Cesarean Scar Defect
Synonyms/Description
Etiology
Ultrasound Findings
Differential Diagnosis
Clinical Aspects and Recommendations
Figures
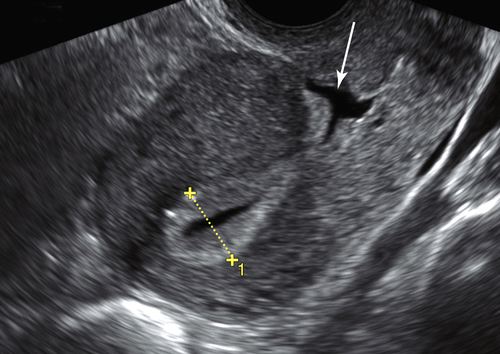
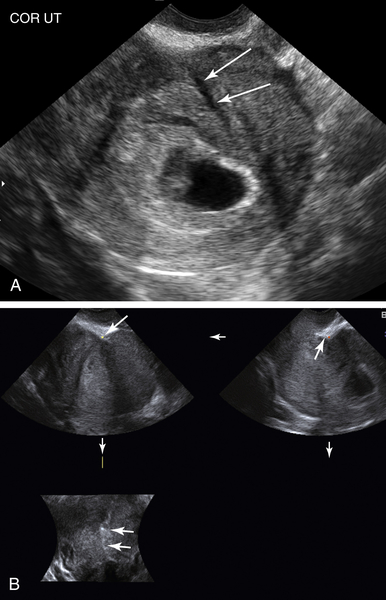
Figure C2-1 Longitudinal view of the normal uterus of a patient with a C-section scar defect. A small amount of fluid outlines the C-section scar defect (arrow) in the anterior lower uterine segment where the C-section scar is located. The niche is formed by the puckering of the anterior wall of the uterus, just above the cervix.
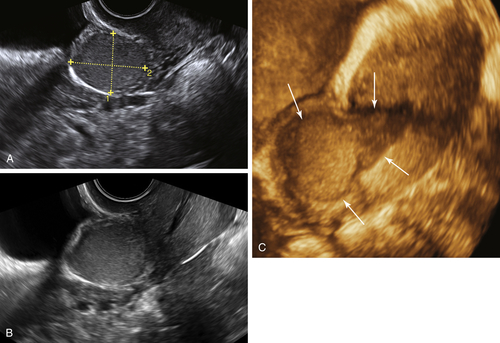
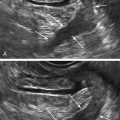
Figure C2-2 Large rounded area of dehiscence of a C-section scar ballooning anteriorly and indenting the bladder. A and B, Two-dimensional views of the lower uterine segment taken obliquely, showing the mass-like defect between the cervix and bladder. The defect (calipers) is filled with low-level echoes indicating unclotted blood. Note the proximity of the defect to the bladder. C, A 3-D longitudinal view of the anterior aspect of the uterus, showing the defect (arrows) originating from the lower uterine segment and bulging anteriorly at the level of the C-section scar.
Suggested Reading
Bujold E., Jastrow N., Simoneau J., Brunet S., Gauthier R.J. Prediction of complete uterine rupture by sonographic evaluation of the lower uterine segment. Am J Obstet Gynecol. 2009;201:320.
Jastrow N., Chaillet N., Roberge S., Morency A.M., Lacasse Y., Bujold E. Sonographic lower uterine segment thickness and risk of uterine scar defect: a systematic review. J Obstet Gynaecol Can. 2010;32:321–327.
Monteagudo A., Carreno C., Timor-Tritsch I.E. Saline infusion sonohysterography in nonpregnant women with previous cesarean delivery: the “niche” in the scar. J Ultrasound Med. 2001;20:1105–1115.
Naji O., Abdallah Y., Bij De Vaate A.J., Smith A., Pexsters A., Stalder C., Mcindoe A., Ghaem-Maghami S. Standardized approach for imaging and measuring Cesarean section scars using ultrasonography. Ultrasound Obstet Gynecol. 2012;39:252–259.
Uppal T., Lanzarone V., Mongelli M. Sonographically detected caesarean section scar defects and menstrual irregularity. J Obstet Gynaecol. 2011;31:413–416.
Vikhareva Osser O., Jokubkiene L., Valentin L. High prevalence of defects in Cesarean section scars at transvaginal ultrasound examination. Ultrasound Obstet Gynecol. 2009;34:90–97.
Vikhareva Osser O., Jokubkiene L., Valentin L. Cesarean section scar defects: agreement between transvaginal sonographic findings with and without saline contrast enhancement. Ultrasound Obstet Gynecol. 2010;35:75–83.
Vikhareva Osser O., Valentin L. Clinical importance of appearance of cesarean hysterotomy scar at transvaginal ultrasonography in nonpregnant women. Obstet Gynecol. 2011;117:525–532.
Wang C.B., Chiu W.W.C., Lee C.Y., Sun Y.L., Lin Y.H., Tseng C.J. Cesarean scar defect: correlation between Cesarean section number, defect size, clinical symptoms and uterine position. Ultrasound Obstet Gynecol. 2009;34:85–89.