1448.
3 Pokorny D, Jahoda D, Veigl D, et al. Topographic variations of the relationship of the sciatic nerve and the piriformis muscle and its relevance to palsy after total hip arthroplasty. Surg Radiol Anat. 2006;28:88–91.
4 Chan VW, Nova H, Abbas S, et al. Ultrasound examination and localization of the sciatic nerve: a volunteer study. Anesthesiology. 2006;104:309–314.
5 Bruhn J, Moayeri N, Groen GJ, et al. Soft tissue landmark for ultrasound identification of the sciatic nerve in the infragluteal region: the tendon of the long head of the biceps femoris muscle. Acta Anaesthesiol Scand. 2009;53(7):921–925. Epub 2009, Apr 27